Edema nelle fasi avanzate della BPCO: cuore
polmonare cronico o scompenso cardiaco?
Stefano Carlone
Direttore UOC Malattie Apparato Respiratorio
Roma
Caso clinico A
•
•
•
•
•
Paziente di 65 anni, con diagnosi certa di BPCO
Dispnea di 3°-4° grado
Ortopnea – Turgore delle giugulari – Epatomegalia
Edema agli arti inferiori
Insufficienza respiratoria ipossiemica
pO2 48 pCO2 34 mmHg pH 7.47
• PFR = Deficit ventilatorio di tipo misto
• ECG = FA ad alta frequenza – segni di ischemia
antero-laterale
• BNP = 1350 pg/ml
Diagnosi: Scompenso cardiaco congestizio in
cardiopatia dilatativa ischemica in paziente affetto
da BPCO
Caso clinico B
•
•
•
•
•
Paziente di 71 anni con diagnosi certa di BPCO
Dispnea di 4° grado
Turgore delle giugulari – Epatomegalia
Edema agli arti inferiori
Insufficienza respiratoria ipossiemica e ipercapnica
pO2 44 pCO2 78 mmHg pH 7.31
• PFR = Deficit ventilatorio di tipo ostruttivo di grado
severo (VEMS 40% del valore teorico, Indice di
Tiffenau 60%)
• ECG = Tachicardia sinusale, P polmonare
• BNP = 285 pg/ml
Diagnosi: “Cuore polmonare” in paziente
affetto da BPCO
COPD: a multi-component
airway disease
Inflammation
Muco-ciliary
dysfunction
Loss of elastic recoil Airway remodelling
(chronic bronchitis)
(emphysema)
Hyperinflation
Dyspnea
Reduced
exercise
tolerance
Systemic
effects
Eventi cardiovascolari prevalenti nella BPCO
Coronaropatie
15.2%
Aritmie
25-30%
FA e fibrillo-flutter
Extrasistolia sopra e ventricolare
Tachicardia sinusale
Tachiaritmie
Fibrillazione ventricolare
Ipertensione arteriosa
39.6%
Scompenso cardiaco
20%
Ipertensione polmonare
90%
al III stadio
Edema (cuore polmonare)
48%
al III stadio
INDACO Study
Comorbidity prevalence in 547 COPD pts
Cardiovascular
comorbidities
51.3
Metabolic
syndrome
Diabetes
18.7
18,5
22.1
Cardiac
ischemia
12.2
8.4
15.4
Anxiety
Depression
7.3
2.8
Hypertension
Cancers
(All)
Heart failure
Lung cancer
None
Ageing of the population increases the
prevalence of chronic diseases,
including cardiovascular diseases,
cancer, chronic respiratory diseases
and metabolic syndrome in developed
countries with a substantial economic
and social burden. Almost half of all
elderly people (> 65 yrs) have at least
three chronic medical conditions and
one fifth have five or more.
Comorbidities affect health outcomes in COPD
Patients with COPD mainly die of
nonrespiratory diseases such as cardiovascular
diseases (25%), cancer (mainly lung cancer,
20-33%) and other causes (30%).
Respiratory diseases (mainly respiratory
failure due to COPD excerbations) account for
4-35% of deaths.
COPD e CV risk
• In
mild to moderate COPD three times as many hospital
admissions in this patient group are for cardiovascular
than for pulmonary causes.
• In
the Lung Health Study, 25% of deaths were due to
CV disease
• In the TORCH study the proportion was 27%
• In
a systematic review of the literature (>80.000 pts)
reduced FEV1 nearly doubles the risk for CV mortality
independent of confounders as age, smoking, etc
• For
every 10% decrease of FEV1, CV mortality
increased by 28%, and nonfatal coronary event
increased by almost 20%, after adjustments for
confounders as age, sex, smoking status, cholesterol
and hypertension
Sin Proc Am Thor Soc 2005
Anthonisen AJCRCM 2002
COPD is frequently associated with
chronic heart failure (CHF) (> 20%)
and metabolic syndrome (hypertension,
diabetes, dyslipidemia, obesity, insulin
resistance, proinflammatory state
( CRP) and a prothrombotic state
Major risk factors for chronic disease
expecially COPD and CHF:
Cigarette smoking
Obesity
Cigarette smoking is associated with:
•Lung and systemic inflammation
•Systemic oxidative stress
•Marked changes of vasomotor and endothelial
function
•Enhanced circulating concentrations of several
procoagulant factors
Obesity is associated with:
•Insulin resistance
•Oxidative stress
•Increased concentrations of various (adipo)
cytokines and inflammatory markers (CRP)
•Endothelial dysfunction
Eur Respir J 2009
Caso B: Terapia
• Broncodilatazione: beta agonisti
short acting e long acting,
anticolinergici (riduzione della CO2)
• Ossigeno terapia
• Diuretici?
• Digitale?
• Riabilitazione
Adverse cardiovascular events by
b2 agonist use in COPD patients
• Myocardial infarction
• Congestive hearth failure
• Cardiac arrest and acute cardiac death
Increase of heart rate and decrease of
potassium concentration, associated with
other effect of b-adrenergic stimulation
may precipitate ischemia, congestive
heart failure, arrythmias and sudden
death
S.R. Salpeter, Chest 2004, 125: 2309-2321
Caso A: Terapia
•
•
•
•
•
Diuretici
Digitale?
ACE inibitori
Ossigeno terapia
Beta bloccanti cardioselettivi
β-Blockers
• The ßB has traditionally been
contraindicated
in
COPD
mainly because of anecdotal
evidence and case reports
citing acute bronchospasm
after their administration
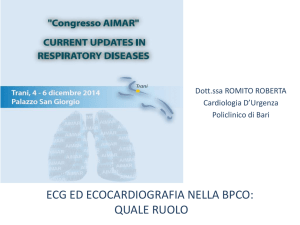
Assessing the effects (mortality,
hospital admissions, and COPD
exacerbations) of BB therapy on 5977
COPD patients on top of standard
therapy with a mean follow-up of 4.35
years.
BMJ 2011;342:d2549
Kaplan-Meier survival curves among
patients with COPD by use of β blockers
22% overall
reduction in all
cause mortality
for COPD
patients taking
BB in addition
to standard
therapy for
COPD.
BMJ 2011;342:d2549
Why BB may improve outcomes in HF
and COPD patients?
• Up-regulation of β2 adrenoceptors by
chronic β blockade may improve the
effectiveness of β2 agonists
(cardioselective β blockers such as
bisoprolol, have been shown to exert
significant β2 adrenoceptor antagonism,
resulting in β2 adrenoceptor upregulation).
• Cardioprotective effects of β blockade
(decrease in oxygen consuption, increase
diastolic filling, antioxidant properties)