Dipartimento di Presidio Fossano Caraglio
Direttore Dr. Riccardo Conte
“NUTRIZIONE ED INVECCHIAMENTO”
Il ruolo dell’invecchiamento
fisiologico e patologico
sull’assetto nutrizionale
Giorgetta Cappa
Fossano 26 novembre 2011
The Fight Against Malnutrition has the overall goal to
secure that everyone who needs care for disease,
old age or handicap receives proper nutritional
care.
The probem is that nutritional treatment is grossly
underutilized in just about every care situation all
over Europe.
At the individual level malnourished people suffer
substantially more from disease than necessary.
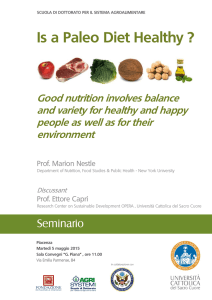
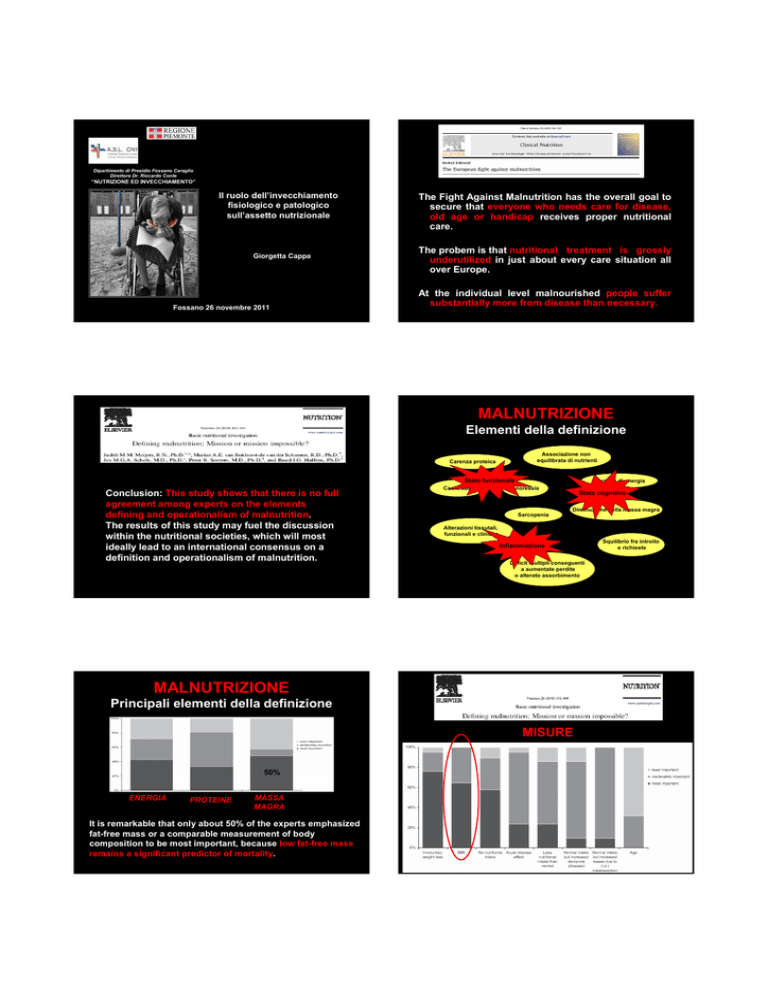
MALNUTRIZIONE
Elementi della definizione
Associazione non
equilibrata di nutrienti
Carenza proteica
Stato funzionale
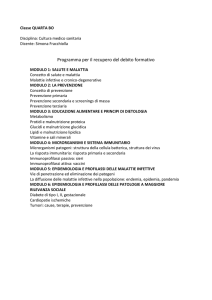
Conclusion: This study shows that there is no full
agreement among experts on the elements
defining and operationalism of malnutrition.
The results of this study may fuel the discussion
within the nutritional societies, which will most
ideally lead to an international consensus on a
definition and operationalism of malnutrition.
Cachessia
Carenza di energia
Anoressia
Stato cognitivo
Diminuzione della massa magra
Sarcopenia
Alterazioni tissutali,
funzionali e cliniche
Squilibrio fra introito
e richieste
Infiammazione
Deficit multipli conseguenti
a aumentate perdite
o alterato assorbimento
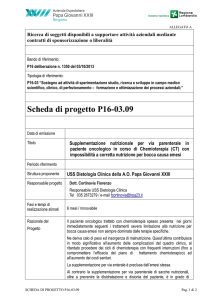
MALNUTRIZIONE
Principali elementi della definizione
MISURE
50%
- Non concordanza sul cutoff di
LOW-BMI (BMI < 18-21 kg/m2)
ENERGIA
PROTEINE
MASSA
MAGRA
- BMI affidabile indicatore di
massa magra solo per valori
It is remarkable that only about 50% of the experts emphasized
fat-free mass or a comparable measurement of body
composition to be most important, because low fat-free mass
remains a significant predictor of mortality.
molto bassi
SARCOPENIA
SCARSE
PROTEINE
PERDITA DI
MASSA
MAGRA
PERDITA DI
CAPACITA’
FUNZIONALE
PROTEIN INTAKE
RDA - WHO Geneva 1985
Optimal protein intake in the elderly.
0.80 g/kg
1.5 g/kg
Clin Nutr 2008
Increasing dietary protein requirements
in Elderly people for optimal muscle and
bone health.
1.6 - 1.8 g/kg
(short term)
JAGS 2009
Are Elderly Hospitalized Patients Getting
Enough Protein?
1.06 ±0.28 g/kg
JAGS 2008
Patologie croniche
Comorbilità
Infiammazione (IL, PCR, TNFα)
Alterazioni metaboliche
(anemia, ipoalbuminemia, IGT)
Sarcopenia
Cachessia
60% proteine corporee nei muscoli.
In situazione di stress metabolico le proteine muscolari sono
rapidamente mobilizzate per fornire aminoacidi, specialmente
glutammina, al fegato, intestino e sistema immunitario.
FRAGILITÀ: un concetto in evoluzione
Fenotipo fisico della fragilità
•Perdita di peso non intenzionale
… la sua identificazione, trattamento e
prevenzione sono oggi considerati il
“cuore” ed allo stesso tempo la sfida
principale della medicina geriatrica …
4,5Kg nell’ultimo anno
•Riferita esauribilità
Item della CES-D Depression Scale
•Diminuzione della velocità di
Tempo impiegato a percorrere 4,5
cammino
metri
•Forza muscolare
Hand Grip Strenght Test
•Diminuita attività fisica
Minnesota Leisure Time Activity
Questionnaire (SV): < 270 Kcal/sett
Presenza di 3 su 5 criteri
G. Gerontol 2011; 59: 125-129
NUTRIENT DENS FOOD vs EMPTY CALORIES !
FACTORS INFLUENCING NUTRITIONAL INTAKE:
Eating nutrient-dense foods become especially important as we get older.
We generally need fewer calories because we tend to become less active
and our lean-muscle mass decreases with age. However we still need the
same amount of most vitamins and mineral…This means that as we get
older, we need to get the same amount (or more) of nutrients from eating a
smaller amount of food.
Personal Factors:
Food Factors:
Environmental Factors:
Satiety
Macronutrients and fibres
Timing
Anorexia of aging
Taste, variety, palatability
and sensory-specific satiety
Social isolation
Energy density
Encouragement, help with
eating and interruptions
Portion size and volume
Ambiance
Liquid vs solid foods
Viscosity
J. Am. Diet Ass. 2008; 108: 937 - 938
ANORESSIA
DELL’INVECCHIAMENTO
SUPPORTO NUTRIZIONALE
NUTRIZIONE PARENTERALE
CIBI FORTIFICATI
ESPEN GL 2009
Cibo normale arricchito con
specifici nutrienti
+ 26% energia, + 23% proteine
in anziani ospedalizzati
NUTRIZIONE ENTERALE
ESPEN GL 2006
INTEGRATORI (ONS)
SNG, PEG
Supplemento alla normale
alimentazione (liquidi,
barrette, polveri)
ONS liquidi favoriscono un più rapido
svuotamento gastrico
Clinical Nutrition 2010; 29: 160 - 169
Small weight gain, but no longer supports
the finding that there is a beneficial effect on
mortality overall.
There is more evidence of a reduction in
complications than in the previous review.
Ridotto meccanismo di compensazione
dell’introito energetico nell’anziano
Further more, elderly people may become
more malnourished because they do not
get assistance with feeding on a busy ward,
and encouragement and assistance may be
all that they require.
Data on the effects of restrictive diets in older
persons are still scarce.
With increasing age,
restrictive diets seem to be less effective with regard
to relevant study endpoints like morbidity, quality of
life and mortality.
Main long-term restrictive diets in the elderly.
Unwarranted and/or ‘‘historical’’ diets without benefit for the patient
- Salt-free diet for hypertension or congestive heart failure
- Low-carbohydrate diet, without simple carbohydrates, for type 2
diabetes mellitus
- Low-fat diet for hypercholesterolemia
- Very low-protein diet for chronic kidney disease
Restrictive diets sometimes justified but to be regularly evaluated
- Moderate caloric restriction (-500 to 750 kcal/d compared with the
usual diet) coupled with regular physical activity for complicated obesity
(especially with type 2 diabetes)
- Moderate reduction of sodium intake (100–120 mmol/d) for resistant
hypertension or congestive heart failure
- Moderate protein restriction (0.8–1.0 g/kg body weight/d) for chronic
kidney disease (before dialysis)
Even in older persons dietary restrictions may be valuable
over a limited period of time during an acute disease. In the
long run, the benefit/risk ratio of restrictive diets is usually
unfavourable. Efforts to improve health status via dietary
restrictions may translate into deficiencies thus producing a
major additional risk for malnutrition and frailty, with a
subsequently increased risk of morbidity and mortality.
In older persons, the promotion of physical
activity to maintain muscle mass complies
more
effectively
with
the
goals
prevention than dietetic restrictions do.
Although proprietary sip feeds have
become a widely accepted means of
improving nutritional status, it is not
enough to provide supplements and hope
for the best.
of
Fattori personali che condizionano
l’apporto nutrizionale nell’anziano
Fattori alimentari che condizionano
l’apporto nutrizionale nell’anziano
Riducono l’intake
Riducono l’intake
Personali
Favoriscono l’intake
Favoriscono l’intake
Alimentari Ingredienti:
Ingredienti:
•Proteine elevate
•Fibre elevate
•Carboidrati a lento assorbimento
•Grassi elevati
Caratteristiche del cibo:
Caratteristiche del cibo:
Cambiamenti psicologici
•Elevata viscosità
•Ampio volume
•Diete monotone
Processo alimentare
Cibo culturalmente inappropriato
•Elevata palabilità
•Aspetto appetitoso
•Elevata densità energetica
•Volume piccolo/
piccole porzioni
•Liquidi (fra i pasti)
•Varietà della dieta
Cambiamenti sociali
Buona salute
Cambiamenti fisiologici
Motivazione
Presentazione di porzioni troppo
ampie
Clinical Nutrition, 2010
Clinical Nutrition, 2010
Fattori ambientali che condizionano
l’apporto nutrizionale nell’anziano
Riducono l’intake
Ambientali
Favoriscono l’intake
Vivere soli
Distrazioni(eg TV,…)
Isolamento sociale
Convenienza/facile accesso
al cibo
Eventi che interrompono i
pasti
Mancanza di aiuto durante i
pasti
Tempo del pasto non
appropriato
Deficit visivo
Deterioramento cognitivo
Difficoltà motorie
Oronasali:
Problemi dentari e cattiva masticazione
Secchezza del cavo orale
Minor sensibilità gustativa ed olfattiva
Gastrointestinali:
Rallentato svuotamento gastrico
Peggioramento della funzione intestinale
Sazietà
Maggior sensibilità a CCK
Sazietà rapida e durevole
Minor fame
Minor sete
Processo
alimentare più
lento
Minor varietà della
dieta
Meno spuntini
Ridotto introito
alimentare
Consumare il pasto alla
stessa ora
Cambiamenti fisiologici
•
•
•
•
Problemi
psicologici
MALNUTRIZIONE
Clinical Nutrition, 2010
Disabilità funzionali:
•
•
Cambiamenti
fisiologici
Consumare il pasto con
altre persone
ANOREXIA OF AGEING
•
•
•
Cambiamenti
sociali
Incoraggiamento da parte
del care giver
Clinical Nutrition, 2010
•
•
•
ANOREXIA OF AGEING
The
prevalence
of
undernutrition
and
risk
of
undernutrition in community dwelling older adults
… 6% of frail older adults (78–86 years) undergoing rehabilitation were
(>65 years) have been reported to be 4.3% and 25.4%,
malnourished and 13% mildly malnourished…
respectively.
Public Health Nutr 2009;12: 82-90
J Nutr Health Aging 2008; 12: 721 - 726
…the prevalence of malnutrition in long-term care home residents has been
estimated to be as high as 85%....
The Fight Against Malnutrition has the overall goal to secure
that everyone who needs care for disease, old age or handicap
receives proper nutritional care.
The problem is that
nutritional
treatment
is grossly
underutilized in just about every care situation all over Europe.
The cost for society of malnutrition is around
120 Billion
Euros annually.
Nutr Rev 2007; 65: 135 - 138
MALNUTRIZIONE
PAZIENTI OSPEDALIZZATI
Prevalenza media 18% (range 5%-37.5%) di pazienti sottopeso
ricoverati in ospedale
Stratton RJ 2003
…a state of nutrition in which a deficiency
or excess (or imbalance) of energy, protein
and other nutrients causes measurable
Incidenza tra il 20% e il 50% di malnutrizione calorico-proteica negli
anziani ospedalizzati.
adverse effects on tissue/body form (body
shape, size and composition) and function,
Clin Nutr 2008
and clinical outcome.
Incremento dei costi dal 75 sino al 300% per la presenza di malnutrizione.
Clin Nutr 2003 - Am J Diet Assoc 2000
Elia M. Guidelines for detection and management of malnutrition.
Maidenhead: Standing Committee of BAPEN; 2000.
CONSEGUENZA DELLA MALNUTRIZIONE SUGLI
OUTCOME E LA QUALITA’ DI VITA
COME RICONOSCERE LA MALNUTRIZIONE ?
VALUTAZIONE CLINICA
Allungamento del tempo di degenza
Aumento del tasso di complicanze (20 fold)
Aumento della morbilità rispetto ai pazienti senza problemi
nutrizionali di uguale patologia
Persistenza
della
- comunità MUST
- altezza
- modificazioni anamnestiche
malnutrizione
post
dimissione
con
incremento del tasso di riammissione ospedaliera o di
(Malnutrition Universal Screening Tool)
recenti del peso, soprattutto se
“involontarie”
mortalità ad un anno
Sarcopenia correlata ad insufficienza respiratoria e a perdita
ESPEN GL FOR NUTRITION
SCREENING 2002
-peso
- valutazione capacità
- ospedale NRS 2002
(Nutritional Risk Screening)
deglutitoria con test di I°livello
dell’ autonomia nelle attività quotidiane
- diario alimentare durante la
- anziani MNA-SF
degenza
(Mini Nutritional Assessment Short Form)
MNA-SF
Alta correlazione con full MNA
Alta accuratezza diagnostica
In elderly people at risk of undernutrition ONS improve nutritional
status and reduce mortality.
Minimo tempo di esecuzione
Basso tasso di risposte “non so”
ESPEN Vienna 2009
TF is clearly indicated in patients with neurologic dysphagia.
In contrast, TF is not indicated in final disease states, including final
dementia, and in order to facilitate patient care.
Oral nutritional therapy via assisted feeding and dietary supplements is
often difficult, time-consuming and demanding … therefore, even in
times of declining financial and human resources, it is unacceptable to
initiate tube feeding (TF) merely in order to facilitate care or save time.
NUTRIENT DENS FOOD vs EMPTY CALORIES !
OMEGA 3 A LUNGA CATENA (EPA - DHA)
CAUSE
Micronutrienti introdotti in quantità inferiore al fabbisogno
in percentuale 33-92% negli anziani in comunità
J. Nutr. 2008
RESOLVINE - NEUROPROTECTINE
…Vitamine liposolubili, Calcio, Vit D, Potassio, Fibre, Vit B12, Vit B6, Ac. Folico…
ALTO POTERE ANTI-INFIAMMATORIO
Dieta mediterranea
Rivalutazione uova,
fegato, frattaglie, latte
intero e derivati
“Alla domanda: chi è il tipico paziente geriatrico?
Il valore aggiunto della alimentazione deve essere
La risposta è: pensa al più anziano, al più malato, al
ricercato nella sinergia, antagonismo e ridondanza
più complicato ed al più fragile dei tuoi pazienti…
dei nutrienti che la compongono e non sulla
affetto di solito da multiple malattie, la cui
validità “scientifica” del singolo nutriente.
presentazione è spesso atipica, e portatore di
Field J.C. Am. J. Clin. Nutr 2009
deficit funzionali. I suoi problemi di salute sono
cronici, progressivi, solo in parte reversibili…”
Hazzard, 1999
(modificata)
NRS 2002
… 6% of frail older adults (78–86 years) undergoing rehabilitation were
malnourished and 13% mildly malnourished…
The prevalence in community
dwelling
older
adults
(>65
years):
J Nutr Health Aging 2008;12:721–6
Frail older adults (78–86 years)
undergoing rehabilitation:
- malnourished 6%
undernutrition 4.3%
- mildly malnourished 13%
risk of undernutrition 25.4%
J Nutr Health Aging 2008;12:721–6
…the prevalence of malnutrition in long-term care home residents has been
Public Health Nutr 2009; 12: 82-90
estimated to be as high as 85%....
Nutr Rev 2007;65:135–8
Mean prevalence of underweight
Prevalence of malnutrition in
in patients admitted to hospital:
…the mean prevalence of being underweight in patients admitted to
long-term care home residents:
approximately 18% (range 5%-
hospital is approximately 18% (range 5%-37.5%)…
as high as 85%
37.5%)
Stratton RJ 2003
Nutr Rev 2007;65:135–8
Stratton RJ 2003
ENTERAL TUBE FEEDING FOR OLDER
PEOPLE WITH ADVANCED DEMENTIA
REVIEW 2009
The success of ONS is sometimes limited by
poor compliance due to low palatability,
side effects such as nausea and diarrhoea,
and by cost.
Calculations extrapolated from the ESPEN sister society BAPEN in
the UK to the EU situation indicates that as many as 20 million
individuals are at risk for malnutrition and that the cost for society
of malnutrition is around 120
Clinical Nutrition (2006) 25, 330–360
Billion Euros annually.
CONSEGUENZA DELLA MALNUTRIZIONE SUGLI
OUTCOME E LA QUALITA’ DI VITA
- longer hospital stays, and present a 20-fold increase in complication rate
The prevalence of malnutrition which is 5–10%
- morbidity is increased in these patients compared to well-nourished
among independently living older individuals is
individuals with the same diseases
considerably higher (30–60%) in hospitalized or
- nutritional deficits often persist for variable periods subsequent to
institutionalized older adults.
discharge
- patients who remain undernourished at discharge have substantially
increased rates of early hospital readmission and 1- year mortality
- sarcopenia with muscle wasting is a major consequence of undernutrition,
leading to respiratory failure and decreased capacity for daily activities.
Clinical Nutrition 2010
PRINCIPALI CAUSE DI INVOLONTARIA PERDITA DI PESO
(5-10% del peso corporeo nei precedenti 12 mesi)
depressione
cancro
patologie cardiache
basso livello socio-economico
…Key features of NHs with a low rate of tube-feeding use
disabilità funzionale
include a physical
patologie gastrointestinali benigne
enjoyment
of
environment
food,
that
administrative
promotes the
support,
and
empowerment of staff to value hand feeding and shared
decision-making processes involving family members.
Nei pazienti istituzionalizzati il 58% dei casi di involontaria perdite
di peso è da attribuire a patologie psicogeriatriche, compresa la
depressione
Arch Intern Med. 2010
Am Fam Physician 2002
PRE CACHEXIA
DEFINIZIONE
SARCOPENIA
INDICATORI
- underlying chronic disease
- C-reactive protein
- unintentional weight loss 5% of
- impaired glucose tolerance
usual body weight during the last
- anaemia related to inflammation
6 months
- hypoalbuminemia
- chronic or recurrent systemic
inflammatory response
- anorexia
or
- A low muscle mass, i.e. a percentage of muscle mass 2
standard deviations below the mean measured in young adults
of the same sex and ethnic background.
- Low gait speed, e.g. a walking speed below 0.8 m/s in the 4-m
walking test.
PERDITA
DI MASSA
MAGRA
PERDITA DI
CAPACITA’
FUNZIONALE
anorexia-related
symptoms.
Clinical Nutrition 2010; 29: 154-159
Clinical Nutrition 2010; 29: 154-159