Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Università Campus Bio-Medico di Roma
Corso di dottorato di ricerca in
Immunologia Oculare
XXII ciclo anno 2007
Fisiopatologia, diagnosi, qualità della vita, stadiazione e nuove
strategie di trattamento della cheratocongiuntivite primaverile (VKC)
Marta Sacchetti
Coordinatore
Prof Stefano Bonini
Tutore
Dott Alessandro Lambiase
26 Febbraio 2010
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Abstract
La cheratocongiuntivite primaverile (VKC) è una patologia allergica cronica che colpisce
prevalentemente i bambini caratterizzata da intensi sintomi oculari con recrudescenza stagionali
spesso associate a coinvolgimento corneale. Tale malattia è ancora scarsamente caratterizzata dal
punto di vista della patogenesi, della diagnosi, dell’impatto sulla qualità della vita e del
trattamento. La VKC è una patologia ad eziologia allergica caratterizzata da una risposta
immunitaria di tipi T helper 2 (Th2). L’immunità innata svolge un ruolo nella patogenesi della
VKC come è stato evidenziato in recenti studi, tra cui un nostro studio in cui è stato dimostrato
un aumento delle cellule natural killers nella congiuntiva di pazienti con VKC rispetto ai
controlli. Nostri dati preliminari indicano anche un coinvolgimento degli ormoni sessuali nella
patogenesi della VKC.
L’inquadramento diagnostico della VKC pone delle difficoltà, in quanto i bambini
sperimentano limitazioni nella qualità della vita, dovuta alla malattia, e il quadro clinico presenta
ampia variabilità nell’arco dell’anno. L’impatto della VKC sulla qualità della vita nel bambino
non era mai stata valutata, abbiamo quindi creato e validato un questionario specifico per
bambini con VKC (il QUICK© test ). Inoltre, poiché non esistono classificazioni della severità
della VKC, abbiamo effettuato uno studio retrospettivo su 207 casi di VKC, i dati sono stati
analizzati con il metodo CART, al fine di ricavare un algoritmo decisionale da applicare nella
pratica clinica, di proporre una stadiazione della severità e individuare i fattori di rischio per un
peggiore esito visivo.
Dal punto di vista terapeutico, attualmente i farmaci di scelta della VKC sono i colliri
antiallergici topici, nelle fasi lievi e moderate, e gli steroidi topici nelle fasi di acuzie, efficaci ma
non privi di effetti collaterali, anche gravi. C’è quindi l’esigenza di terapie alternative, che
consentano un miglior controllo della malattie con minori effetti collaterali. In uno studio
multicentrico abbiamo dimostrato l’efficacia della Ciclosporina A in collirio nel ridurre il
numero delle recrudescenze della VKC.
2
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
INDICE
1. Introduzione…………………………………………………………………………..5
2. Caratteristiche cliniche e inquadramento diagnostico della VKC………………...7
3. Patogenesi della cheratocongiuntivite primaverile……………………………….13
3.1 Fattori genetici……………………………………………………………………………….13
3.2 Fattori ormonali……………………………………………………………………………..14
3.3 Studio preliminare sul ruolo deglio romoni sessuali nella patogenesi della VKC…16
4. Fisiopatologia ……………………………………………………………………….19
4.1 Mediatori nella VKC ……………………………………………………………………….19
4.2 Cellule nella VKC……………………………………………………………………..…….21
5. Trattamento della cheratocongiuntivite primaverile…………………………….24
5.1 Studio multicentrico randomizzato controllato in doppio cieco per la valutazione
dell’efficacia del trattamento con ciclosporina A in collirio nella prevenzione delle recidive
dell’infiammazione nella VKC……………………………………………………………….27
5.2 Studio aggiuntivo per valutare l’efficacia della ciclosporina per il trattamento delle
fasi acute della VKC………………………………………………………………………….31
5.3 Trattamento chirurgico della cheratocongiuntivite primaverile ………………..35
6. Conclusioni………………………………………………………………………….36
7. Bibliografia…………………………………………………………………………..37
8. Lavori allegati ……………………………………………………………………..48
8.1 Sacchetti M, Baiardini I, Lambiase A, Aronni S, Fassio O, Gramiccioni C, Bonini
S, Bonini S.Development and testing of the quality of life in children with vernal
keratoconjunctivitis questionnaire.Am J Ophthalmol. 2007 Oct;144(4):557-63.
8.2 Bonini S, Sacchetti M, Mantelli F, Lambiase A.(2007)Clinical grading of vernal
keratoconjunctivitis.Curr Opin Allergy Clin Immunol;7(5):436-41.
3
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
8.3 Lambiase A, Normando EM, Vitiello L, Micera A, Sacchetti M, Perrella E, Racioppi L,
Bonini S, Bonini S (2007): Natural killer cells in vernal keratoconjunctivitis. Mol Vis 13:
1562–1567.
8.4 Marta Sacchetti, Alessandro Lambiase, Flavio Mantelli,Velika Deligianni, Andrea
Leonardi, Stefano Bonini. Tailored Approach to the Treatment of Vernal Keratoconjunctivitis.
Ophthalmology IN PRESS
8.5 Iovieno A, Lambiase A, Sacchetti M, Stampachiacchiere B, Micera A, Bonini S.(2008)
Preliminary evidence of the efficacy of probiotic eye-drop treatment in patients with vernal
keratoconjunctivitis.Graefes Arch Clin Exp Ophthalmol.246(3):435-41.
4
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
1. Introduzione
La cheratocongiuntivite primaverile (VKC) è una patologia allergica cronica che colpisce
prevalentemente i bambini, caratterizzata da intensi sintomi oculari quali prurito, lacrimazione,
fotofobia e arrossamento, associati ad infiammazione della congiuntiva bulbare e tarsale. (Bonini
2000) L’origine allergica di questa condizione è largamente accettata, ma l’eziologia e la
patogenesi sono ancora scarsamente caratterizzate. Recentemente, sono stati condotti numerosi
studi sulle cellule e i mediatori coinvolti nell’infiammazione che hanno evidenziato come la
patogenesi della VKC è molto più complessa di una semplice reazione da ipersensibilità di tipo I,
che caratterizza altre forme di congiuntivite allergica, più comuni e meno severe. Ad oggi però,
il ruolo di una possibile predisposizione genetica e/o dei fattori ambientali coinvolti
nell’insorgenza, nella progressione e nella risoluzione di tale condizione non sono stati ancora
chiariti.
Sebbene sia definita “primaverile” la VKC ha spesso un andamento cronico durante tutto
l’anno con recrudescenze stagionali, in primavera ed in estate, caratterizzate da un
peggioramento della sintomatologia ed un frequente interessamento corneale che va dalla
cheratite puntata superficiale a vere e proprie ulcere corneali con compromissione della funzione
visiva.(Leonardi 2002, Bonini 2000) Tale decorso, associato ad un’importante variabilità della
severità della sintomatologia nel corso dell’anno, comportano una compromissione della qualità
della vita del bambino con VKC e richiedono un importante impegno nella gestione e
nell’approccio al paziente con VKC, volto ad un controllo ottimale dei sintomi e i segni sia
durante l’anno, ma soprattutto nelle fasi di acuzie.
I farmaci antiallergici topici disponibili per il trattamento della VKC si sono dimostrati
efficaci nel controllo dei sintomi nelle forme lievi e moderate della malattia, laddove le fasi di
acuzie dell’infiammazione, richiedono l’uso di steroidi topici, efficaci ma non scevri di effetti
collaterali anche gravi e permanenti quali il glaucoma e la cataratta. C’è quindi lì esigenza di
5
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
valutare l’ efficacia di nuove terapie per il controllo della malattia, quali la Ciclosporina A in
collirio, che consentano un buon controllo della malattia, e minori rischi di effetti collaterali.
6
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
2. Caratteristiche cliniche e inquadramento diagnostico della VKC
La cheratocongiuntivite primaverile ha una maggiore prevalenza in zone di clima
temperato, l’area del Meditarreneo, l’Africa centrale e occidentale, il Medio Oriente, il
Giappone, il sucontinente Indiano e il Sud America.
La VKC colpisce più frequentemente i bambini di sesso machile con un rapporto
maschi/femmine di 4:1 to 2:1 in diversi studi, caratteristicamente, tale differenza non si mantiene
nelle forme che si presentano in età adulta, in cui il rapporto maschi/femmine non mostra
sostanziali differenze. (Neumann et al. 1959; Bonini et al. 2000, Bielory 2000, Lambiase 2009).
La VKC insorge prima dei 10 anni, l’età media di insorgenza è tra 4 e 6 anni, e in genere risolve
dopo la pubertà, presentando quindi un durata media tra 4 e 10 anni. (Bielory 2000; Leonardi
2002a).
Nella sua forma tipica, la VKC si presenta con intensi sintomi oculari quali prurito,
iperemia, fotofobia e lacrimazione. Le principali caratteristiche cliniche della VKC sono
elencate in tabella (Bonini S 2000)
7
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Nella maggior parte dei pazienti (98%), la VKC è bilaterale, anche se piccole differenze
di gravità tra i due occhi sono comuni (Bonini et al. 2000). L’andamento della malattia mostra
spesso un esordio stagionale ma, nell’evoluzione, può diventare perenne dopo pochi anni. In
circa un quarto dei pazienti con VKC la malattia è presente durante tutto l'anno, senza alcuna
remissione, fin dall'esordio (Bonini et al. 2000).
I pazienti con VKC presentano tipicamente diversi episodi di infiammazione attiva
durante tutto l'anno, durante tali riacutizzazioni la sintomatologia si aggrava notevolmente a
causa dell’infiammazione oculare che frequentemente si accompagna ad un interessamento
corneale, caratterizzato da alterazioni epiteliali, quali epiteliopatia puntata, fino a vere e proprie
ulcere corneali a scudo, formazioni di placche e neovascolarizzazione corneale. (Allansmith
1988; Buckley 1988). L’insorgenza di ulcera corneale è riportata nel 3-11% dei pazienti con
VKC,e nel, 6% dei pazienti affetti da VKC causa una riduzione del visus dovuto esiti corneali.
(Neumann et al. 1959; Cameron 1995; Tabbara 1999, Bonini 2000). Un’altra caratteristica della
VKC è la secrezione di muco iper-denso, filamentoso e appiccicoso, che provoca intenso fastidio
e aggrava la sintomatologia. Durante le riacutizzazioni, si assiste anche alla comparsa di punti di
trantas al limbus, depositi di eosinofili degradati e detriti di cellule epiteliali.(Figura 1)
8
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
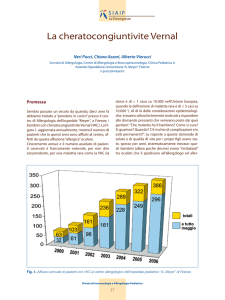
Figura 1. Durante le riacutizzazioni dell’infiammazione della VKC si osserva un
frequente intereassamento corneale con puntata superficiale (A) o vere e proprie ulcere
conrneali (B), associate a inetnsa iperemia congiuntivale (C), papille congeste (C e F), punti
di trantas (D) e inensa secresione di muco iperdenso (E, F)
9
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
La reazione papillare congiuntivale è un’altra caratterista della VKC, ma tende a permanere
anche nelle fasi di quiescenza. Le papille nella VKC sono tipicamente di grandi dimensioni (> 1
mm), più frequentemente localizzate al tarso superiore, altre volte possono interessare il limbus.
(Figura 2)
Figura 2. Reazione papillare limbare moderata (A) e severa (B) e reazione papillare
tarsale superiore mederata 2+( C) e severa 3+ (D).
In base alla localizzazione delle papille, la VKC viene classificata in tarsale, limbare o
mista (Verin et al. 1999). Nelle fasi di riacutizzazione, le papille diventano congeste, iperemiche
e intervallate a muco rappreso. Bonini et al. (2000) ha classificato le papille tarsali superiori
come segue:
(1) Grado 0: nessuna reazione papillare.
(2) Grado 1 +: papille rare, di 0,2 millimetri, sparse nella congiuntiva tarsale o intorno al
limbus.
(3) Grado 2 +: papille di 0,3-1 millimetri sulla congiuntiva tarsale o al limbus.
(4) Grado 3 +: papille di 1-3 mm tutte le sulla congiuntiva tarsale o per 360° intorno al
limbus.
10
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
(5) Grado 4 +: papille di più 3 millimetri sulla congiuntiva tarsale o formazione
gelatinosa al limbus che coinvolge la cornea periferica.
La dimensione delle papille correla direttamente con la persistenza e il peggioramento dei
sintomi nel follow-up a lungo termine (Bonini et al. 2000). (Figura 3)
Figura 3. Curva di sopravvivenza dei pazienti con VKC in base al grado di severità
dlle papille tarsali (Bonini S 2000)
La sintomatologia oculare, e soprattutto il prurito e la fotofobia, possono variare da lieve
a intensi ed essere aggravati da l'esposizione al vento, polvere, luce intensa, caldo o lo sforzo
fisico associato con la sudorazione. Tale esagerata iper-reattività a stimoli non-specifici come il
calore, sole e del vento durante la fase attiva della VKC ha suggerito il coinvolgimento
dell’infiammazione neurogenica nella patogenesi della VKC (Bonini, 1992a).
L’intensa sintomatologia, la forte variabilità di manifestazioni cliniche della VKC, e il
fatto che la VKC colpisce prevalentemente i bambini nell’età evolutiva, ha spinto il nostro
gruppo a indagare l’impatto della VKC sulla qualità della vita. Poiché non esistevano strumenti
specifici per valutare la qualità della vita nella VKC, un questionario specifico per bambini con
la cheratocongiuntivite primaverile (il QUICK© test ), è stato creato e validato su una
popolazione di bambini con VKC da 5 a 12 anni. (Sacchetti M 2007-lavoro allegato)
11
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Non ci sono precisi criteri diagnostici per questa malattia. Iperemia, prurito, fotofobia,
lacrimazione e secrezione mucosa sono sintomi tipici della VKC, ma non specifici, in quanto
sono comuni anche ad altre malattie della superficie oculare quali la cheratocongiuntivite
atopica, le blefarocongiuntiviti, l’occhio secco. Le papille giganti sulla congiuntiva tarsale
superiore e al limbus sono caratteristiche tipiche della VKC. La diagnosi si basa quindi sulle
caratteristiche cliniche, l’età, la familiarità,l’andamento della malattia, e sulla presenza dei tipici
segni e sintomi clinici, con l’inevitabile conseguenza che i casi lievi o atipici possono sfuggire
alla diagnosi.
Nonostante la disponibilità di nuove conoscenze sulla patogenesi della VKC, nessun test
clinico o marker diagnostico di laboratorio è stato sviluppato per supportare la diagnosi nei casi
atipici o per predire il corso di questa malattia. (Bonini et al. 2000)
La mancanza di criteri diagnostici standard e di un linguaggio comune tra gli oculisti per
quanto riguarda la gravità della VKC rende più difficile diagnosticare e trattare questa malattia.
Bonini et al. (2007) ha proposto una classificazione clinica delle fasi cliniche della VKC per
aiutare i medici ad utilizzare un linguaggio comune nella diagnosi e nella gestione della VKC e
per consentire una più omogenea la selezione dei pazienti per sperimentazioni cliniche. (Bonini
2007-lavoro allegato)
12
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
3. Patogenesi della cheratocongiuntivite primaverile
3.1 Fattori genetici
La caratteristica distribuzione geografica, e la persistenza di incidenza della VKC nelle
popolazioni emigrate suggerisce la possibilità di una predisposizione genetica alla base della
patogenesi della VKC. A sostegno di tale ipotesi, uno studio ha dimostrato che la VKC è più
comune tra individui di origine asiatica e africana che vivono in Svezia (Montan et al. 1999).
Finora, però, nessun fattore genetico predisponente è stato identificato perla VKC.
Inoltre, la costante e maggiore presenza di eosinofili nel sangue, lacrime e nel raschiato
congiuntivale, l'espressione di una moltitudine di mediatori e citochine, così come la
predominanza delle cellule CD4 a livello locale nella VKC suggeriscono che tale malattia
potrebbe appartenere ad un fenotipo di upregulation del cluster di geni di citochine sul
cromosoma 5q. Il cluster di geni di citochine, attraverso i suoi prodotti come la interleuchina (IL)
-3, -4, -5 e il GM-CSF, regola la prevalenza di cellule T helper di tipo 2 (Th2), la crescita e la
funzione dei mastociti e degli eosinofili così come la produzione di immunoglobuline (Ig) E
nella VKC (Bonini et al.1995a).
La presenza di familiarità per malattie allergiche come asma, rinite, eczema, orticaria e è
stata riportata nel 49% dei pazienti affetti da VKC (Bonini et al. 2000) suggerendo una
predisposizione allo sviluppo di malattie atopiche in questi pazienti. Inoltre, un terzo dei pazienti
con VKC presenta malattie atopiche associate (Bonini et al. 2000, Tuft et al.1989), tra cui la più
comune è l’asma.
Anche il cheratocono, altra condizione ad ereditarietà multifattoriale, sembra avere una
maggiore incidenza nei bambini con VKC (circa 15%) (Iqbal et al. 2003).
13
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
3.2 Fattori ormonali
La predilezione per il sesso maschile e la risoluzione dopo la pubertà suggeriscono inoltre
un ruolo degli ormoni sessuali nello sviluppo della VKC. Uno studio di Bonini del 1995
evidenziava un aumento significativo nell’espressione dei recettori degli estrogeni e del
progesterone nella congiuntiva di bambini con VKC, rispetto ai controlli sani. (Bonini et al.
1995b)
L’influenza degli ormoni androgeni ed estrogeni sul sistema immunitario è stata
evidenziata da numerosi studi epidemiologici, clinici e sperimentali. Infatti, è stata evidenziata
una diversa prevalenza delle malattie allergiche tra i sessi. In generale i bambini sono più
frequentemente affetti da eczema atopico, asma e congiuntivite allergica rispetto alle bambine, e
tale rapporto si inverte dopo la pubertà, con maggiore frequenza di malattie atopiche nelle donne
rispetto agli uomini.(W Chen 2008)
È stato dimostrato che gli estrogeni sono in grado di stimolare la sintesi di anticorpi
potenziando l’immunità umorale. Inoltre le cellule mastocitarie esprimono in Recettore alfa per
gli estrogeni, che stimola la degranulazione mastocitaria. (Cutolo M 2004, Narita S 2007). Il
progesterone sembra essere in grado di potenziare la produzione di IgE, ma studi dimostrano
anche la sua azione di soppressione del rilascio di istamina. (Mitchell VF 207, Vasiadi M 2006)
L’azione degli androgeni nelle patologie atopiche è ancora poco chiara. Il pregnenolone,
il deidroepiandrosterone (DHEA) e il DHEA-solfato (DHEAS), causano rapida degranulazione
mastocitaria in vitro. (Malkin CJ 2003). Studi in modelli animali di allergia hanno evidenziato
che il DHEA è in grado di sopprimere l’ infiammazione allergica delle vie aeree suggerendo che
l’effetto soppressivo del DHEA sia associato ad una downregulation della risposta Th2 (Yu CK
2002). È stato inoltre dimostrato che la somministrazione di DHEA sopprime l’aumento delle
IgE del siero e dei livelli di IL-6 in un modello animale di eczema atopico. (Sudo N 2001). In un
altro studio, i livelli di DHEA sierici in pazienti adulti di sesso maschile (di età compresa tra 1930 anni) con eczema atopico sono risultati significativamente inferiori a quelli dei controlli sani
14
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
di sesso maschile della stessa età. (Tabata N 1997) Tuttavia, poiché non sono noti i recettori
ormonali specifici per il DHEA, resta da stabilire se l'effetto del DHEA sia mediato attraverso la
sua maggiore conversione in testosterone e in estradiolo negli uomini rispetto alle donne.
Il testosterone sembrerebbe avere un effetto inibitorio della rispostaallergica, infatti, non
influenza il rilascio di istamina in colture cellulari di mastociti in vitro (Pitton C 1988) e, in un
modello animale di rinite allergica, il testosterone ha evidenziato un effetto inibitorio nella
produzione di IgE. In vivo, non sono state dimostrate differenze di genere tra i livelli di
testosterone e i risultati dei test cutanei positivi o la presenza di malattie atopiche.(Uekert 2006)
Androgeni ed estrogeni esercitano inoltre una significativa influenza sulla salute e il
benessere della superficie oculare e degli annessi oculari. Gli steroidi sessuali agiscono
modulando molteplici aspetti anatomici e fisiologici della ghiandola lacrimale e del Meibomio,di
congiuntiva cornea. Si ritiene che gli steroidi sessuali siano coinvolti nello sviluppo e/o la
progressione di molte patologie del segmento anteriore, come l’occhio secco, intolleranza alle
lenti a contatto, le cheratocongiuntiviti allergiche, la neoangiogenesi corneale, malattie
autoimmuni. (Sullivan D 2004)
È opinione ormai accettata che il meccanismo d’azione degli steroidi sessuali a livello
oculare sia dovuto prevalentemente alla formazione locale -intracrina- di androgeni e estrogeni
da precursori ghiandola surrenale, quali il DHEA, il DHEA-S e l’androstenedione. Infatti, gli
esseri umani ei primati sono gli unici in possesso di ghiandole surrenali, che secernono DHEA e
DHEA-S, che vengono poi convertiti in potenti androgeni, quali, il testosterone e il
diidrotestosterone (DHT) ed estrogeni dagli enzimi della steroidogenesi a livello periferico.
(Labrie F 1995)
Questo processo consente agli organi bersaglio di aggiustare la sintesi e il metabolismo
degli steroidi sessuali in base alla necessità locale. (Figura 4)
15
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Figura 4 Enzimi steroidogenici unami nei tessuti periferici intracrini. (Labrie 1998)
Un recente lavoro ha evidenziato che le cellule della superficie oculare e degli annessi
oculari esprimono l'RNA messaggero degli enzimi necessari alla sintesi e il metabolismo degli
steroidi sessuali e dei recettori degli androgeni evidenziando come i tessuti oculari siano
bersaglio dell’azione degli androgeni.(Schirra F. 2006, Rocha EM 2000)
3.3 Studio preliminare sul ruolo degli ormoni sessuali nella patogenesi della VKC
I livelli sierici dei principali ormoni sessuali (LH, FSH, E1, E2, progesterone, DHEA,
DHEA-S, testosterone totale, testosterone libero, DHT, SHBG) sono stati valutati in 14 bambini
pre-puberi (maschi, età <11 anni, LH<1 UI/l, Testosterone <200 ng/100 ml) con VKC (età media
7,3±2,5 anni) e paragonati ad un gruppo di controllo (N=74, età media 8,3±1,8anni) con le stesse
caratteristiche di età e sesso (maschi, età <11 anni, LH<1 UI/l, Testosterone <200 ng/100 ml).
I nostri dati preliminari mostrano un aumento significativo dei livelli sierici di DHEA-S
(p=0,002), Estrone (p=0,005) e Testosterone libero (p=0,001) e una riduzione significativa di
DHT (p=0.001) e della sex hormones binding globulin (SHBH) (p=0,004) rispetto ai controlli.
(Fugura 5)
16
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Tali risultati evidenziano una disregolazione degli ormoni sessuali nei bambini con VKC,
con una riduzione del DHT, il maggiore ormone androgeno attivo in età pre-pubere, che
potrebbe contribuire alla patogenesi della malattia.
Figura 5. I bambini con VKC mostrano un aumento significativo dei livelli sierici di
DHEA-S, Estrone e Testosterone libero e una riduzione significativa di DHT e SHBH
rispetto ai controlli.
Inoltre, dati preliminari derivanti dal microarray effettuato su citologie ad impressione
congiuntivale in bambini con VKC (n=3), mostrano una alterazione anche a livello locale
17
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
dell’espressione della SHBG, che risulta ridotta a livello congiuntivale, rispetto ai controlli sani
(n=3). Mostrano inoltre un aumento dell’espressione del 17-beta-steroido-deidrogenasi 2 (17BHSD-2) e una riduzione dell’espressione della 5-alfa-reduttasi 3, che partecipa al metabolismo
del DHT. Tali dati, se confermati dalla real-time PCR, mostrerebbero un impairment del tono
androgenico a livello locale nelle VKC.
18
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
4. Fisiopatologia
Nonostante la familiarità per atopia, i livelli sierici di IgE totali e specifiche, il numero
più elevato di mastociti ed eosinofili, e la risposta favorevole alla terapia anti-allergica - tutte
caratteristiche delle malattie allergiche - siano state osservate anche nella VKC (Bielory 1992;
Abelson 1993), la patogenesi di questa malattia sicuramente molto più complessa di una
semplice reazione di ipersisensibilitàdi tipo I. infatti, circa il50% dei pazienti con VKC presenta
negatività ai test allergometrici cutanei (Bonini et al. 2000). La forte abbondanza di citochine
Th2, l'aumentata espressione dei loro recettori e la scarsità di cellule T helper di tipo 1 (Th1)
nelle lacrime e nel siero di pazienti con VKC confermano il ruolo cruciale svolto dalla risposta
Th2 nell'insorgenza e la perpetuazione dell’ infiammazione osservata nella VKC. Inoltre, il
sistema immunitario, sistema nervoso ed endocrino sembrano interagire uno con l'altro nella
patogenesi della VKC (Bonini et al. 2004).
4.1 Mediatori nella VKC
Citochine e chemochine
Le cellule T helper (CD4), i mastociti e gli eosinofili che infiltrano la congiuntiva nella
VKC sono le principali fonti di citochine in questa malattia. In particolare, le cellule T isolate a
livello congiuntivale nella VKC mostrano un profilo Th2 (Calder et al. 1999). I livelli di
citochine Th2, vale a dire IL-4 e IL-5, sono stati trovati elevati nei pazienti VKC (Calder et al.
1999; Leonardi et al. 1999a). Inoltre, un aumento dell’ espressione di mRNA per le citochine di
tipo Th2 è stata osservata a livello tissutale delle VKC (Metz et al. 1997). I livelli sierici di IL-4
e i livelli lacrimali di IL-4 e IL -5 sono più elevati nei pazienti con VKC rispetto ai controlli. È
interessante notare che, IL-2, interferone (IFN)-gamma e fattore di necrosi tumorale (TNF)-beta,
le principali citochine secrete da Th1, non sono aumentate nella VKC (Leonardi, 2002°, Bonini
2003). Questi risultati confermano che VKC ha principalmente un profilo di tipo Th2 (Uchio et
19
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
al.2000; Fujishima et al. 2002).
Le chemochine (CC), sono potenti attivatori e chemioattrattanti, sono prodotte non solo
dalle cellule infiammatorie, ma anche da cellule epiteliali attivate, fibroblasti e cellule endoteliali
vascolari nella congiuntiva. Le chemochine sono coinvolti nel normale traffico e reclutamento
dei leucociti durante la risposta infiammatoria. Le chemochine sono raggruppate in sottofamiglie
dette CXC, CC, C e CX3C (Abu El-Asrar et al. 2001a). Elevati livelli di eotassina sono stati
trovati nel muco dai pazienti VKC, inoltre, i livelli eotassina correlavano significativamente con
la percentuale di eosinofili nelle lacrime questo suggerisce che l’eotassina possa essere
responsabile del reclutamento degli eosinofili nella VKC (Leonardi et al. 2003a). L’eotassina,
associata a MCP e RANTES, sono altamente espressi nei tessuti limbari e possono essere
responsabili della massiccia infiltrazione degli eosinofili nella VKC.
L’IL-8 è attivamente secreta dai macrofagi e dalle cellule epiteliali nella VKC è un
chemoattrattante e un attivatore di polimorfonucleati. Essa svolge un ruolo cruciale nella la
migrazione delle cellule infiammatorie, quali polimorfonucleati ed eosinofili (Miyoshi 2001).Il
recettore delle chemiochine (CXCR) -3 è anche notevolmente aumentato ed espresso
abbondantemente sui linfociti T nella congiuntiva dei pazienti VKC attiva, suggerendo un ruolo
nella regolazione del reclutamento di linfociti nella congiuntiva dei pazienti con VKC (Abu ElAsrar et al. 2001a).
Mediatori infiammatori
L’Istamina è un importante mediatore infiammatorio nelle congiuntivit allergiche,
rilasciata da mastociti e basofili attivati. La concentrazione lacrimale di istamina è aumentata nei
pazienti con VKC rispetto ai controlli sani (Abelson et al. 1980). Inoltre, i pazienti con VKC
dimostrano una iper-reattività congiuntivale non-specifica se provocati con test di provocazione
congiuntivale con istamina (Bonini et al. 1992a).
Anche le Metalloproteinasi (MMP) e gli inibitori delle MMP (TIMP) sono coinvolti
nella patogenesi della VKC, i livelli lacrimali di pro-MMP-1 e pro-MMP-9 sono
20
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
significativamente aumentati nei pazienti con VKC rispetto ai soggetti di controllo. L’attività di
MMP-9 è correlata in modo significativo con il coinvolgimento della cornea e la formazione
delle papille giganti (Leonardi et al. 2003b,c).
Fattori di crescita
Diversi fattori di crescita, come il fattore di crescita epidermica(EGF), il fattore di
crescita dei fibroblasti (FGF), il Trasformingrowth factor beta-1 (TGFb-1) sono stati aumentati
nella VKC. Questi fattori inducono la crescita dei fibroblasti e la produzione di procollagene
(Leonardi et al. 1998). Recentemente, i recettori per il fattore di crescita nervoso (NGF) sono
stati dimostrati nella congiuntiva dei pazienti con VKC attiva. Alti livelli plasmatici del NGF
sono stati descritti nella VKC in correlazione con il numero di mastociti congiuntivali,
suggerendo che i fattori neurali possono avere un ruolo nella patogenesi della VKC (Lambiase et
al. 1995). È interessante notare che, la sostanza P - un neuropeptide con ben nota attività su
cellule del sistema immunitario -è aumentata nel plasma e nelle lacrime dei pazienti con VKC
(Fujishima et al. 1997; Lambiase et al. 1997).
4.2 Cellule nella VKC
I mastociti, le cellule T, gli eosinofili e i macrofagi sono coinvolti nella patogenesi della
VKC. I mastociti sono una caratteristica costante nei tessuti congiuntivali della VKC. Il
notevolmente aumento del numero dei mastociti trovati in campioni di papille giganti tarsali
suggerisce un ruolo attivo di queste cellule nell’anomalo metabolismo del tessuto connettivo
osservato nella VKC. Queste cellule esprimono Fc [epsilon] RI sulla loro superficie cellulare,
che consente loro di legare le IgE (Church 1997). Il legame con le IgE specifiche per allergeni
risultati nel rilascio di mediatori pro-infiammatori, quali istamina, proteasi, prostaglandine D2e
leucotrieni C4. Questi mediatori sono responsabili del prurito, iperemia, lacrimazione e chemosi
nelle congiuntiviti allergiche (Church 1997). I mastociti liberano anche citochine, tra cui IL-4.
Le citochine liberate dai mastociti sono responsabili dell'avvio dell’ infiammazione allergica, con
21
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
conseguente infiltrazione di eosinofili. IL-4 svolge un ruolo chiave dell'infiammazione allergica
attraverso l’attivazione e la crescita delle cellule T, l'induzione della produzione di IgE dalle
cellule B, l'aumento di molecole di adesione e la modulazione della differenziazione di tipo Th2,
che è essenziale per la reazione allergica. (Fukagawa et al. 2000). Triptasi e chimasi, indicatori
dell'attivazione dei mastociti, sono aumentati nelle lacrime delle VKC e sono stati proposti come
markers di severità della VKC (Tabbara 2001).
Gli eosinofili sono una caratteristica costante nelle lacrimale e nella citologia
congiuntivale delle VKC. Infatti, circa il 50-90% delle cellule nelle lacrime durante la fase attiva
della VKC sono eosinofili (Leonardi, 2002a). Gli eosinofili, insieme con i mastociti, sono le
principali cellule effettrici dell’infiammazione oculare nella VKC e risultano aumentati in modo
significativo nelle lacrime, nella circolazione periferica e nei tessuti congiuntivale provenienti da
pazienti con VKC. (Trocmé et al.1989, 1993; Leonardi et al. 1995). Gli eosinofili attivati
rilasciano citochine, chemochine, leucotrieni e proteine come MBP, ECP, la per ossidasi
eosinofila (EPO) e la proteina eosinofila X / neurotossina (EPX) (Tomassini et al. 1994;
Leonardi 2002a). I livelli sierici e lacrimali di ECP e EPX sono più alti in pazienti VKC rispetto
ai soggetti normali (Bonini et al. 1992a). I livelli di ECP lacrimale correlano positivamente con
segni clinici e sintomi e si riducono dopo trattamento con desametasone o ciclosporina
(Leonardi et al. 1995).
Anche il numero di linfociti T è aumentato nella congiuntiva dei pazienti con VKC.
L'attivazione di questi linfociti sembra giocare un ruolo vitale nella patogenesi della VKC. I
cloni di cellule T derivate da tessuti di VKC sono principalmente di tipo Th2 (Leonardi et al.
1999a). I linfociti Th2, in virtù del loro profilo di citochine, sono responsabili dell’aumento della
produzione di IgE, del reclutamento e l'attivazione di mastocic e eosinofili (Umetsu 1997;
Bielory et al. 2002a)
Un nostro lavoro, ha recentemente dimostrato un aumento delle cellule natural killer
nella congiuntiva dei pazienti con VKC, suggerendo un ruolo di queste cellule e dell’ immunità
22
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
innata nella VKC. (Lambiase 2007-lavoro allegato, Bonini 2005)
Cellule epiteliali
E 'stato dimostrato che le cellule epiteliali congiuntivali non costuiscono solo una barriera
meccanica, ma partecipano all’infiammazione esprimendo antigeni di superficie come ad
esempio le molecole di adesione (ICAM-1, VCAM-1 e HLADR) e rilasciando citochine
(eotassina, IL-8, IL-6, RANTES). È stato ipotizzato che l’istamina rilasciata dai mastociti
congiuntivali, potrebbe stimolare la sintesi di IL-6 e IL-8 dalla cellule epiteliali congiuntivali e
contribuire ad amplificare la risposta allergica (Irkec 2003).
Anche i fibroblasti di cornea e congiuntiva contribuiscono alla induzione e
amplificazione dell’ infiammazione allergica oculare così come al rimodellamento del tessuto.
TGFb-1, IL-1 e le citochine prodotte dalle cellule Th2 inducono la produzione di VEGF da parte
dei fibroblasti congiuntivali, che possono svolgere un ruolo cruciale nella neovascolarizzazione e
nella formazione delle papille giganti (Asano-Kato et al. 2005).
23
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
5. Trattamento della cheratocongiuntivite primaverile
Poiché la VKC è una malattia cronica, e recidivante la gestione del paziente è piuttosto
impegnativa. L'esposizione a stimoli non-specifici come sole, vento e acqua può provocare
arrossamento congiuntivale frequenti tra i pazienti VKC, evitare i fattori scatenanti, è
complicato e comunque non sufficiente per controllare i sintomi. L’applicazione di impacchi
freddi e l'uso di lacrime artificiali hanno dimostrato di essere efficaci nel sollievo dei sintomi
(Bielory 2002b).
La varietà dei farmaci attualmente disponibili per il trattamento della VKC include l’uso
di antistaminici, stabilizzatori mastocitari, agenti multiazione, corticosteroidi e
immunomodulatori ma, a tutt’oggi, non ci sono terapie in grado di agire sui molteplici aspetti
della fisiopatologia della VKC. Infatti, la maggior parte dei farmaci utilizzati sono palliativi e
non specifici volti a trattare i sintomi o a deprimere la risposta immunitaria in toto senza agire
sulla complessa risposta immunitaria, per cui quando la terapia viene interrotta vi è spesso una
recidiva della malattia.
Perché ci sono pochi studi randomizzati e controllati la selezione di un farmaco tra le molte
opzioni disponibili è per lo più sulla base dell'esperienza personale e la preferenza del medico
curante. Una meta-analisi di studi randomizzati controllati ha infatti evidenziato come ci siano
scarse evidenze per raccomandare uno specifico farmaco, e come ci sia anche una mancanza di
criteri standardizzati di trattamento basati sulla diagnosi e la stadiazione della severità. (Mantelli
2007)
A tale scopo, ci siamo proposti di creare una stadiazione della severità e dell’attività della
VKC utilizzando un metodo di analisi dei dati che ci consentisse di ricavare un albero
decisionale, di semplice e immediata interpretazione nalla pratica clinica. Per far ciò, uno studio
retrospettivo su 207 casi di VKC è stato effettuato, i dati sono stati analizzati con il metodo
CART®, al fine di ricavare un algoritmo decisionale, di proporre una stadiazione della severità e
24
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
individuare i fattori di rischio per un peggiore esito visivo (Sacchetti M 2010-IN PRESS-lavoro
allegato).
I colliri contenenti antiistaminici vengono spesso utilizzati dai pazienti durante a primi
stadi della malattia, come trattamento di prima linea. Questi sono in grado di alleviare il prurito.
Gli antistaminici H1- selettivi, qauli emedastina e levocabastina, sono efficaci nel controllo dei
segni e sintomi della VKC live e moderata. (Bielory et al. 2005).
Gli stabilizzatori di membrana inibiscono la degranulazione dei mastociti che è un evento
centrale nella VKC. I mediatori rilasciati dai mastociti, infatti, sono responsabili di molti
sintomi e segni associati VKC. Tali farmaci sono quindi in grado di alleviare i sintomi acuti della
malattia attiva e anche di ridurre lo stimolo per lo sviluppo dell’ infiammazione allergica cronica
(Church 2002).
L'efficacia del sodio cromoglicato (QID), lodoxamide (qid), Nedocromil (bid) e pemirolast
(QID) nel controllo dei sintomi e nella prevenzione dell’esacerbazione è stato dimostrato da
molti studi (Tabbara 1977; Bonini et al. 1992b). Questi farmaci dovrebbero essere usati come
trattamento di prima scelta al momento della comparsa delle manifestazioni allergiche stagionali
e dovrebbe essere usato continuo per tutta la stagione.
Gli antistaminici sistemici possono essere una buona scelta quando allergia coinvolge gli occhi,
il naso o faringe simultaneamente. Non trovano invece indicazione quando l’allergia è limitata
agli occhi, il trattamento con farmaci antistaminici topici è efficace e privo di effetti indesiderati.
Recentemente, una nuova generazione di farmaci antiistaminici multiazione,come
l’Olopatadina, l’Epinastine, il Ketotifene e l’Azelastina hanno dimostrato la duplice azione di
stabilizzatori di membrana e antagonismo del recettore H1. L'azione di questi farmaci non è
limitata ai mastociti, al blocco dei recettori H1, essi esercitano anche un’azione antiinfiammatoria attraverso diversi meccanismi quali l’inibizione del rilascio di TNF-alfa e di varie
citochine da parte dell’epitelialio congiuntivale e delle cellule infiammatorie, in modo da
controllare l’infiammazione in modo più efficace rispetto ai soli antiistaminici (Lambiase 2009).
25
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
L’uso degli anti-infiammatori non steroide (FANS) in collirio, quali il ketorolac e il
diclofenac hanno dimostrato di diminuire prurito oculare e congiuntivale e l’iperemia associata
alle congiuntiviti allergiche. (D'Angelo et al. 2003, Kosrirukvongs 2004).
I corticosteroidi topici sono i farmaci più efficaci farmaci per il controllo dei segni e sintomi
della VKC. A causa delle complicazioni associate al loro uso prolungato, questi non dovrebbero
essere prescritta come trattamento di prima linea. Infatti, il trattamento prolungato con
corticosteroidi può causare effetti collaterali gravi e permanenti quali cataratta e glaucoma e
aumentare la suscettibilità alle infezioni virali e da funghi. (Tabbara 1995, Bonini 2000)
La Ciclosporina A topica, è stata proposta per il trattamento della VKC per ridurre i segni e i
sintomi della VKC in numero studi clinici in aperto. La ciclosporina blocca la proliferazione dei
linfociti Th2 e la produzione di IL-2. Inoltre, inibisce il rilascio di istamina attraverso una
riduzione della produzione di IL-5 (Ben - Ezra et al. 1988; Secchi et al. 1990). Ben Ezra et al.
(1986) ha descritto l’uso di ciclosporina collirio 2% per il trattamento di gravi VKC quasi due
decenni fa, riportando efficacia nel sollievo dei sintomi soggettivi nell’ 86% dei pazienti trattati.
Un altro studio, il trattamento topico con Ciclosporina (0,5-2%) in emulsione di olio d'oliva o di
ricino, instillata quattro volte al giorno, ha dimostrato essere efficace nel trattamento della VKC.
(Abu El-Asrar et al. 1996). Alcuni studi in doppio cieco, controllati con placebo hanno
dimostrato che la ciclosporina (2%) in collirio è efficace e sicura nel trattamento delle VKC
severe (Bleik JH 1991, Pucci et al. 2002; Kilic 2006). In uno studio prospettico in aperto, su 10
casi VKC severa, il trattamento con ciclosporina topica (2%) ha ridotto significativamente gli
score dei segni clinici e dei sintomi. Dopo il trattamento è stata inoltre osservata la riduzione
della popolazione di cellule CD4 e di CD28 congiuntivali. (Avudunk et al. 2001). La
Ciclosporina a concentrazioni inferiori 0,05% e 1% è stata anche utilizzata nel trattamento delle
VKC, ma le evidenze disponibili sono ancora scarse per trarre conclusioni sull’efficacia.
(Kosrirukvongs 2004, Spadavecchia et al. 2006).
26
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
5.1 Studio multicentrico randomizzato controllato in doppio cieco per la valutazione
dell’efficacia del trattamento con ciclosporina A in collrio nella prevenzione delle recidive
dell’infiammazione nella VKC
Uno studio della durata di 2 anni, in doppio cieco, multicentrico, randomizzato,
controllato con cross-over è stato effettuato presso il nostro centro per valutare l’efficacia del
trattamento con Ciclosporina nella prevenzione delle recidive della VKC e nel trattamento delle
fasi acute della malattia.
L’obiettivo primario studio era valutare la differenza nel numero di recidive di
infiammazione oculare tra i gruppi di pazienti trattati con ciclosporina e ketotifene. Inoltre, le
differenze di sintomi e segni tra i due gruppi sono stati valutati ad ogni visita.
Metodi: Trentaquattro pazienti con VKC (30M e 4F, età media 14±7anni)sono stati
inclusi nello studio e trattati in doppio cieco con ciclosporina senza conservanti 0,05% in
emulsione cationica (N=16) o ketotifene 0,025% soluzione oftalmica (N=18) due volte al giorno
per 6 mesi da marzo a ottobre. Nel secondo anno di studio, i pazienti sono stati inclusi per sei
mesi (da Marzo a Ottobre) in cross-over: i pazienti precedentemente trattati con ciclosporina
hanno ricevuto ketotifene (N=15) e i pazienti precedentemente trattati con ketotifene hanno
ricevuto ciclosporina (N=15).
I pazienti sono stati valutati con un esame oculare completo, i segni (iperemia,
secrezione, del tarso e / o papille limbal, Trantas punti, congiuntivale fibrosi, cheratite puntata
superficiale, ulcera corneale e vasi della cornea) e i sintomi (prurito, fotofobia, arrossamento,
lacrimazione, secrezione e la riduzione della visione) sono stati valutati e un punteggio da 0 a 3 è
stato assegnato (0 = assente, 1 = lieve, 2 = moderata, 3 = grave) al basale, dopo 12 settimane di
trattamento, dopo 3 mesi e alla fine del trattamento (6 mesi). Ulteriori visite sono state effettuate
in caso di recidive della malattia durante il periodo dello studio. L’Oxford score è stato anche
valutato ad ogni visita.
27
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Il test Anova e la regressione lineare sono stati effettuati per valutare la differenza tra il
numero di recidive nei gruppi trattati la ciclosporina (CsA) vs ketotifene. La curva di
sopravvivenza di Kaplan-Meier e le stime di rischio sono stati eseguiti per valutare le differenze
nell’obiettivo primario (numero di recidive VKC). Il modello lineare generalizzato per misure
ripetute è stato utilizzato per valutare le differenze di segni e sintomi tra i due gruppi.
Risultati: Nel primo anno dello studio, tre pazienti hanno abbandonato lo studio, a causa
di una reazione avversa (n=1, trattata con CsA),e di inefficacia della terapia con scarso controllo
dell'infiammazione (n=2 trattati con ketotifene). Nel secondo anno di studio, i pazienti sono stati
trattati in cross-over. In totale 30 pazienti (un paziente ha abbandonato lo studio prima di iniziare
il trattamento per mancanza di compliance) sono stati trattatti CSA-(n = 15) o Ketotifene (n =
15). Durante il secondo anno dello studio, 5 pazienti sono usciti dallo studio per inefficacia del
trattamento (4 nel grppo trattato con ketotifenee 1 nel gruppo trattato con CsA).
Considerando tutti i pazienti abbiamo osservato in tutto 49 esacerbazioni, 15 in pazienti
trattati con CsA e 34 in pazienti trattati con ketotifene. L'analisi statistica ha mostrato una
differenza statisticamente significativa nel numero di riacutizzazioni della VKC tra i due gruppi
di trattamento, indicando che i pazienti trattati con CsA avevano un numero significativamente
inferiore di riacutizzazioni rispetto ai pazienti trattati con ketotifene (p <0,05). Inoltre, di un
minor numero di pazienti ha sviluppato recidive (10 nel gruppo ciclosporina vs 18 nel gruppo
Ketotitifene) e un minor numero di pazienti con ha sviluppato più di una recidiva (9% nel gruppo
ciclosporina vs 33% ketotifene). I pazienti trattati con ketotifene hanno mostrato un rischio di
recidiva 2,4 volte superiore rispetto ai pazienti trattati con CsA. Infine, il trattamento con CsA ha
garantito un più lungo intervallo libero da malattia. (Figura 6)
28
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Figura 6.Il trattamento con CsA ha consentito di ridurre significativamente il
numero di riacutizzazioni rispetto al trattamento con ketotifene (A, B). Il pazienti trattati
con ketotifene hanno mostrato un rischio di recidiva 2,4 volte superiore rispetto alla CsA
(C). Il trattamento con CsA ha garantito un più lungo intervallo libero da malattia. (D)
Inoltre, l'analisi statistica ha evidenziato che il trattamento con ciclosporina A 0,05% è
più efficace del trattamento con ketotifene nel controllare tutti i sintomi valutati: prurito (p =
0.003), fotofobia (p = 0.023), secrezione (p = 0.002), lacrimazione (p = 0.045), arrossamento (p
= 0,016)e score totalae die sintomi (TSYS) (p = 0,045) e solo uno dei segni valutati (secrezione
mucosa; p = 0,041). (Figura 7,8)
29
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Figura 7. Il trattamento con ciclosporina A 0,05% è più efficace del trattamento con
ketotifene nel controllare tutti i sintomi valutati: prurito (A), fotofobia (B), secrezione (C),
lacrimazione (D), arrossamento (E)e score totalae dei sintomi (F).
30
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Figura 8. La Ciclosporina A in collirio è risultata più efficace nel controllo dei segni
come la secrezione mucosa (A) rispetto al Ketotifene in collirio, ma non degli altri segni
valutati: iperemia (B), papille limbari e tarsali (C, D), total score dei segni(E) e Oxford
score (F).
Nessuna differenza significativa è stata osservata in dell'acuità visiva e la pressione
intraoculare tra i due gruppi di pazienti
5.2 Studio aggiuntivo per valutare l’efficacia della ciclosporina per il trattamento delle
fasi acute della VKC.
In caso di recidiva di VKC i pazienti sono stati inclusi in questo studio aggiuntivo per valutare
l'efficacia della ciclosporina 1% vs il trattamento standard, con steroide topico (Etacortilen ®
0,15%, Sifi) per il trattamento delle infiammazioni allergiche acute.
31
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
L'obiettivo di questo studio era di confrontare gli effetti clinici della ciclosporina vs
trattamento con steroidi.
Metodi: Questo studio è stato condotto in doppio cieco, randomizzato e controllato.
Quando una ricaduta di VKC è stato confermato dal medico (con un incremento di almeno il
100% della somma di iperemia, prurito e punteggi lesione corneale rispetto al basale dei valori),
tutti i segni e sintomi clinici sono stati registrati. A seguito di randomizzazione (1:1), i pazienti
hanno ricevuto ciclosporina 1% o steroide topico quattro volte al dì per 7 giorni. Una volta che
raggiunta la remissione della fase acuta, il trattamento è stato sospeso e tutti i segni e sintomi
clinici sono stati registrati. La remissione è stata definita come riduzione di almeno il 100% della
somma di iperemia e prurito e punteggi lesione corneale rispetto ai valori di fase acuta. Se la
remissione non è stata ottenuta dopo 7 giorni di trattamento, i paziente sono stati considerati
"non responder" e trattati con steroidi topici 4 volte al giorno per 7 giorni (rescue medication).
Dopo la remissione della fase acuta, i pazienti, ancora una volta iniziato il trattamento precedente
(0,05% ciclosporina o fumarato ketotifene 0,025%).
Il Test Chi quadrato è stato eseguito per confrontare il numero di pazienti che hanno
ricevuto il trattamento rescue nel gruppo CsA versus gruppo di steroidi. Gli score dei sintomi e
dei segni sono stati anche analizzati con modello lineare generalizzato per misure ripetute, per
valutare le differenze tra i trattamenti con CsA 0,1% e del 0,15%.
Risultat: Venti recidive di infiammazione acuta hanno richiesto il ricorso al trattamento
rescue con desametasone 0,15% 4 volte al giorno per 7 giorni, secondo quanto previsto dal
protocollo dello studio. In particolare è stato necessario amministrare il trattamento rescue in 16
pazienti che hanno ricevuto il trattamento con CsA e in 7 trattati con steroidi (p <0,029). (Figura
9)
32
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Figura 9 I pazienti con riacutzzazione trattati con CsA 0,1% hanno richiesto un
numero maggiore di rescue medication rispetto ai pazienti trattati con desametazone (A,B)
Allo stesso modo, i pazienti trattato con desametasone hanno mostrato un miglioramento
significativo del prurito (p = 0,037), dell’ iperemia congiuntivale (p = 0,009) e del total score dei
segni (p = 0,038) rispetto ai pazienti trattati con CsA 0,1%. (Figura 10)
33
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Figura 10. il trattamento con desametazone è risultato più efficace nel controllo del
prurito(A), iperemia(B), total score dei segni (C) rispetto al trattamento con CsA 0.1%, ma
non ha raggiunto la significatività nel total score dei sintomi (D), nell’Oxford score (E) e
negli altri parametri valutati.
Questo studio ha dimostrato con il trattamento con CsA 0,05% consente una riduzione
significativa delle recidive stagionali di infiammazione oculare nei pazienti con VKC, rispetto al
34
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
trattamento standard con collirio antiallergico (Ketotifene 0,025%). I risultati di questo studio
suggeriscono che la ciclosporina in collirio può essere utilizzata nei pazienti con VKC come
trattamento preventivo delle riacutizzazioni che consenta un risparmio nell’uso degli steroidi.
Nelle fasi di acuzie, invece, il trattamento più efficace resta quello steroideo topico, usato ad alte
dosi per brevi periodi.
5.3 Trattamento chirurgico della cheratocongiuntivite primaverile
Sebbene sia stato proposto il trattamento delle papille giganti con l’escissione chirurgica, la sua
efficacia non è stata dimostrata, e la rapida ricomparsa della reazione papillare rende inutile tale
chirurgia. Anche la crioterapia delle papille giganti è da sconsigliare in quanto promuove
l'infiammazione e può causare cicatrici congiuntivali. (Tanaka et al. 2004).
Differente è l’approccio ai pazienti che hanno sviluppato una ulcera corneale a placca, in cui la
rimozione chirurgica della placca è necessaria per ottenere la riepitelizzazione della ulcera a
scudo ulcera. (Solomon et al. 2004).
Anche l’innesto di membrana amniotica è stato descritto in pazienti con ulcere persistenti
refrattarie alla terapia medica, al fine di favorire la riepitelizzazione (Rouher et al. 2004).
35
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
6. Conclusioni
Nonostante lo sviluppo di nuovi farmaci nel corso dell'ultimo decennio, al momento, la
situazione dei pazienti con VKC severa rimane preoccupante per la dipendenza da steroidi topici,
con tutti i rischi che ne conseguono. Nuovi e selettivi farmaci sono necessari per un miglior
controllo della VKC. (Hingorani1995). Finora, i risultati di attualità ciclosporina sono molto
incoraggianti, ma a causa della indisponibilità dei preparazioni commerciali, il suo uso in VKC è
limitato. Gli sviluppi futuri nella modulazione di prodotti eosinofili, citochine e molecole di
adesione potranno essere rilevanti. La dimostrazione di alti livelli di leucotrieni nelle lacrime di
pazienti con VKC e del miglioramento nei segni e sintomi della VKC quando viene
somministrato per via orale montelukast, un antagonista del recettore dei leucotrieni, suggerisce
che gli anti-leucotrieni hanno potenziale terapeutico e la necessità di ulteriori studi (Akman et al.
1998; Lambiase et al. 2003). Anche molecole probiotiche sono state proposte per inibire le
allergie oculari. Uno studio preliminare ha dimostrato che il trattamento con Lactobacillus
acidophilus diluito in soluzione fisiologica somministrata come collirio migliora i segni ed i
sintomi nei pazienti con VKC. (Iovieno 2008-lavoro allegato)
36
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
7. Bibliografia
Abelson MB , Schaefer K (1993): Conjunctivitis of allergic origin: immunologic mechanisms
and current approaches to therapy.Surv Ophthalmol 38: 115–132.
Abelson MB, Baird RS , Allansmith MR (1980): Tear histamine levels in vernal conjunctivitis
and other ocular inflammations. Ophthalmology 87: 812–814.
Abu El-Asrar AM, Struyf S, Al-Mosallama AA, Missotten L, Van Damme J , Geboes K (2001):
Expression of chemokine receptors in vernal keratoconjunctivitis. Br J Ophthalmol 85: 1357–
1361.
Abu El-Asrar AM, Tabbara KF, Geboes K, Missotten L , Desmet V (1996): An
immunohistochemical study of topical cyclosporine in vernal keratoconjunctivitis. Am J
Ophthalmol 121: 156–161.
Akman A, Irkec M , Orhan M (1998):Effects of lodoxamide, disodium cromoglycateand
fluorometholone on tear leukotrienelevels in vernal keratoconjunctivitis.Eye 12: 291–295.
Allansmith MR , Ross RN (1988): Ocular allergy. Clin Allergy 18: 1–136.
Asano-Kato N, Fukagawa K, Okada N, Kawakita T, Takano Y, Dogru M, Tsubota K , Fujishima
H (2005): TGF-beta1, IL-1beta, and Th2 cytokines stimulate vascular endothelial growth factor
production from conjunctival fibroblasts. Exp Eye Res 80: 555–560.
Avunduk AM, Avunduk MC, Erdol H, Kapicioglu Z , Akyol N (2001): Cyclosporine effects on
clinical findings and impression cytology specimens in severe vernal keratoconjunctivitis.
Ophthalmologica 215: 290–293.
37
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
BenEzra D, Pe’er J, Brodsky M , Cohen E (1986): Cyclosporine eye drops for the treatment of
severe vernal keratoconjunctivitis. Am J Ophthalmol 101: 278– 282.
BenEzra D, Matamoros N , Cohen E (1988): Treatment of severe vernal keratoconjunctivitis
with cyclosporine A eyedrops. Transplant Proc 20: 644–649.
Bielory L (2000): Allergic and immunologic disorder of the eye. Part 2: ocular allergy. J Allergy
Clin Immunol 106: 1019–1032.
Bielory L (2002b): Ocular allergy guidelines: a practical treatment algorithm. Drugs 62:1611–
1634.
Bielory L , Frohman LP (1992): Allergic and immunologic disorders of the eye. J Allergy Clin
Immunol 89: 1–15.
Bielory L, Bonini S , Bonini S (2002a): Inflammatory mechanism in allergic diseases.
In: Zweiman B , Schwartz LB (eds). Allergic eye disorders. New York: Marcel Dekker, 311–
323.
Bielory L, Lien KW , Bigelsen S (2005): Efficacy and tolerability of newer antihistaminesin the
treatment of allergic conjunctivitis. Drugs 65: 215–228.
Bleik JH, Tabbara KF.Topical cyclosporine in vernal keratoconjunctivitis.(1991)
Ophthalmology;98(11):1679-84.
Bonini S, Bonini S, Schiavone M, Centofanti M, Allansmith MR , Bucci MG (1992a):
Conjunctival hyperresponsiveness to ocular histamine challenge in patients with vernal
conjunctivitis. J Allergy Clin Immunol 89: 103–107.
38
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Bonini S, Barney NP, Schiavone M, Centofanti M, Berruto A, Bonini S , Allansmith MR
(1992b): Effectiveness of Nedocromil sodium 2% eyedrops on clinical symptoms and tear fluid
cytology of patients with vernal conjunctivitis. Eye 6: 648–652.
Bonini S, Bonini S, Lambiase A et al. (1995a): Vernal keratoconjunctivitis: a model of 5q
cytokine gene cluster disease.Int Arch Allergy Immunol 107: 95–98.
Bonini S, Lambiase A, Schiavone M, Centofanti M, Palma LA , Bonini S (1995b): Estrogen and
progesterone receptors in vernal keratoconjunctivitis. Ophthalmology 102: 1374–1379.
Bonini S, Bonini S, Lambiase A et al. (2000):Vernal keratoconjunctivitis revisited. A case series
of 195 patients with long-term followup. Ophthalmology 107: 1157–1163.
Bonini S, Lambiase A, Sacchetti M, Bonini S.(2003) Cytokines in ocular allergy. Int
Ophthalmol Clin;43(1):27-32.
Bonini S, Coassin M, Aronni S , Lambiase A (2004): Vernal keratoconjunctivitis. Eye 18: 345–
351.
Bonini S, Micera A, Iovieno A, Lambiase A, Bonini S. (2005) Expression of Toll-like receptors
in healthy and allergic conjunctiva. Ophthalmology112(9):1528;
Bonini S, Sacchetti M, Mantelli F , Lambiase A (2007): Clinical grading of vernal
keratoconjunctivitis. Curr Opin Allergy Clin Immunol 7: 436–441.
Buckley RJ (1988): Vernal keratoconjunctivitis.Int Ophthalmol Clin 28: 303–308.
Calder VL, Jolly G, Hingorani M, Adamson P, Leonardi A, Secchi AG, Buckley RJ ,Lightman S
(1999): Cytokine production and mRNA expression by conjunctival T-cell lines in chronic
allergic eye disease. Clin Exp Allergy 29: 1214–1222.
Cameron JA (1995): Shield ulcers and plaques of the cornea in vernal keratoconjunctivitis.
phthalmology 102: 985–993.
39
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Chen W, Mempel M, Schober W, Behrendt H, Ring J.Gender difference, sex hormones, and
immediate type hypersensitivity reactions.Allergy. 2008;63(11):1418-27.
Church MK , Levi-Schaffer F (1997): The human mast cell. J Allergy Clin Immunol 99: 155–
160.
Church MK , McGill JI (2002): Human ocular mast cells. Curr Opin Allergy Clin Immunol 2:
419–422.
Cutolo M, Sulli A, Capellino S, Villaggio B, Montagna P, Seriolo B et al. Sex hormones
influence on the immune system: basic and clinical aspects in autoimmunity. Lupus
2004;13:635–638
D’Angelo G, Lambiase A, Cortes M, Sgrulletta R, Pasqualetti R, Lamagna A , Bonini S (2003):
Preservative-free diclofenac sodium 0.1% for vernal keratoconjunctivitis. Graefes Arch Clin Exp
Ophthalmol 241: 192–195.
Fujishima H, Takeyama M, Takeuchi T, Saito I , Tsubota K (1997): Elevated levels of substance
P in tears of patients with allergic conjunctivitis and vernal keratoconjunctivitis. Clin Exp
Allergy 27:372–378.
Fujishima H, Saito I, Takeuchi T , Tsubota K (2002): Immunological characteristics of patients
with vernal keratoconjunctivitis. Jpn J Ophthalmol 46: 244–248.
Fukagawa K, Nakajima T, Saito H, Tsubota K, Shimmura S, Natori M , Hirai K (2000): IL-4
induces eotaxin production in corneal keratocytes but not in epithelial cells. Int Arch Allergy
Immunol 121: 144– 150.
Hingorani M , Lightman S (1995): Therapeuticoptions in ocular allergic disease.Drugs 50: 208–
221.
40
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Iovieno A, Lambiase A, Sacchetti M, Stampachiacchiere B, Micera A , Bonini S (2008):
Preliminary evidence of the efficacy of probiotic eye-drops treatment in patients with vernal
keratoconjunctivitis. Graefes Arch Clin Exp Ophthalmol 246: 435–441.
Iqbal A, Jan S, Babar TF , Khan MD (2003): Corneal complications of vernal catarrh. J Coll
Physicians Surg Pak 13: 394–397.
Irkec M , Bozkurt B (2003): Epithelial cells in ocular allergy. Curr Allergy Asthma Rep : 352–
357.
Kilic A , Gurler B (2006): Topical 2% cyclosporine A in preservative-free artificial tears for the
treatment of vernal keratoconjunctivitis. Can J Ophthalmol 41: 693–698.
Kosrirukvongs P , Luengchaichawange C (2004): Topical cyclosporine 0.5 per cent and
reservative-free ketorolac tromethamine 0.5 per cent in vernal keratoconjunctivitis. J Med Assoc
Thai 87:190–197.
Labrie F, Bélanger A, Simard J, Van Luu-The, Labrie C.DHEA and peripheral androgen and
estrogen formation: intracinology.Ann N Y Acad Sci. 1995;774:16-28
Lambiase A, Bonini S, Bonini S, Micera A, Magrini L, Bracci-Laudiero L , Aloe L (1995):
Increased plasma levels of nerve growth factor in vernal keratoconjunctivitis and relationship to
conjunctival mast cells. Invest Ophthalmol Vis Sci 36: 2127–2132.
Lambiase A, Bonini S, Micera A, Tirassa P, Magrini L, Bonini S , Aloe L (1997): Increased
plasma levels of substance P in vernal keratoconjunctivitis. Invest Ophthalmol Vis Sci 38: 2161–
2164.
Lambiase A, Bonini S, Rasi G, Coassin M,Bruscolini A , Bonini S (2003): Montelukast,a
leukotriene receptor antagonist,in vernal keratoconjuctivitis associatedwith asthma. Arch
Ophthalmol 121: 615–620.
41
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Lambiase A, Normando EM, Vitiello L et al. (2007): Natural killer cells in vernal
keratoconjunctivitis. Mol Vis 13: 1562–1567.
Lambiase A, Minchiotti S, Leonardi A, et al. (2009);Prospective, multicenter demographic and
epidemiological study on vernal keratoconjunctivitis: a glimpse of ocular surface in Italian
population.Ophthalmic Epidemiol. 16(1):38-41.
Lambiase A, Micera A, Bonini S.(2009)Multiple action agents and the eye: do they really
stabilize mast cells?Curr Opin Allergy Clin Immunol;9(5):454-65..
Leonardi A (2002a): Vernal keratoconjunctivitis: pathogenesis and treatment. Prog Retin Eye
Res 21: 319–339.
Leonardi A, Papa V, Milazzo G , Secchi AG (2002b): Efficacy and safety of desonide phosphate
for the treatment of allergic conjunctivitis. Cornea 21: 476–481.
Leonardi A, Borghesan F, Faggian D, Secchi A , Plebani M (1995): Eosinophil cationic protein
in tears of normal subjects and patients affected by vernal keratoconjunctivitis. Allergy 50: 610–
613.
Leonardi A, Borghesan F, DePaoli M, Plebani M , Secchi AG (1998): Procollagens and
inflammatory cytokine concentrations in tarsal and limbal vernal keratoconjunctivitis. Exp Eye
Res 67: 105–112.
Leonardi A, De Franchis G, Zancanaro F, et al (1999a): Identification of local Th2 and Th0
lymphocytes in vernal conjunctivitisby cytokine flow cytometry.Invest Ophthalmol Vis Sci 40:
3036–3040.
Leonardi A, Jose PJ, Zhan H , Calder VL (2003a): Tear and mucus eotaxin-1 and eotaxin-2 in
allergic keratoconjunctivitis.Ophthalmology 110: 487–492.
42
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Leonardi A, Cortivo R, Fregona I, Plebani M, Secchi AG , Abatangelo G (2003b): Effects of
Th2 cytokines on expression of collagen, MMP-1, and TIMP-1 in conjunctival fibroblasts. Invest
Ophthalmol Vis Sci 44: 183–189.
Leonardi A, Brun P, Abatangelo G, Plebani M , Secchi AG (2003c): Tear levels and activity of
matrix metalloproteinase (MMP)-1 and MMP-9 in vernal keratoconjunctivitis. Invest
Ophthalmol Vis Sci 44: 3052–3058.
Malkin CJ, Pugh PJ, Jones RD, Jones TH, Channer KS. Testosterone as a protective factor
against atherosclerosis-immunomodulation and influence upon plaque development and stability.
J Endocrinol 2003;178:373–380.
Mantelli F, Santos MS, Petitti T, Sgrulletta R, Cortes M, Lambiase A, Bonini S.
(2007)Systematic review and meta-analysis of randomised clinical trials on topical treatments
for vernal keratoconjunctivitis.Br J Ophthalmol.;91(12):1656-61.
Metz DP, Hingorani M, Calder VL, Buckley RJ , Lightman S (1997): T-cell cytokines in chronic
allergic eye disease. J Allergy Clin Immunol 100: 817–824.
Mitchell VL, Gershwin LJ. Progesterone and environmental tobacco smoke act synergistically to
exacerbate the development of allergic asthma in a mouse model. Clin Exp Allergy
2007;37:276–286.
Miyoshi T (2001): Interleukin-8 concentrations in conjunctival epithelium brush cytology
samples correlate with neutrophil, eosinophil infiltration, and corneal damage. Cornea 20: 743–
747.
Montan PG, Ekstrom K, Hedlin G, van Hage-Hamsten M, Hjern A , Herrmann B (1999): Vernal
keratoconjunctivitis in a Stockholm ophthalmic centre – epidemiological, functional, and
immunologic investigations. Acta Ophthalmol Scand 77: 559–563.
43
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Narita S, Goldblum RM, Watson CS, Brooks EG, Estes DM, Curran EM etal. Environmental
estrogens induce mast cell degranulation and enhance IgE-mediated release of allergic
mediators.Environ Health Perspect 2007;115:48–52.
Neumann E, Gutmann MJ, Blumenkranz N, Michaelson IC (1959): A review of four hundred
cases of vernal conjunctivitis. Am J Ophthalmol 47: 166–172.
Pitton C, Michel L, Salem P, Benhamou M, Mencia-Huerta JM, Maclouf J et al. Biochemical
and morphological modifications in dexamethasone-treated mouse bone marrow derived mast
cells. J Immunol1988;141:2437–2444.
Pucci N, Novembre E, Cianferoni A, Lombardi E, Bernardini R, Caputo R, Campa L , Vierucci
A (2002): Efficacy and safety of cyclosporine eyedrops in vernal keratoconjunctivitis. Ann
Allergy Asthma Immunol 89: 298–303.
Rocha EM, Wickham LA, da Silveira LA, Krenzer KL, Yu FS, Toda I, Sullivan BD, Sullivan
DA. Identification of androgen receptor protein and 5alpha-reductase mRNA in human ocular
tissues. Br J Ophthalmol. 2000 Jan;84(1):76-84.
Rouher N, Pilon F, Dalens H, Fauquert JL,Kemeny JL, Rigal D , Chiambaretta F(2004):
Implantation of preserved human amniotic membrane for the treatment of shield ulcers and
persistent corneal epithelial defects in chronic allergic keratoconjunctivitis. J Fr Ophtalmol 27:
1091–1097.
Sacchetti M, Baiardini I, Lambiase A, Aronni S, Fassio O, Gramiccioni C, Bonini S, Bonini
S.Development and testing of the quality of life in children with vernal keratoconjunctivitis
questionnaire.Am J Ophthalmol. 2007 Oct;144(4):557-63.
44
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Schirra F, Suzuki T, Dickinson DP, Townsend DJ, Gipson IK, Sullivan DA.Identification of
steroidogenic enzyme mRNAs in the human lacrimal gland, meibomian gland, cornea, and
conjunctiva.Cornea. 2006;25(4):438-42.
Secchi AG, Tognon MS , Leonardi A (1990): Topical use of cyclosporine in the treatment of
vernal keratoconjunctivitis. Am J Ophthalmol 110: 641–645.
Solomon A, Zamir E, Levartovsky S ,Frucht-Pery J (2004): Surgical managementof corneal
plaques in vernal keratoconjunctivitis:a clinicopathologic study. Cornea 23: 608–612.
Spadavecchia L, Fanelli P, Tesse R et al. (2006): Efficacy of 1.25% and 1% topical cyclosporine
in the treatment of severe vernal keratoconjunctivitis in childhood. Pediatr Allergy Immunol 17:
527–532.
Sudo N, Yu XN, Kubo C. Dehydroepiandrosterone attenuates the spontaneous elevation of
serum IgE level in NC/Nga mice. Immunol Lett 2001;79:177–179.
Sullivan DA.Tearful relationships? Sex, hormones, the lacrimal gland, and aqueous-deficient dry
eye.Ocul Surf. 2004 Apr;2(2):92-123.
Tabbara KF (1999): Ocular complications of vernal keratoconjunctivitis. Can J Ophthalmol34:
88–92.
Tabbara KF (2001): Tear tryptase in vernal keratoconjunctivitis. Arch Ophthalmol 119:338–342.
Tabbara KF , Arafat NT (1977):Cromolyn effects on vernal keratoconjuctivitis in children. Arch
Ophthalmol 95: 2184–2186.
Tabata N, Tagami H, Terui T.Dehydroepiandrosterone may be one of the regulators of cytokine
production in atopic dermatitis. Arch Dermatol Res 1997;289:410–414.
45
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Tanaka M, Takano Y, Dogru M, Fukagawa K, Asano-Kato N, Tsubota K , Fujishima H (2004):
A comparative evaluation of the efficacy of intraoperative mitomycin C use after the excision of
cobblestone- like papillae in severe atopic and vernal keratoconjunctivitis. Cornea 23: 326–329.
Tomassini M, Magrini L, Bonini S, Lambiase A , Bonini S (1994): Increase levels of eosinophil
cationic protein and eosinophil derived neurotoxin (protein X) in vernal keratoconjunctivitis.
Ophthalmology 101: 1808–1811.
Trocme SD, Kephart GM, Allansmith MR, Borne WM , Gleich GJ (1989): Conjunctival
deposition of eosinophil granule major basic protein in vernal keratoconjunctivitis and contact
lens-associated giant papillary conjunctivitis. Am J Ophthalmol 108: 57– 63.
Trocme SD, Kephart GM, Bourne WM, Buckley RJ , Gleich GJ (1993): Eosinophil granule
major basic protein deposition in corneal ulcers associated with vernal keratoconjunctivitis.
Am J Ophthalmol 115: 640–643.
Tuft SJ, Dart JK , Kemeny M (1989): Limbal vernal keratoconjunctivitis: clinical characteristics
and immunoglobulin E expression compared with palpebral vernal.Eye 3: 420–427.
Uchio E, Ono SY, Ikezawa Z , Ohno S (2000): Tear levels of interferon-g, interleukin (IL) -2,
IL-4 and IL-5 in patients with vernal keratoconjunctivitis, atopic keratoconjunctivitis and allergic
conjunctivitis. Clin Exp Allergy 30: 103–109.
Uekert SJ, Akan G, Evans MD, Li Z, Roberg K, Tisler C et al. Sex-related differences in
immune development and the expression of atopy in early childhood. J Allergy Clin Immunol
2006;118:1375–1381.
Vasiadi M, Kempuraj D, Boucher W, Kalogeromitros D, Theoharides TC. Progesterone inhibits
mast cell secretion.Int J Immunopathol Pharmacol 2006;19:787–794.
46
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Verin PH, Dicker ID , Mortemousque B (1999): Nedocromil sodium eye drops are more
effective than sodium cromoglycate eye drops for the long-term management of vernal
keratoconjunctivitis. Clin Exp Allergy 29: 529–536.
Yu CK, Liu YH, Chen CL. Dehydroepiandrosterone attenuates allergic airway inflammation in
Dermatophagoides farinae-sensitized mice. J Microbiol Immunol Infect 2002;35:199–202.
47
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Development and Testing of the Quality of Life in
Children with Vernal Keratoconjunctivitis Questionnaire
MARTA SACCHETTI, ILARIA BAIARDINI, ALESSANDRO LAMBIASE, SILVIA ARONNI, OMAR FASSIO,
CLAUDIA GRAMICCIONI, SERGIO BONINI, AND STEFANO BONINI
● PURPOSE:
To develop and validate a questionnaire that
measures health-related quality of life (HRQoL) in children with vernal keratoconjunctivitis (VKC).
● DESIGN: Prospective, observational case series.
● METHODS: An initial list of 42 items was developed
and administered to 30 children with active VKC (six
girls and 24 boys; mean age, nine ⴞ two years). The 30
most significant items were selected and converted into
questions on a three-step scale for validation in 41
children with active VKC (eight girls and 33 boys; mean
age, 9.5 ⴞ 2.1 years). Twenty-two children also completed the generic KINDL questionnaire. Clinical signs
were evaluated and scored and total sign scores (TSSs)
were calculated. Validation was performed by factorial
analysis and Pearson correlation. Internal consistency
was computed by the Chronbach ␣ on the extracted
factors.
● RESULTS: Factorial analysis extracted two factors with
good internal consistency: symptoms (12 items; ␣ ⴝ
0.89) and daily activities (four items; ␣ ⴝ 0.77). Correlations of Quality of Life in Children with Vernal
Keratoconjunctivitis (QUICK) scores to KINDL scores
were in the expected direction. Most patients reported
itching (93%), burning (90%), redness (90%), the need
to use eye drops (90%), tearing (83%), and photophobia
(80%). The children’s greatest concerns were limitations
on going to the pool (71%), playing sports (58%), and
meeting friends (58%). QUICK symptom scores were
correlated significantly to conjunctival hyperemia (P <
.001), secretion (P ⴝ .042), chemosis (P ⴝ .012),
superficial punctate keratopathy (P < .001), and TSS
(P ⴝ .010).
● CONCLUSIONS: The QUICK questionnaire is a new,
simple instrument to measure HRQoL in children with
severe allergic conjunctivitis. This test is effective for the
global evaluation of the impact of VKC on children’s
Accepted for publication Jun 19, 2007.
From the Department of Ophthalmology, University of Rome Campus
Bio-Medico, Rome, Italy (M.S., A.L., S.A., St.B.); the Section for
Allergy and Respiratory Diseases, Department of Internal Medicine,
University of Genoa, Genoa, Italy (I.B.); the Department of Psychology,
Turin University, Turin, Italy (O.F.); the Department of Internal Medicine, Second University of Naples, Naples, Italy (Se.B.); and the
Institute of Neurobiology and Molecular Medicine, Italian National
Research Council, Rome, Italy (C.G., Se.B.).
Inquiries to Stefano Bonini, Via E. Longoni, 83, 00155 Roma, Italy;
e-mail: [email protected]
0002-9394/07/$32.00
doi:10.1016/j.ajo.2007.06.028
©
2007 BY
daily lives. (Am J Ophthalmol 2007;144:557–563.
© 2007 by Elsevier Inc. All rights reserved.)
V
ERNAL KERATOCONJUNCTIVITIS (VKC) IS A SEVERE
allergic conjunctivitis mainly affecting preadolescent boys. It is characterized by recurrent inflammation of the conjunctiva and cornea causing intense
ocular symptoms such as redness, itching, photophobia,
and mucous discharge with corneal involvement and
potential impairment of visual function. These symptoms
may last all year with seasonal exacerbations and often
require long-term therapy.1,2 Clinical objective evaluation
of signs and symptoms commonly are used to evaluate
VKC severity. However, clinical evaluations may not
necessarily reflect the impact of the disease on the patients’
health-related quality of life (HRQoL). In fact, because the
presence of severe signs and symptoms of VKC may
significantly influence the well-being and daily functioning
of patients, often they or their parents refer problems with
daily activities, even in mild and moderate cases, to VKC.
The availability of an instrument to assess the impact of
symptoms of ocular surface inflammation on children’s
daily functioning would aid in the evaluation of VKC
severity and treatment outcomes.
HRQoL parameters have become important outcome measures in allergic diseases, and many questionnaires have been
developed to evaluate the impact of allergy on HRQoL.3–9 In
particular, rhinoconjunctivitis HRQoL questionnaires, addressed to adults, adolescents, and children, also include
the evaluation of eye symptoms. However, these questionnaires are not specific to ocular allergy, because symptoms
of both nasal and ocular allergy influence HRQoL
scores.10 –13 Moreover, allergic rhinoconjunctivitis only
accounts for a limited percentage of cases of allergic
conjunctivitis in children,14 usually the mildest forms
without corneal and visual involvement. In fact, studies of
quality of life in children with allergic rhinoconjunctivitis,
in contrast to studies in adults and adolescents, demonstrated minimal interference with their normal daily activities and emotions,6,13,15 whereas the severity of signs
and symptoms in VKC patients significantly influences
daily life and social interactions.1
This study describes the development and initial validation of a new instrument, the Quality of Life in Children
with Keratoconjunctivitis (QUICK) questionnaire, for the
measurement of HRQoL in children between five and 12
ELSEVIER INC. ALL
RIGHTS RESERVED.
557
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
years of age with allergic conjunctivitis, keratoconjunctivitis, or both. Our goal was to develop an instrument: 1)
able to capture physical, psychosocial, and practical aspects
of HRQoL of particular relevance in patients with VKC;
2) that is generated and tested according to well-established procedures applied to other, similar questionnaires;
and 3) designed to be used by children as a quick and
simple test.
METHODS
THIS STUDY WAS CARRIED OUT IN TWO SEPARATE PHASES:
the development and the validation processes, involving
two different groups of patients with VKC. The questionnaire was developed using a standard multistep method.
These phases are described in detail below.
● PATIENTS: Children (age, between four and 12 years)
with active VKC were recruited consecutively by the
Corneal and External Disease Center in Rome, Italy, from
March 20, 2003 through July 18, 2005 for the development
and validation phases of the new questionnaire. VKC
diagnosis was based on clinical history and objective
examination (presence of mild to severe cobblestone-like
appearance in the upper tarsal conjunctiva) and was
confirmed by the presence of eosinophils in a conjunctival
scraping. VKC was considered in the active phase when
patients reported symptoms of itching, photophobia, and
tearing associated with conjunctival hyperemia, mucous
discharge, epithelial keratopathy, or a combination thereof
at slit-lamp examination. Patients in treatment with topical steroid drugs were not included.
Clinical histories were collected and clinical signs (conjunctival tarsal or bulbar papillary reaction, secretion,
hyperemia and chemosis, corneal superficial keratopathy)
were evaluated and scored from 0 to 3 (0 ⫽ absent, 1 ⫽
mild, 2 ⫽ moderate, 3 ⫽ severe) to correlate questionnaire
scores to clinical findings. The total sign score was calculated as the sum of all the sign scores (range, zero to 18).
FIGURE 1. Diagram showing the procedure of query selection
during the development and validation phases of the Quality of
Life in Children with Vernal Keratoconjunctivitis (QUICK)
questionnaire in children with vernal keratoconjunctivitis
(VKC).
the field of ocular allergy was required to indicate
symptoms and problems troubling children with
VKC.1,2,14
3) Ten children with VKC in the active phase (seven
boys and three girls; mean age, 6.5 ⫾ three years)
and their parents (six men and four women; mean
age, 44 ⫾ six years) were interviewed by a clinician
and a psychologist to identify those areas of daily life
that were impaired by the presence of VKC.
4) Two psychologists (I.B. and O.F.) with experience in
the process of development and validation of qualityof-life questionnaires for allergic diseases were requested to adapt the items to a pediatric population.8
● DEVELOPMENT PROCESS:
Item Generation. The aim of
this phase was to identify symptoms and problems perceived as troublesome by patients with VKC. A preliminary list of items was developed on the basis of the
following sources:
Item Reduction. A qualitative selection was performed
from the preliminary list of items by eliminating those that
were redundant, ambiguous, difficult to understand, or
expressed in the negative form. The resulting list of items
was listed randomly and was administered to 30 children
with VKC in the active phase (24 boys and six girls; age
range, five to 12 years; mean age ⫾ standard deviation
[SD], nine ⫾ two years), who had to indicate which of the
selected items they had experienced directly in the preceding two weeks on a three-point scale: 1 ⫽ never, 2 ⫽
sometimes, and 3 ⫽ always. The highest scoring items then
were adopted to construct the new specific tool. The
1) An international literature review was performed to
identify existing questionnaires for HRQoL assessment in children with ocular surface symptoms,
allergy, or both by using the key words conjunctivitis,
rhinoconjunctivitis, keratoconjunctivitis, allergy, atopy,
children, quality of life, questionnaire.7,13,16,17
2) A panel of four ophthalmologists (M.S., A.L., S.A.,
and St.B.) and two immunologists (St.B. and C.G.)
who perform clinical and investigational research in
558
AMERICAN JOURNAL
OF
OPHTHALMOLOGY
OCTOBER 2007
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
TABLE 1. Characteristics of Patients with Vernal Keratoconjuctivitis Included in the
Development Phase (n ⫽ 30) and in the Validation Process (n ⫽ 41) of the QUICK Questionnaire
Characteristic of Patients
Item Reduction Phase
Validation Phase
No. of patients
Age (yrs)
Mean (range)
Gender (n)
Male
Female
Associated atopic conditions (n)
Asthma
Rhinitis
Atopic dermatitis
Urticaria
Vernal keratoconjunctivitis course (n)
Seasonal
Perennial
Duration of disease (yrs)
Range
Mean
Topical treatment (n)
Anti-allergic eye drop
Cyclosporine A eye drop
None
Vernal keratoconjunctivitis form (n)
Limbal
Tarsal
Mixed
Visual acuity (mean)
Total signs score (mean)
30
41
9 ⫾ 2 (5 to 12)
9.5 ⫾ 2.1 (5 to 12)
24
6
33
8
1
10
3
0
4
16
5
3
13
17
21
20
1 to 6
3.1 ⫾ 2
1 to 9
4.5 ⫾ 2.3
25
2
3
34
3
4
4
22
4
0.9/1 ⫾ 0.16/1
5 ⫾ 2.2
7
29
5
0.9/1 ⫾ 0.2/1
6.4 ⫾ 3
QUICK ⫽ Quality of Life in Children with Vernal Keratoconjunctivitis.
resulting questionnaire then was administered to a different patient population for validation (Figure 1).
● VALIDATION PROCESS:
Forty-one children with VKC
in the active phase (33 boys and eight girls; age range, five
to 12 years; mean age ⫾ SD, 9.5 ⫾ 2.1 years) completed
the preliminary QUICK questionnaire, converted into
questions on a Likert scale of three steps. Children were
asked to point out difficult questions or problems with any
item. Twenty-four of the 41 children also completed the
KINDL questionnaire, a generic tool designed to obtain an
assessment of HRQoL, independent of current health
status, in children of a wide age range.18 Nineteen children
were administrated the Kid-KINDL version (28 items for
children between eight and 12 years), and five children
were administered the Kiddy KINDL (12 items for children
between four and seven years). Both KINDL versions
include six domains (physical well-being, emotional wellbeing, self-esteem, family, friends, and school) and an
additional domain of six items for chronically ill children.
The subscales of KINDL are calculated such that a higher
score corresponds to a higher HRQoL.
VOL. 144, NO. 4
QUALITY
OF
LIFE
IN
The aim of the validation phase was to evaluate the
following psychometric properties of the new instrument:
1) Validity. This parameter assesses whether an instrument actually measures what it was designed to
measure. Factorial analysis was performed on the
preliminary QUICK questionnaire scores to identify
potential subscales according to our hypotheses; the
principal component method with Varimax rotation
was adopted. By means of Pearson correlation coefficients, we also evaluated the relationship between
the new questionnaire and the KINDL questionnaire
to evaluate the convergent validity.
2) Internal consistency. This parameter measures the
homogeneity of a scale. It was computed using the
Cronbach correlation coefficient on the extracted
factors. Measurements with reliability of 0.70 or
more have been recommended for the purpose of
comparing groups. The statistically significant cutoff
value was set at P ⬍ .05. The entire statistical
analysis was conducted by using SPSS software
version 10.0 (SPSS, Inc, Chicago, Illinois, USA).
CHILDREN
WITH
VKC
559
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
TABLE 2. Mean Response Scores (range, zero to three) to
the Preliminary List of 42 Questions Asked to 30 Children
with Vernal Keratoconjunctivitis in the Development Phase
of the QUICK Questionnaire
During the Last Two Weeks, Because of Conjunctivitis . . .
Score
1 . . . you had to use eye drops
2 . . . you had trouble going to the swimming
pool
3 . . . you rubbed your eyes
4 . . . you had red eyes
5 . . . you had tearing
6 . . . you had, in the morning, closed, and sticky
eyes
7 . . . you had itchy eyes
8 . . . you felt burning in your eyes
9 . . . you had problems playing with pets
10 . . . you had problems going to the cinema
11 . . . you had problems in the light
12 . . . you had to use tissues
13 . . . you had difficulties in reading
14 . . . you had eye secretion
15 . . . you were nervous and restless
16 . . . you had trouble meeting your friends
17 . . . you had problems playing video games or
computer
18 . . . you had trouble practicing sports (football,
gym, etc.)
19 . . . you felt embarrassed
20 . . . you had difficulties concentrating on
homework or other activities
21 . . . you had blurred vision
22 . . . you had problems at school
23 . . . you had trouble playing outdoors
24 . . . you had puffy eyes
25 . . . you have eaten little
26 . . . you had reduction in eyesight
27 . . . you had difficulties watching TV
28 . . . you had trouble staying in air-conditioned
rooms
29 . . . you cried easily
30 . . . you slept badly
31 . . . you had problems going to school
32 . . . you had problems riding your bicycle
33 . . . you were proud of yourself
34 . . . you had problems going to the country
35 . . . you had problems falling asleep
36 . . . you felt at ease with other people
37 . . . you attended school regularly
38 . . . you enjoyed playing with other children
39 . . . you had difficulty opening your eyes
completely
40 . . . you had problems participating in social
activities (boy scouts, football team, etc.)
41 . . . you were satisfied with yourself
42 . . . you searched for the company of your friends
2.46
TABLE 3. Factorial Analysis Allowed Selection of 16 Items
To Be Allocated into Two Domains (Symptoms and
Daily Activities) for the Final Version of the QUICK
Questionnaire to Assess Quality of Life in Children
with Vernal Keratoconjunctivitis
Factor II:
2.30
2.24
2.24
2.22
. . . you felt burning in your eyes
. . . you had trouble staying in
air-conditioned rooms
. . . you had to use tissues
. . . you had puffy eyes
. . . you had problems in the light
. . . you had tearing
. . . you had itchy eyes
. . . you had red eyes
. . . you had blurred vision
. . . you had eye secretion
. . . you had to use eye drops
. . . you had, in the morning, closed
and sticky eyes
. . . you had trouble playing outdoors
. . . you had trouble practicing sports
(football, gym)
. . . you had trouble meeting your
friends
. . . you had trouble going to the
swimming pool
% Variance
2.20
2.17
2.15
2.11
2.08
2.05
2.02
1.95
1.95
1.80
1.79
1.78
1.74
1.71
1.69
1.66
1.54
1.54
1.47
1.44
1.43
1.41
⫺0.143
0.719
0.717
0.715
0.694
0.689
0.689
0.664
0.635
0.596
0.565
0.042
0.070
⫺0.015
⫺0.123
⫺0.109
⫺0.343
⫺0.405
⫺0.105
⫺0.152
⫺0.091
0.536
0.217
⫺0.338
0.734
0.562
0.683
0.549
0.677
0.401
38.71
0.422
13.34
RESULTS
● SUBJECT
CHARACTERISTICS: Thirty children (24
boys and six girls) with VKC completed the initial list of
42 items for the development of the new questionnaire,
and 41 children with VKC (33 boys and eight girls)
completed the preliminary QUICK test of 30 items for
the validation phase. All patients were between five and
12 years of age. The characteristics of patients are listed
in Table 1. All patients showed signs and symptoms of
conjunctival inflammation with conjunctival hyperemia
(100%), mucus discharge (58%), and superficial punctuate keratitis (55%). At the time of inclusion in this
study, only seven patients (10%) were not receiving
treatment. The remaining patients were receiving treatment with antiallergic eye drops (83%), whereas a small
percentage (7%) also was treated with topical cyclosporine A.
1.41
1.37
1.35
1.35
1.34
1.34
1.21
1.20
1.10
1.07
1.06
1.04
0.99
0.98
0.78
AMERICAN JOURNAL
0.756
QUICK ⫽ Quality of Life in Children with Vernal Keratoconjunctivitis.
Total variance, 52.05%.
The 30 final items selected for the validation process are in
bold face.
560
Factor I: QUICK QUICK Daily
Symptoms
Activities
QUICK Items
● QUICK DEVELOPMENT PROCESS: Item Generation. The
initial list of expressions comprised 51 items. Whenever
OF
OPHTHALMOLOGY
OCTOBER 2007
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
TABLE 4. The QUICK Questionnaire Scores Showed
Significant Correlations to KINDL Scores in Children with
Vernal Keratoconjunctivitis
QUICK Symptoms
QUICK Daily
Activities
KINDL Domains
P Value
R
P Value
R
Physical well-being
Emotional well-being
Self-esteem
Family
Friends
School
Disease
Total score
.006
.335
.271
.824
.965
.605
.001
.101
⫺0.635
⫺0.239
0.283
0.824
⫺0.012
⫺0.135
⫺0.699
⫺0.359
.105
.584
.508
.947
.960
.862
.012
.281
⫺0.407
⫺0.143
0.172
⫺0.17
⫺0.13
⫺0.46
⫺0.526
⫺0.240
QUICK ⫽ Quality of Life in Children with Vernal Keratoconjunctivitis.
FIGURE 2. Bar graphs showing the percentage of children
referring the presence of (Top) vernal keratoconjunctivitis
(VKC)-related symptoms and (Bottom) daily life limitations in
the previous two weeks.
possible, children’s and parents’ language was maintained. The qualitative selection omitted nine items
that were considered redundant, ambiguous, difficult to
understand, expressed in negative form, or a combination thereof. The item generation phase resulted in a
pool of 42 items (Figure 1).
Item Reduction. Thirty patients with active VKC completed the preliminary questionnaire of 42 items (Table
1). Analysis of children’s answers allowed us to select 30
items with higher mean score for the validation process
(Table 2).
● QUICK VALIDATION PROCESS: Validation was undertaken in a group of 41 children with active VKC (Table 1).
Validity. Factor analysis revealed a bidimensional structure, which explained up to 52% of the total variance. This
solution was deemed appropriate on the basis of eigenvalues. Fourteen items were excluded because they were not
allocated to the extracted dimensions (Figure 1). The 16
items selected for the final version of the QUICK questionnaire were allocated into two domains: 1) symptoms
VOL. 144, NO. 4
QUALITY
OF
LIFE
IN
(12 items) and 2) daily activities (four items; Table 3). The
percentages of children with VKC referring symptoms and
problems in daily life are shown in Figure 2.
Item and scale scores were oriented so that higher scores
indicated worse HRQoL. To make scores more meaningful
and to permit comparisons among different populations of
patients, linear transformations were performed on raw
scores, indicating the percentage of maximum possible
scores. Thus, the minimum possible score is defined as zero
and the maximum possible score is defined as 100.
Twenty-four of 41 children (mean age, nine ⫾ two
years; 19 boys and five girls) also completed the KINDL
questionnaire. Correlations between QUICK and KINDL
scores were in the expected direction: as shown in Table 4,
conceptually similar domains had higher correlations than
conceptually unrelated domains.
Internal Consistency. The dimensions of QUICK
showed satisfactory Cronbach ␣ values: symptoms, ␣ ⫽
0.889; and daily activities, ␣ ⫽ 0.772. The QUICK
symptom factor showed a significant correlation to objective clinical sign scores: conjunctival hyperemia (P ⬍ .001;
⫽ 0.656), secretion (P ⫽ .042; ⫽ 0.409), chemosis
(P ⫽ .012; ⫽ 0.469), superficial punctuate keratopathy
(P ⬍ .001; ⫽ 0.657), and limbal papillary reaction (P ⫽
.042; ⫽ 0.387), but not with tarsal papillary reaction and
duration of disease. The total signs score also was significantly related to the QUICK symptoms score
(P ⫽ .010; ⫽ 0.442). The QUICK daily activity factor
showed no significant correlation to clinical sign scores.
DISCUSSION
THIS STUDY DESCRIBES THE DEVELOPMENT AND INITIAL
validation of an age- and disease-specific quality-of-life
questionnaire for allergic keratoconjunctivitis in a group of
children with VKC. VKC is, together with atopic keratoCHILDREN
WITH
VKC
561
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
conjunctivitis, the most severe form among ocular allergies.1,2,14,19 VKC is a rare disease affecting young patients
with severe ocular symptoms that undoubtedly interferes
with their quality of life. In addition to their intense ocular
discomfort, children with VKC often experience negative
consequences because of the limiting of many of their
preferred activities in the attempt to avoid worsening of
their disease. What children really experience in daily life,
and their subjective viewpoint about symptoms and problems resulting from VKC, should not be neglected in the
planning of patient management. In contrast to existing
quality of life tests that include items for allergic conjunctivitis, the QUICK questionnaire was developed to be used
specifically in children with severe forms of ocular allergy
with or without corneal involvement.
The final version of the QUICK questionnaire contains
16 items. It was designed specifically to be administered
easily and quickly to five- to 12-year-old children with
chronic keratoconjunctivitis. The validation process
showed that the new questionnaire met the standards for
internal consistency and validity. Psychometric characteristics make QUICK useful to evaluate the specific burden
of VKC on HRQoL. At present, it also seems to be the first
validated questionnaire specific for the assessment of
HRQoL in VKC.
Conceptually similar domains of QUICK showed significant correlations to KINDL, providing good evidence for
QUICK validity. In particular, the QUICK symptoms
domain was significantly related to the physical well-being
and disease domains of KINDL, suggesting that VKCrelated symptoms are associated with a reduction of health
status and to a subjective perception of illness. The disease
domain of KINDL also was related significantly to the daily
activity domain of QUICK, indicating that the children’s
functioning in everyday life is influenced negatively by the
presence of VKC.
The QUICK questionnaire was validated in a population of children with VKC aged between five and 12 years.
The item generation phase of the questionnaire included
children younger than five years who initially were interviewed with their parents to collect information regarding
VKC-related problems. However, because of the lack of
collaboration of younger children, only children aged more
than five years were included in the subsequent phases of
administration of the questionnaire. The differences in age
between the groups of patients should not affect the
validity of the QUICK questionnaire, because children
included in all subsequent phases of development and
validation were aged between five and 12 years. In addition, because topical steroids exert a prompt and intense
effect by reducing signs and symptoms of VKC, patients in
treatment with topical steroids were not included in the
study to avoid interferences of such treatments on the
children’s perception of the disease.
562
AMERICAN JOURNAL
The QUICK questionnaire was developed for its initial
validation in the Italian language because the prevalence
of VKC is higher in Mediterranean countries than in other
regions.1,2,19 An English version of the questionnaire also
was produced (© 2007 Barzanò & Zanardo) for which the
Italian version was translated into English and back by two
independent bilingual translators. The administration of
the QUICK questionnaire in other languages and in
different geographic and cultural regions may contribute to
its further validation.
The QUICK symptoms domain showed significant correlation to the clinical, objective parameters of VKC
severity, indicating that the QUICK symptom score is
related to the disease process. The lack of significant
correlation between the QUICK daily activities domain
and clinical sign scores may be explained by daily life
adjustments related to the perception of the disease by the
children, their parents, or both, rather than the severity of
the disease at the time of the visit. In addition, the parents’
perception of the disease may have a profound impact on
the child’s own perception, influencing the child’s diseaserelated quality of life and capacity for adjustment. Because
the aim of the study was to provide a tool capable of
assessing VKC-related quality of life, its relationship to the
child’s psychological state or to a combination of the
child’s and parents’ psychological condition has not been
investigated. Further studies should be performed to clarify
such an association. In our opinion, the lack of correlation
between the QUICK daily activities domain and clinical
sign scores should not be interpreted as a sign of reduced
validity, but rather suggests the importance of combining
clinical, objective evaluations to HRQoL instruments to
balance all kinds of health outcome measures.
Itching, burning, redness, photophobia, and the need to
use eye drops were the most frequent symptoms reported,
because these are the expression of the severity of the
allergic inflammation.1,14 However, children with VKC
also experienced disease-related limitations in their daily
life and social interactions such as playing sports and
meeting friends. Patients reported limitations in activities
that cause exposure to allergens such as playing outdoors20
and to irritant stimuli, such as going to the pool because of
the notoriously powerful irritating effects of chlorinated air
and water.21,22 These findings suggest that treatment of
VKC should improve not only the children’s signs and
symptoms, but also their daily life and functioning.
In conclusion, the QUICK questionnaire is a new tool
for the measurement of HRQOL in children with allergic
conjunctivitis, including those with severe symptoms,
corneal involvement, or both. This new instrument may
allow collection of information on relevant additional
clinical variables in subjects with severe ocular allergy,
both in clinical practice and in drug trials.
OF
OPHTHALMOLOGY
OCTOBER 2007
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
THIS STUDY WAS SUPPORTED BY AN EU-FRAMEWORK PROGRAMME FOR RESEARCH, CONTRACT NO. FOOD-CT-2004-506378,
the GA2LEN project (Global Allergy and Asthma European Network). The authors indicate no financial conflict of interest. Involved in design and
conduct of study (M.S., I.B., A.L., S.A., C.G., Se.B., St.B.); collection (M.S., S.A., St.B.), analysis (O.F.), and interpretation of the data (M.S., I.B.,
A.L., O.F., Se.B., St.B.); and preparation (M.S., I.B., A.L., S.A., O.F., C.G., Se.B., St.B.), review (A.L., S.A., Se.B., C.G., St.B.), and approval of the
manuscript (M.S., I.B., A.L., S.A., O.F., C.G., Se.B., St.B.). The study was conducted following the tenets of the Declaration of Helsinki; the use of
the QUICK questionnaire was approved by the Institutional Review Board of the University of Rome Campus Bio-Medico, and informed consent was
obtained from the participating children’s parents.
We would like to thank Annalisa Alesii, San Raffaele La Pisana, Rome, Italy, and Cristina Artesani, Allergy Unit C.I. Columbus, Rome, Italy, for
their contribution in the first phase of the development of the questionnaire. The copyright for the Italian and English versions of the QUICK
questionnaires has been provided by Barzanò & Zanardo, 2007.
REFERENCES
1. Bonini S, Bonini S, Lambiase A, et al. Vernal keratoconjunctivitis revisited: a case series of 195 patients with
long-term follow-up. Ophthalmology 2000;107:1157–1163.
2. Bonini S, Coassin M, Aronni S, Lambiase A. Vernal keratoconjunctivitis. Eye 2004;18:345–351.
3. Guyatt GH, Feeny DH, Patrick DL. Measuring healthrelated quality of life. Ann Intern Med 1993;118:622– 629.
4. Felce D, Perry J. Quality of life: its definition and measurement. Res Dev Disabil 1995;16:51–74.
5. Leynaert B, Soussan D. Monitoring the quality-of-life in
allergic disorders. Curr Opin Allergy Clin Immunol 2003;3:
177–183.
6. Juniper EF. Measuring health-related quality of life in rhinitis. J Allergy Clin Immunol 1997;99:S742–S749.
7. Rutishauser C, Sawyer SM, Bowes G. Quality-of-life assessment in children and adolescents with asthma. Eur Respir J
1998;12:486 – 494.
8. Baiardini I, Pasquali M, Giardini A, et al. Rhinasthma: a new
specific questionnaire for patients with rhinitis and asthma.
Allergy 2003;58:289 –294.
9. Cohen BL, Noone S, Munoz-Furlong A, Sicherer SH.
Development of a questionnaire to measure quality of life in
families with a child with food allergy. J Allergy Clin
Immunol 2004;114:1159 –1163.
10. Juniper EF, Guyatt GH. Development and testing of a new
measure of health status for clinical trials in rhinoconjunctivitis. Clin Exp Allergy 1991;21:77– 83.
11. Bunnag C, Leurmarnkul W, Jareoncharsri P, et al. Development of a health-related quality of life questionnaire for Thai
patients with rhinoconjunctivitis. Asian Pac J Allergy Immunol 2004;22:69 –79.
12. Juniper EF, Guyatt GH, Dolovich J. Assessment of quality of
life in adolescents with allergic rhinoconjunctivitis: development and testing of a questionnaire for clinical trials. J
Allergy Clin Immunol 1994;93:413– 423.
VOL. 144, NO. 4
QUALITY
OF
LIFE
IN
13. Juniper EF, Howland WC, Roberts NB, Thompson AK, King
DR. Measuring quality of life in children with rhinoconjunctivitis. J Allergy Clin Immunol 1998;101:163–170.
14. Bielory L, Bonini S, Bonini S. Allergic eye disorders. In:
Zweiman B, Schwartz LB, eds. Inflammatory mechanisms in
allergic diseases. New York, New York: Marcel Dekker,
2002:311–323.
15. Meltzer EO. Quality of life in adults and children with
allergic rhinitis. J Allergy Clin Immunol 2001;108:S45–S53.
16. Juniper EF, Thompson AK, Ferrie PJ, Roberts JN. Development and validation of the mini rhinoconjunctivitis quality
of life questionnaire. Clin Exp Allergy 2000;30:132–140.
17. French DJ, Carroll A, Christie MJ. Health-related quality of
life in Australian children with asthma: lessons for the
cross-cultural use of quality of life instruments. Qual Life Res
1998;7:409 – 419.
18. Ravens-Sieberer U, Bullinger M. Assessing health-related
quality of life in chronically ill children with the German
KINDL®: first psychometric and content analytical results.
Qual Life Res 1998;7:399 – 407.
19. Leonardi A. Vernal keratoconjunctivitis: pathogenesis and
treatment. Prog Retin Eye Res 2002;21:319 –339.
20. Halken S. Prevention of allergic disease in childhood:
clinical and epidemiological aspects of primary and secondary allergy prevention. Pediatr Allergy Immunol 2004;15:
S9 –S32.
21. Bernard A, Carbonelle S, Michel O, et al. Lung hyperpermeability and asthma prevalence in schoolchildren:
unexpected associations with the attendance at indoor
chlorinated swimming pools. Occup Environ Med 2003;
60:385–394.
22. Massin N, Bohadana AB, Wild P, Hery M, Toamain JP,
Hubert G. Respiratory symptoms and bronchial responsiveness in lifeguards exposed to nitrogen trichloride in
indoor swimming pools. Occup Environ Med 1998;55:
258 –263.
CHILDREN
WITH
VKC
563
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Clinical grading of vernal keratoconjunctivitis
Stefano Bonini, Marta Sacchetti, Flavio Mantelli and Alessandro Lambiase
Purpose of review
The purpose of the present review is to provide an overview
on the clinical features of vernal keratoconjunctivitis on the
basis of cases series presented in the literature.
Furthermore, a new grading system of vernal
keratoconjunctivitis based on the severity of the disease is
proposed. Different treatment options are discussed based
on the clinical grade of vernal keratoconjunctivitis.
Recent findings
Recent epidemiological studies on the demographic,
clinical and immunologic features of vernal
keratoconjunctivitis are presented. The efficacy and
complications of treatments are described.
Summary
Diagnosis and treatment of patients is a challenge for
ophthalmologists as no precise diagnostic criteria have
been established, the pathogenesis is unclear, and
antiallergic treatments are often unsuccessful. This review
describes old and new concepts of vernal
keratoconjunctivitis diagnosis and treatment: the clinical
features, the diagnostic criteria, the common features
between this and other ocular allergies and the therapeutic
strategies. On the basis of this knowledge, a new grading
system is introduced based on clinical signs and symptoms
of ocular surface inflammation. This new grading of vernal
keratoconjunctivitis may help clinicians and researchers to
classify disease activity and to establish a common
agreement for treatments.
Keywords
allergy, antiallergic treatments, cyclosporine A, steroids,
vernal keratoconjunctivitis
Curr Opin Allergy Clin Immunol 7:436–441. ß 2007 Lippincott Williams & Wilkins.
Department of Ophthalmology, University of Rome Campus Bio-Medico,
Rome, Italy
Correspondence to Stefano Bonini, MD, University of Rome Campus Bio-Medico,
Department of Ophthalmology, Via E. Longoni, 83, 00155 Rome, Italy
Tel: +39 0622541342; fax: +39 0622541456; e-mail: [email protected]
Current Opinion in Allergy and Clinical Immunology 2007, 7:436–441
Abbreviations
PAC
SAC
VKC
perennial allergic conjunctivitis
seasonal allergic conjunctivitis
vernal keratoconjunctivitis
ß 2007 Lippincott Williams & Wilkins
1528-4050
Introduction
Vernal keratoconjunctivitis (VKC) is a disease usually
contained under the classification of allergic conjunctivitis,
together with seasonal allergic conjunctivitis (SAC),
perennial allergic conjunctivitis (PAC) and atopic keratoconjunctivitis (AKC) [1]. In spite of common clinical and
immunological features, however, VKC differs from other
ocular allergic diseases for age of onset, clinical findings,
low percentage of patients with positive response to
standard allergic diagnostic tests and scarce response to
antiallergic treatments [2]. The lack of standardized
diagnostic criteria and the lack of a common language
between physicians regarding the definition and the
severity of VKC renders this disease more difficult to
diagnose and treat. This article summarizes the authors’
longstanding clinical and research experience in order to
propose a new clinical grading according to the clinical
phases of VKC. This proposal may help physicians use a
common language in the diagnosis and management of
patients. Furthermore, this grading may be used to allow a
more homogenous selection of patients for clinical trials.
Definition and features of vernal
keratoconjunctivitis
VKC, an orphan disease characterized by severe chronic
inflammation of the ocular surface, mainly affects boys in
the first decade of life [2,3]. The disease is generally
bilateral and is characterized by seasonal or perennial
symptoms that exacerbate in spring or early autumn.
During exacerbations, patients complain of symptoms of
intense itching and photophobia associated with tearing
and sticky mucus discharge. The disease may primarily
involve the tarsal or limbal conjunctiva leading to different
forms of VKC: limbal, tarsal or mixed (both limbal
and tarsal) forms. The presence of giant papillae with a
cobblestone-like appearance in the upper tarsal conjunctiva or at the limbus is considered the hallmark of the
disease. These signs are associated with the presence of
Horner–Trantas dots and corneal involvement, ranging
from superficial punctuate keratopathy to corneal erosions
and shield ulcers [2,3,4–6].
VKC generally has a good prognosis; however, in our case
series of 195 patients with VKC, 6% of patients showed a
permanent reduction in visual acuity as a result of corneal
damage [2,7–9].
Treatments
Topical steroids have been shown to be effective in
controlling ocular surface inflammation in VKC, but they
436
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Vernal keratoconjunctivitis Bonini et al. 437
should be used with particular caution due to their ocular
side effects including glaucoma and cataract formation
[2,4,9–13]. As alternative, new topical agents with dual
antiallergic activity (mast cell stabilizers and antihistamine) may be used for long-term treatment of allergic
inflammation, to alleviate signs and symptoms of the
disease [4,12,14–20]. In spite of treatments, symptoms
and signs of severe forms are not adequately controlled
unless prolonged steroid-based therapies are used
[2,3,4]. Recently, topical treatment with cyclosporine
A 1% and 2% eye-drops has been proposed for patients
with VKC. The efficacy of topical cyclosporine A in
VKC has been already reported, but it requires further
investigations with long-term randomized clinical studies
[21–28].
Common features of vernal
keratoconjunctivitis and other ocular allergies
Patients with VKC may share several anamnestic,
diagnostic and clinical features with other ocular allergic
diseases. For instance, a personal or family history of
allergy is detectable in approximately 50% of patients with
VKC and is a common finding in patients with seasonal or
perennial allergic conjunctivitis [1,2,3,29]. In addition,
atopic dermatitis is present in 10% of VKC patients and
is constantly present in patients with atopic keratoconjunctivitis [1,30].
High levels of specific serum IgEs as well as a positive
skin test to common allergens are constant features of
almost all ocular allergies. The presence of specific IgEs
to seasonal or perennial allergens can be documented in
approximately all cases of SAC and PAC, but many
patients with VKC show a negative response to skin test
or radioallergosorbent test (RAST) for common allergens.
In agreement with other studies, our case series of VKC
reported positive skin tests in 58% of patients with VKC,
and positive RAST tests in 52% of patients [2,3,31].
Signs and symptoms of VKC may not always allow a
differential diagnosis with respect to other ocular allergic
diseases. Severe forms of VKC typically present with a
cobblestone-like appearance of the upper tarsal or limbal
conjunctiva, associated with mucus discharge, corneal
damage and intense itching. These severe forms are
easily distinguishable from other allergic conjunctivitis,
while the mildest forms do not always show these typical
manifestations. Indeed, the presence of giant papillae
may certainly orient towards a diagnosis of VKC. Corneal
involvement is present in the clinical picture of AKC and
VKC, but not in SAC and PAC. The presence of severe
itching is a constant feature of VKC that is detectable in
more than 96% of patients. Moderate to intense itching,
however, is a common feature of all ocular allergic diseases representing a diagnostic criterion to distinguish
allergic conjunctivitis from other diseases of the ocular
surface [1,2,3,4,31].
The presence of eosinophils in the conjunctival
epithelium may be an additional tool to distinguish
VKC from other diseases of the ocular surface. This
feature is present in 85% of conjunctival scrapings of
VKC patients, but may also be present in patients with
other allergic conjunctivitis [1,2,31].
Variability of clinical features of vernal
keratoconjunctivitis
The term ‘vernal’ does not appropriately describe the
course of the disease in a significant percentage of patients.
In fact, most patients in our series of 195 patients showed a
seasonal presentation of the disease, but 23% of patients
showed a perennial form and 60% of patients also had
recurrences during winter [2].
In addition, prolonged inflammation (presence of the
disease for more than 3 years) leads to a greater chance
of developing perennial symptoms all year round [2,7].
Moreover, intermittent daily worsening of symptoms
(during seasonal recurrences) is a common finding in
most of our patients. These daily changes have not been
adequately studied but they seem to be related to
unknown environmental factors and are scarcely influenced by antiallergic treatments. Symptom variability
could influence the outcome of clinical trials especially
if patient enrolment occurs during a prolonged period of
time [2,32,33].
Signs of the disease are also extremely variable in severity
and presentation: cobblestone-like appearance or mild
papillary reaction, corneal keratopathy or absence of
corneal involvement, signs of conjunctival fibrosis or
conjunctival oedema. These findings are not necessarily
all simultaneously present in VKC patients, but may
represent different evolutions of the disease.
Clinical grading of vernal keratoconjunctivitis
Based on the clinical characteristics of VKC, we suggest
the following grading system to be adopted to grade the
severity of the disease at the moment of the clinical
examination (Table 1):
(1) Grade 0, quiescent: the disease was present in the past
(i.e. 1 year ago during spring season) or in the recent
present, but at the time of visit the patient is free of
symptoms, the conjunctiva shows no (or mild) hyperemia
and the cornea is not involved in the allergic reaction. In
contrast to the lack of symptoms and ocular involvement,
papillae may be present (þ1 up to þ3 papillary reaction),
although they are not inflamed.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Absent
Absent/mild
(2) Grade 1, mild intermittent: the patient refers to onset of
symptoms, such as itching and mild photophobia, during
spring season. Occasional symptoms may be present
during the day but their occurrence is short and well
tolerated. Slight ocular inflammation leads to mild
hyperemia (Fig. 1a) but no corneal involvement. Once
again, papillary reaction ranges from þ1 to þ3, and giant
papillae may be present notwithstanding the mild form of
the disease (Fig. 1b).
(3)Grade2,moderate,isdividedintotwomoregradesbased
on the severity of symptoms and corneal involvement:
(a) 2A Moderate intermittent: symptoms occur as in
grade 1 but they are more frequent and disturbing during
the day. Mild conjunctival secretion and tearing may
interfere with daily activity. Mild to severe papillary
reaction may be observed as well as conjunctival hyperemia (Fig. 1c), without corneal involvement.
(b) 2B Moderate persistent the patient is symptomatic
every day during season. Conjunctival hyperemia,
secretion and itching occur everyday. The cornea
may be occasionally involved with superficial punctuate
keratitis. Mild to severe papillary reaction may be
observed (Fig. 1d).
(4) Grade 3, severe: symptoms are present everyday and
the patient’s daily activities are influenced by the intense
itching and photophobia. Moderate to severe conjunctival
hyperemia (Fig. 1e) and secretion may be associated to the
presence of Horner-Trantas dot. The cornea is involved
with superficial punctuate keratitis. Mild to severe
conjunctival papillae (þ3 to þ4 papillary reaction) are
common, and present injection and swelling (Fig. 1f).
(5) Grade 4, very severe: severe itching and photophobia
are present everyday with mucus discharge on the ocular
surface and between papillae. Presence of superficial
keratopathy or corneal erosions and ulcerations are
common features. Horner-Trantas dots are present (more
than 3), and mild to severe papillary reaction (þ3 to þ4),
with injection and swelling, is usual (Fig. 1g,h).
VKC, vernal keratoconjunctivitis.
Severe
Moderate to severe
Absent or mild and occasional
symptoms
Grade 5, evolution
Grade 4, very severe
Few Trantas dots may
be present
Numerous Trantas dots
may be present
Absent
Moderate to severe
Superficial punctuate
keratitis may be present
Superficial punctuate
keratitis
Corneal erosion or
ulceration.
Absent
Absent
Mild to severe
Moderate to severe with
injection and swelling
Moderate to severe with
injection and swelling
Mild to severe fibrosis
Mild to moderate
Moderate to severe
Mild to moderate
Grade 0, quiescent
Grade 1, mild intermittent
Grade 2A, moderate
intermittent
Grade 2B, moderate
persistent
Grade 3, severe
Table 1 Clinical grading (from 0 to 5) of vernal keratoconjunctivitis
Corneal involvement
Absent
Absent
Absent
Trantas dot
Absent
Absent
Absent
Papillary reaction
Mild to moderate
Mild to moderate
Mild to severe
Conjunctival secretion
Absent
Absent/mild
Mild
Conjunctival hyperemia
Absent/mild
Mild
Mild
Symptoms
Absent
Mild and occasional symptoms
Mild to moderate intermittent
symptoms
Mild to moderate persistent
symptoms
Moderate to severe persistent
symptoms
Severe and persistent symptoms
VKC grading
438 Eye allergy
(6) Grade 5, evolution: the patient has occasional
symptoms during seasonal periods. Conjunctival papillary reaction may be present but the cornea is spared.
Evidence of conjunctival fibrosis may be seen on the
upper tarsal conjunctiva or at the fornix (Fig. 1i,j).
Treatment options
Although clinicians in the field of ocular allergies agree that
there are several features to aid in their differential diagnosis, once they describe therapeutic options, they generally refer to the wide range of topical treatments rather than
considering different treatments for the different clinical
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Vernal keratoconjunctivitis Bonini et al. 439
Figure 1 Clinical grading of vernal keratoconjunctivitis
The patient with vernal keratoconjunctivitis (VKC) at grade 1 shows mild conjunctival hyperemia (a) and papillary reaction (b). The grade 2 of the disease is
characterized by moderate conjunctival hyperemia (c) and papillary reaction (d). More severe ocular surface inflammation (e) with severe papillary reaction
(f) are present in grade 3. Severe corneal involvement and ocular surface inflammation with limbal reaction (g) or papillary injection with mucous discharge
(h) are considered as grade 4. Conjunctival fibrosis at upper tarsal (i) or fornix (j) are associated with VKC evolution phase (grade 5).
presentations. At present, there is a wide range of antiallergic drugs in the market, but it must be highlighted that
all these drugs are exclusively symptomatic, and have no
effect on disease activity or progression.
Although with peculiar features, the mildest grades of VKC
may show many similarities to the other forms of allergic
conjunctivitis, and thus they may all share a common
therapeutic approach. On the other hand, the more severe
grades (3 and 4) of the VKC require more effective and
prompt therapeutic approaches. Indeed, therapeutic
options must be considered on the basis of disease severity
and personalized according to the single patient.
In line with the proposed grading, we indicate possible
therapeutic options as follows (Fig. 2):
(1) Grade 0, quiescent: no treatment is needed in this
phase of the disease; the usual approach is to wait for
symptoms to occur.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
440 Eye allergy
Figure 2 Different therapeutic approach proposed for the different vernal keratoconjunctivitis grades
Grade 4
Very severe
Grade 2
Moderate: A
intermittent,
B persisent
Grade 3
Severe
Topical
pulsed steroid
(high dose)
Topical pulsed
steroid
Cyclosporine A eye drops
Grade 1
Mild
intermittent
Grade 0
Quiescent
No
treatments
Occasional
Antiallergic
eye drops
Daily administration
Antiallergic eye drops
(Mast cell stabilizers/
anti-histamine/
Dual action)
Grade 5
Evolution
Occasional
Antiallergic
eye drops
Lubricant eye drops/Vasoconstrictors eye drops when necessary
(2) Grade 1, mild intermittent: topical vasoconstrictors or
antihistamines may be used in this phase to control the
mild symptoms of the disease.
(3) Grade 2, moderate, in grades 2A and 2B the therapeutic approach is based on the use of topical antiallergic
eye drops such as antihistamines or mast cell stabilizers,
as well as dual action antiallergic drugs:
(a) 2A Moderate intermittent: brief courses of antiallergic
eye drops may be used to control symptoms of the
disease. Topical steroid are not required in this grade
of the disease.
(b) 2B Moderate persistent: daily administration of
topical antiallergic drugs are generally required to maintain low levels of ocular inflammation and to control daily
manifestations of the disease.
(4) Grade 3, severe: daily administration of topical
antihistamines or mast cell stabilizers, as well as dual action
antiallergic drugs, is recommended. As a possible alternative, topical cyclosporine A from 1% to 2%, has been
proposed [21–28]. In addition, a brief pulse of high dose
topical steroids may be considered in the recurrences of
ocular inflammation. Moreover, to avoid possible abuses,
steroids should be prescribed in a controlled regimen, in
order to reach a maximum of 10 drops per month,
during season.
(5) Grade 4, very severe: in general, treatment recommendations are the same as for grade 3, although topical
steroids are more frequently required. Clinicians should
strongly suggest patients to record the use of steroid
eye drops in order to limit possible abuses. The use of
topical cyclosporine should be considered on a daily basis.
When present, corneal shield ulcers should be surgically
removed. No treatment is necessary for the presence of
giant papillae, including cryotherapy.
(6) Grade 5, evolution: brief courses of topical antihistamines or mast cell stabilizers, as well as multiple active
antiallergic drugs, may be used to control symptoms of
the disease during recurrences. No further therapies are
required during periods of disease quiescence.
Conclusion
In conclusion, we have proposed a new grading for
clinical signs and symptoms of VKC patients. We believe
that grading of the disease may allow a clearer evaluation
of disease severity and progression, and may aid in the
choice of therapeutic options and analysis of treatment
efficacy. Grading of the disease may also help create a
common language among researchers and clinicians,
allowing a more careful and homogenous selection of
patients for enrolment in clinical trials.
Further clinical trials are necessary to validate the
proposed grading system.
References and recommended reading
Papers of particular interest, published within the annual period of review, have
been highlighted as:
of special interest
of outstanding interest
Additional references related to this topic can also be found in the Current
World Literature section in this issue (p. 456).
1
Bielory L. Allergic and immunologic disorders of the eye. Part II: Ocular allergy.
J Allergy Clin Immunol 2000; 106:1019–1032.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Vernal keratoconjunctivitis Bonini et al. 441
2
Bonini S, Bonini S, Lambiase A, et al. Vernal keratoconjunctivitis revisited: a
case series of 195 patients with long-term follow-up. Ophthalmology 2000;
107:1157–1163.
Leonardi A, Busca F, Motterle L, et al. Case series of 406 vernal
keratoconjunctivitis patients: a demographic and epidemiological study. Acta
Ophthalmol Scand 2006; 84:406–410.
This study evaluated the specific allergic sensitization and epidemiological characteristics based on data collected in 406 cases of vernal keratoconjunctivitis
(VKC).
3
17 Lee S, Allard TR. Lodoxamide in vernal keratoconjunctivitis. Ann Pharmacother
1996; 30:535–537.
18 Foster CS. Evaluation of topical cromolyn sodium in the treatment of vernal
keratoconjunctivitis. Ophthalmology 1988; 95:194–201.
19 Avunduk AM, Tekelioglu Y, Turk A, Akyol N. Comparison of the effects of
ketotifen fumarate 0.025% and olopatadine HCl 0.1% ophthalmic
solutions in seasonal allergic conjunctivities: a 30-day, randomized,
double-masked, artificial tear substitute-controlled trial. Clin Ther 2005;
27:1392– 1402.
4
Leonardi A. Vernal keratoconjunctivitis: pathogenesis and treatment. Prog
Retin Eye Res 2002; 21:319–339.
5
Pucci N, Novembre E, Lombardi E, et al. Atopy and serum eosinophil cationic
protein in 110 white children with vernal keratoconjunctivitis: differences
between tarsal and limbal forms. Clin Exp Allergy 2003; 33:325–330.
6
Tuft SJ, Dart JK, Kemeny M. Limbal vernal keratoconjunctivitis: clinical
characteristics and immunoglobulin E expression compared with palpebral
vernal. Eye 1989; 3 (Pt 4):420–427.
22 Mendicute J, Aranzasti C, Eder F, et al. Topical cyclosporin A 2% in the
treatment of vernal keratoconjunctivitis. Eye 1997; 11:75–78.
7
Bonini S, Coassin M, Aronni S, Lambiase A. Vernal keratoconjunctivitis.
Eye 2004; 18:345–351.
23 Secchi AG, Tognon MS, Leonardi A. Topical use of cyclosporine in the
treatment of vernal keratoconjunctivitis. Am J Ophthalmol 1990; 110:641–
645.
8
Iqbal A, Jan S, Babar TF, Khan MD. Corneal complications of vernal catarrh.
J Coll Physicians Surg Pak 2003; 13:394–397.
9
Tabbara KF. Ocular complications of vernal keratoconjunctivitis. Can J
Ophthalmol 1999; 34:88–92.
10 Tabbara KF, al-Kharashi SA. Efficacy of nedocromil 2% versus fluorometholone
0.1%: a randomised, double masked trial comparing the effects on severe vernal
keratoconjunctivitis. Br J Ophthalmol 1999; 83:180–184.
11 Akman A, Irkec M, Orhan M. Effects of lodoxamide, disodium cromoglycate
and fluorometholone on tear leukotriene levels in vernal keratoconjunctivitis.
Eye 1998; 12 (Pt 2):291–295.
12 Coutu RB. Treatment of vernal keratoconjunctivitis: a retrospective clinical
case study. Wallace F. Molinari Ocular Pharmacology Award. Optom Vis Sci
1991; 68:561–564.
13 Dada T, Konkal V, Tandon R, et al. Corneal topographic response to
intraocular pressure reduction in patients with vernal keratoconjunctivitis
and steroid-induced glaucoma. Eye 2007; 21:158–163.
14 Kosrirukvongs P, Vichyanond P, Wongsawad W. Vernal keratoconjunctivitis
in Thailand. Asian Pac J Allergy Immunol 2003; 21:25–30.
15 Verin P, Allewaert R, Joyaux JC, et al., Lodoxamide Study Group. Comparison of
lodoxamide 0.1% ophthalmic solution and levocabastine 0.05% ophthalmic
suspension in vernal keratoconjunctivitis. Eur J Ophthalmol 2001; 11:120–
125.
16 Verin PH, Dicker ID, Mortemousque B. Nedocromil sodium eye drops are more
effective than sodium cromoglycate eye drops for the long-term management of
vernal keratoconjunctivitis. Clin Exp Allergy 1999; 29:529–536.
20 Abelson MB. A review of olopatadine for the treatment of ocular allergy. Expert
Opin Pharmacother 2004; 5:1979–1994.
21 BenEzra D, Matamoros N, Cohen E. Treatment of severe vernal keratoconjunctivitis with cyclosporine A eyedrops. Transplant Proc 1988; 20 (Suppl 2):
644–649.
24 Gupta V, Sahu PK. Topical cyclosporin A in the management of vernal
keratoconjunctivitis. Eye 2001; 15:39–41.
25 Bleik JH, Tabbara KF. Topical cyclosporine in vernal keratoconjunctivitis.
Ophthalmology 1991; 98:1679–1684.
26 Spadavecchia L, Fanelli P, Tesse R, et al. Efficacy of 1.25% and 1% topical
cyclosporine in the treatment of severe vernal keratoconjunctivitis in
childhood. Pediatr Allergy Immunol 2006; 17:527–532.
27 Pucci N, Novembre E, Cianferoni A, et al. Efficacy and safety of cyclosporine
eyedrops in vernal keratoconjunctivitis. Ann Allergy Asthma Immunol 2002;
89:298–303.
28 Kilic A, Gurler B. Topical 2% cyclosporine A in preservative-free artificial tears
for the treatment of vernal keratoconjunctivitis. Can J Ophthalmol 2006;
41:693–698.
29 Friedlaender MH. Current concepts in ocular allergy. Ann Allergy 1991;
67:5–13.
30 Bonini S. Atopic keratoconjunctivitis. Allergy 2004; 59 (Suppl 78):71–
73.
31 Bonini S, Bonini S. Studies of allergic conjunctivitis. Chibret Int J 1987; 5:12–
22.
32 Bonini S, Bonini S. IgE and non-IgE mechanisms in ocular allergy. Ann Allergy
1993; 71:296–299.
33 Bonini S, Bonini S, Schiavone M, et al. Conjunctival hyperresponsiveness to
ocular histamine challenge in subjects with vernal conjunctivitis. J Allergy Clin
Immunol 1992; 89:103–107.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Molecular Vision 2007; 13:1562-7 <http://www.molvis.org/molvis/v13/a173/>
Received 17 March 2007 | Accepted 25 August 2007 | Published 30 August 2007
©2007 Molecular Vision
Natural killer cells in vernal keratoconjunctivitis
Alessandro Lambiase,1 Eduardo Maria Normando,1 Laura Vitiello,3 Alessandra Micera,1,2 Marta Sacchetti,1
Eleonora Perrella,6 Luigi Racioppi,3 Sergio Bonini,4,5 Stefano Bonini1
1
Interdisciplinary Center for Biomedical Research (CIR), Laboratory of Ophthalmology, University Campus Bio-Medico of Rome,
Rome Italy; 2IRCCS-G.B. Bietti Eye Foundation, Rome, Italy; 3Department of Biology and Molecular and Cellular Pathology,
Second University of Naples, Naples, Italy; 4Internal Medicine, Second University of Naples; Naples, Italy; 5Institute of Neurobiology and Molecular Medicine, National Research Council (INMM-CNR) of Rome, Italy; 6Pathology, University Campus Bio-Medico
of Rome, Italy
Purpose: Recent studies suggest that natural killer (NK) cells exert effector/regulatory properties on both innate and
adaptive responses via release of different cytokines. While some information indicates NK cells in allergic asthma and
atopic dermatitis, no data are available for allergic conjunctivitis. The aim of this study was to evaluate NK in the blood
and the conjunctiva of patients with vernal keratoconjunctivitis (VKC).
Methods: Six patients with active VKC and six healthy subjects were included in the study. Blood samples and conjunctival biopsies were taken from each patient. NK cells in blood and conjunctiva were quantified by flow cytometry and
immunohistochemistry, respectively. Clinical findings of the patients were recorded, conjunctival immune infiltrates were
characterized, and both parameters were correlated to NK cell number.
Results: Compared to healthy subjects, NK cells were significantly decreased in the blood and increased in the conjunctiva of patients with VKC.
Conclusions: Together with lymphocytes, eosinophils, and mast cells, NK cells constitute a significant proportion of the
immune cells infiltrating VKC conjunctiva. This finding indicates a potential role of NK and innate immunity in the
regulation of allergic reactions and in diseases such as VKC. New therapeutic alternatives for modulating allergic inflammation might target NK cells.
Vernal keratoconjunctivitis (VKC) is a chronic bilateral
inflammation of the conjunctiva characterized by hyperemia,
chemosis, photophobia, and mucous discharge. The hallmark
of the disease is the presence of giant papillae on the upper
tarsal conjunctiva or limbus [1]. Originally classified as an
allergic conjunctivitis-type disease, VKC was considered for
many years to be the expression of a classical type I immunoglobulin-E (IgE)-mediated hypersensitivity reaction of the
conjunctiva, according to the Coombs and Gell definition [2].
Recent studies have demonstrated that only 50% of patients
with VKC are sensitive to the skin/Radio-Allergo-Sorbent Test
(skin/RAST) [3], and that a more complex IgE-independent
pathogenic mechanism is involved with the contribution of
many cells and mediators detected in the serum, tears, and
conjunctiva of patients with VKC [4]. Conjunctival allergen
challenge and biochemical/functional studies indicate a Th2driven mechanism [5,6] for VKC, and a definition, similar to
that of asthma, of “an allergic inflammatory disease with mast
cells, eosinophils and lymphocytes” [7]. This traditional view
of the allergic reaction has been recently revisited, and an adjuvant role of innate immunity in allergic inflammation has
been proposed. Epithelial cells, dendritic cells (prototypical
antigen presenting cells), natural killer (NK) cells, as well as
mast cells/basophils, through expression of various membrane
receptors, particularly toll-like receptors (TLR), might also
participate in the innate immunity response by playing a regulatory role in allergy [8-10]. In line with this hypothesis, TLRs
have been shown to be differentially expressed in the conjunctiva of patients with VKC when compared to healthy subjects [11].
NK cells are granular lymphocytes that play a crucial role
in innate immunity due to their cytotoxic ability to destroy
virus-infected cells and certain tumor cell targets without prior
stimulation [12]. Recent data suggest that a subpopulation of
NK cells (NK-T) are important regulators of both innate and
acquired response through the release of several
immunoregulatory mediators (including TNFα, TNFβ, TGFβ,
GM-CSF, MIP-1α, IL-1, IL-2, IL-3, IL4, IL5, IL-8, IL10 and
IL-13) [13-16]. Indeed, NK cells can be triggered by specific
T-cell receptor activation to secrete cytokines that promote
Th2 responses instead of Th1 responses, suggesting that NK
cells might play a role in regulating the balance between Th1/
Th2 lymphocytes [15,16].
In the present study, we sought to compare NK cells in
the peripheral blood and in the conjunctiva of VKC patients
with those of healthy subjects.
Correspondence to: Professor Stefano Bonini, M.D., Chair of Ophthalmology, University Campus Bio-Medico, Via Emilio Longoni
83, 00155 Rome Italy; Phone: +39 06-22541342; FAX: +39 0622541456; email: [email protected]
METHODS
Patients and tissue handling: The study, performed in spring,
involved six patients with active VKC (males between 7-35
years old) and six healthy subjects with no history of atopic
1562
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Molecular Vision 2007; 13:1562-7 <http://www.molvis.org/molvis/v13/a173/>
©2007 Molecular Vision
ocular/systemic diseases (males between 24-26 years old).
VKC diagnosis was based on the presence of recurrent symptoms of itching, photophobia, and tearing in early spring. The
symptoms were associated with a mild to severe cobblestonelike appearance in the upper tarsal conjunctiva, mucous discharge, epithelial keratopathy, and at least two eosinophils per
optic field (x100/oil immersion) in the conjunctival scraping.
Two out of six patients showed sensitization to
Dermatophagoides pteronissinus with a skin prick test. Symptoms (itching, tearing, and photophobia) and signs (tarsal and
bulbar papillae, hyperemia, secretion, and corneal epithelial
involvement) were recorded and graded on a scale of 0-3 (0,
absent; 1, weak; 2, mild; and 3, severe). A total symptom score
(from 0-9) and a total sign score (from 0-15) were calculated.
Table 1 summarizes the characteristics of the patients included
in the study. One physician (A.L.) carried out all ocular examinations by slit lamp biomicroscopy. All patients were without treatment for at least one week prior to the study. Blood
samples and conjunctival biopsies were collected from both
VKC and healthy subjects and flow cytometry and immunohistochemistry were performed to identify circulating and conjunctival NK cells. Conjunctival biopsy from healthy subjects
was performed at the time of surgery, for strabismus.
The study adhered to the tenets of the Declaration of
Helsinki. Informed consent was obtained from both VKC and
healthy subjects, and institutional human experimentation committee approval was granted.
Flow cytometry: For specific staining, 150 µl of peripheral blood were pretreated with NH4CL-EDTA for 10 min at
room temperature to lyse erythrocytes It was then incubated
for 30 min at 4 °C with CD3-FITC, CD16-PE, or CD56-PerCP
conjugated monoclonal antibodies, according to the
manufacturer’s instructions (Simultest CD3/CD16+CD56;
Code 340042; Becton Dickinson Biosciences, San Jose, CA).
All samples were analyzed through a FACScan flow cytometer (Becton Dickinson) equipped with an argon laser emitting at 488 nm. Forward and side scatter signals were collected as linear signals, and all emissions were collected on a
four-decade logarithmic scale. FITC, PE, and PerCP signals
were measured, respectively at 530 nm, 575 nm and 670 nm.
Spectral overlap was minimized by electronic compensation
with Calibrite beads (Becton Dickinson) before each series.
CellQuest® software (Becton Dickinson) was used to acquire
and evaluate 5,000 events with preserved side scatter signals
and high membrane staining for specific antibodies.
Histological and immunohistochemical evaluations:
Conjunctival specimens were post-fixed in 4% ρ-formaldehyde-100 mM phosphate-buffered saline (PBS) and cut in 3
µm sections (HM 325 Microm; BioOptica, Milan, Italy). Sections were either processed for basic histology (hematoxylin
and eosin; BioOptica), immunohistochemistry, or immunofluorescence. Briefly, sections were stained with monoclonal
antihuman CD4 (1/50; Dako Corp, Carpenteria, CA), EG2 (1/
50; Peninsula, Upsala, Sweden), AA1 (1/200; R&D Systems,
Minneapolis, MN), and CD56 (undiluted clone T199; BD)
antibodies and developed using ABC-peroxidase (Vectastain
Elite ABC, Vector Laboratories, Inc., Burlingame, CA) or with
the appropriate fluorescent technique. As a negative control,
sections were stained with a nonspecific isotype antibody. Thelper lymphocytes (CD4+), activated eosinophils (EG2+),
mast cells (AA1+), and NK cells (CD56+) were counted under light microscopy, in a blind-fashion, in three optic fields
(40X magnification) for each of three randomly selected areas. Arkon32 software (version 10.06.06) was used for image
analysis. Data are shown as mean±SEM.
For fluorescent analysis, specific binding of the primary
antibody was detected using a cy2-conjugated donkey
antimouse-antirabbit-antigoat antibody (Jackson Laboratory,
West Grove, PA), and evaluated at 60X magnification in an
oil immersion (E2000U confocal microscope; Nikon, Tokyo,
Japan). Brightness and contrast level were evaluated using C1
software (Nikon), and the images were transferred to the Adobe
Photoshop 7.0 program (Adobe Systems Inc., San Jose, CA).
To detect nonspecific binding, we performed control immunofluorescent staining by substituting the primary antibody with
control isotype IgG (data not shown).
Statistical evaluation: The nonparametric Mann-Whitney
test (StatView II for PC; Abacus Concepts Inc., Barkley, CA)
was used for statistical comparison of the number of circulating and conjunctival immune cells in patients with VKC versus healthy subjects. The Spearman rho test was employed to
correlate the number of circulating and conjunctival NK cells
to signs, symptoms, and IgE serum levels and to the number
TABLE 1. CHARACTERISTICS OF PATIENTS WITH VERNAL KERATOCONJUNCTIVITIS
This table summarizes the characteristics of the patients included in
the study.
1563
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Molecular Vision 2007; 13:1562-7 <http://www.molvis.org/molvis/v13/a173/>
©2007 Molecular Vision
of circulating and conjunctival eosinophils. Data are represented in graphs as mean±SEM, and p values less than 0.05
were considered statistically significant.
RESULTS
Circulating NK cells (CD56+ and CD16+) were decreased in
patients with VKC compared to healthy subjects. The decrease
in NK cells was significant when considering NK cell number
(Figure 1A; VKC: 744±401 versus healthy subjects: 1554±649;
p<0.05) as well as percent NK cells (CD56+ and CD16+ cells/
CD3+ cells; VKC: 5.6%±1.9% versus healthy subjects:
10.9%±5%; Figure 1B; p<0.05).
Immunohistochemistry of the conjunctiva showed a significant increase of CD4+ T-helper lymphocytes (VKC:
56.1±17.5/optic field versus control: 5.6±2.6/optic field;
p<0.01), activated eosinophils (VKC: 30.9±8.3/optic field
versus control: 0±0/optic field; p<0.01) and AA1+ mast cells
(VKC: 41.3±11.6/optic field versus control: 2.2±2.5/optic field;
p<0.01) in patients with VKC compared to healthy subjects
(Figure 2).
CD56+-bearing NK cells were detected in all conjunctiva of patients with VKC and in 75% (4/6) of healthy subjects. Statistical analysis showed a significant (p<0.01) increase
in the number of CD56+ cells infiltrating the conjunctiva of
patients with VKC (24±10.5 cells/optic field) when compared
to healthy subjects (5.9±2.6 cells/optic field; Figure 3).
No significant correlations were observed between the
number of circulating or conjunctival NK cells and the signs
and symptoms scores or plasma IgE levels.
DISCUSSION
This report demonstrates that, relative to healthy normal subjects, patients with VKC have a decreased number of circulating NK cells and an increased number of NK cells together
with Th lymphocytes, activated eosinophils, and mast cells in
the conjunctiva.
NK cells play a crucial role in innate immunity, having
the ability to directly lyse virus-infected cells [12]. Aside from
their cytotoxic activity, NK cells can produce and release high
amounts of both Th1 (IFNγ) and Th2 (IL4, IL5, and IL13)
cytokines, enabling these cells to also regulate acquired immune response [13-16]. A new concept proposes classifying
NK cells by their predominant Th1 (NK-1) or Th2 (NK-2)
cytokine pattern [15]. Both subsets might inhibit or stimulate
aspects of the allergic and normal immune response by specific patterns of cytokine release [17]. Recently, it was proposed that NK cells play a crucial role in the pathogenesis of
allergic diseases by altering the balance between Th1/Th2 lymphocytes. NK cells might be triggered to secrete cytokines
(IL-4, IL-5, and IL-13) that promote Th2 rather than Th1 responses [15,16]. In an animal model of allergic asthma,
Schuster and coworkers detected increased numbers of NK
cells along with CD4 and CD8 expressing T cells in both
bronchoalveolar lavage fluid (BALF) and lung parenchyma
[18]. In a murine model of allergic peritonitis, NK-derived
IL-5 contributed to the observed eosinophil infiltration [19].
Furthermore, NK-specific depletion inhibited allergen-induced
pulmonary eosinophil and CD3-T cell infiltration, and blunted
the increase of IL-4, IL-5, and IL-12 in BALF [20]. Allergenspecific immunotherapy in humans was also shown to decrease
NK cell activity [21]. All these data indicate a key role of NK
cells in the control of allergic disease. The present findings of
decreased circulating NK in VKC patients appear at first to
Figure 1. Circulating natural killer cells in patients with vernal keratoconjunctivitis compared to healthy subjects. A: Flow cytometry
demonstrated a significant decrease of circulating natural killer cells
(cells/µl) in vernal keratoconjunctivitis (VKC) patients compared to
healthy subjects (p<0.05). B: The percent natural killer cell decrease
was significant (CD56+ and CD16+ cells/CD3+ cells; p<0.05).
1564
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Molecular Vision 2007; 13:1562-7 <http://www.molvis.org/molvis/v13/a173/>
©2007 Molecular Vision
diverge from the hypothesis that NK is an important regulator
of the allergic reaction. However, similar decreases in circulating NK cells have been described in atopic diseases such as
asthma and atopic dermatitis [22-24]. In these prior studies,
the decrease of circulating NK cells was shown to not be due
to any intrinsic defect in the ability of NK cells to proliferate,
but merely reflected accumulation of these cells in the site of
inflammation [22]. In line with this hypothesis, we demonstrated a significant increase of NK cells infiltrating the conjunctiva in inflamed VKC tissues. The number of NK cells in
VKC conjunctiva was similar to that of eosinophils—cells long
considered to be crucial players in the pathogenesis of VKC.
This finding indicates that NK cells may be involved in the
pathophysiology of VKC, modulating allergic inflammation
through the release of cytokines that influence the balance
between Th1 and Th2 responses and the resulting conjunctival eosinophil infiltration.
Surprisingly, no significant correlation was observed between the number of circulating or conjunctival NK cells and
the clinical signs and symptoms of VKC. This lack of correlation might indicate an all or none relationship with VKC that
is unaffected by changes in the severity signs and symptoms.
Conversely, it might simply reflect the low sample size of VKC
Figure 2. Evaluation of inflammatory cells in the conjunctiva of patients with vernal keratoconjunctivitis. The graph (A) illustrates a significant increase of T-helper lymphocytes (CD4+/green; B), activated eosinophils (EG2+/green; C), and mast cells (AA1+/green; D) in vernal
keratoconjunctivitis (VKC) conjunctiva compared to healthy subjects (E, F, G, respectively). No specific binding was detected when sections
were incubated with isotype IgG (data not shown; 40X magnification).
1565
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Molecular Vision 2007; 13:1562-7 <http://www.molvis.org/molvis/v13/a173/>
©2007 Molecular Vision
Figure 3. Immunohistochemical evaluation of natural killer cells in vernal keratoconjunctivitis conjunctiva. Graph A illustrates the significant
increase of natural killer cells in the conjunctiva of patients with vernal keratoconjunctivitis (VKC) compared to healthy subjects. Natural
killer cells were identified by CD56 expression quantified by immunohistochemistry (B=VKC and C=healthy subjects) and confocal analysis
(D=VKC and E=healthy subjects). No specific immune staining was observed in the presence of isotype IgG (F=control staining; 40X
magnification).
1566
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Molecular Vision 2007; 13:1562-7 <http://www.molvis.org/molvis/v13/a173/>
patients. A more extensive study including a larger population
is required to confirm these initial findings. Nonetheless, this
study indicates a potential role of NK cells in VKC pathophysiology as well as a link between innate and specific immunity in allergic diseases. These novel findings appear of
clinical relevance since a deeper understanding of the role of
NK in VKC might lead to new pharmacological strategies focused on selective modulation of Th1 and Th2 polarization of
NK cells, using factors such as IL-7, IL-15, and αgalactosylceramide [25,26].
ACKNOWLEDGEMENTS
This study was presented in part at the 2006 Association for
Research in Vision and Ophthalmology meeting (ARVO, Fort
Lauderdale, FL).
REFERENCES
1. Bonini S, Coassin M, Aronni S, Lambiase A. Vernal keratoconjunctivitis. Eye 2004; 18:345-51.
2. Coombs RRA, Gell PGH. The classification of allergic reactions
underlying disease. In: Gell PGH, Coombs RRA, editors. Clinical Aspects of Immunology. London: Blackwell; 1963. p. 317320.
3. Bonini S, Bonini S, Lambiase A, Marchi S, Pasqualetti P, Zuccaro
O, Rama P, Magrini L, Juhas T, Bucci MG. Vernal keratoconjunctivitis revisited: a case series of 195 patients with long-term
followup. Ophthalmology 2000; 107:1157-63.
4. Leonardi A. Vernal keratoconjunctivitis: pathogenesis and treatment. Prog Retin Eye Res 2002; 21:319-39.
5. Maggi E, Biswas P, Del Prete G, Parronchi P, Macchia D, Simonelli
C, Emmi L, De Carli M, Tiri A, Ricci M, Romagnani S. Accumulation of Th-2-like helper T cells in the conjunctiva of patients with vernal conjunctivitis. J Immunol 1991; 146:116974.
6. Metz DP, Bacon AS, Holgate S, Lightman SL. Phenotypic characterization of T cells infiltrating the conjunctiva in chronic allergic eye disease. J Allergy Clin Immunol 1996; 98:686-96.
7. Bonini S, Bonini S. IgE and non-IgE mechanisms in ocular allergy. Ann Allergy 1993; 71:296-9.
8. Dombrowicz D. Exploiting the innate immune system to control
allergic asthma. Eur J Immunol 2005; 35:2786-8.
9. Lambrecht BN, Hammad H. Taking our breath away: dendritic
cells in the pathogenesis of asthma. Nat Rev Immunol 2003;
3:994-1003.
10. Marone G, Triggiani M, de Paulis A. Mast cells and basophils:
friends as well as foes in bronchial asthma? Trends Immunol
2005; 26:25-31.
11. Bonini S, Micera A, Iovieno A, Lambiase A, Bonini S. Expression of Toll-like receptors in healthy and allergic conjunctiva.
Ophthalmology 2005; 112:1528; discussion1548-9.
12. Kiessling R, Klein E, Wigzell H. “Natural” killer cells in the
mouse. I. Cytotoxic cells with specificity for mouse Moloney
leukemia cells. Specificity and distribution according to geno-
©2007 Molecular Vision
type. Eur J Immunol 1975; 5:112-7.
13. Biron CA. Activation and function of natural killer cell responses
during viral infections. Curr Opin Immunol 1997; 9:24-34.
14. Scharton-Kersten TM, Sher A. Role of natural killer cells in innate resistance to protozoan infections. Curr Opin Immunol
1997; 9:44-51.
15. Stuhlsatz HW, Eberhard A, Kristin H, Vojtisek O, Greiling H.
[Glycosaminoglycans in the synovial fluid of chronic joint diseases (proceedings)]. Z Rheumatol 1976; 35:suppl444-54.
16. Hoshino T, Winkler-Pickett RT, Mason AT, Ortaldo JR, Young
HA. IL-13 production by NK cells: IL-13-producing NK and T
cells are present in vivo in the absence of IFN-gamma. J Immunol
1999; 162:51-9.
17. Korsgren M. NK cells and asthma. Curr Pharm Des 2002; 8:18716.
18. Schuster M, Tschernig T, Krug N, Pabst R. Lymphocytes migrate
from the blood into the bronchoalveolar lavage and lung parenchyma in the asthma model of the brown Norway rat. Am J
Respir Crit Care Med 2000; 161:558-66.
19. Walker C, Checkel J, Cammisuli S, Leibson PJ, Gleich GJ. IL-5
production by NK cells contributes to eosinophil infiltration in
a mouse model of allergic inflammation. J Immunol 1998;
161:1962-9.
20. Korsgren M, Persson CG, Sundler F, Bjerke T, Hansson T, Chambers BJ, Hong S, Van Kaer L, Ljunggren HG, Korsgren O. Natural killer cells determine development of allergen-induced eosinophilic airway inflammation in mice. J Exp Med 1999; 189:55362.
21. Sin B, Misirligil Z, Aybay C, Gurbuz L, Imir T. Effect of allergen
specific immunotherapy (IT) on natural killer cell activity (NK),
IgE, IFN-gamma levels and clinical response in patients with
allergic rhinitis and asthma. J Investig Allergol Clin Immunol
1996; 6:341-7.
22. Ikegami Y, Yokoyama A, Haruta Y, Hiyama K, Kohno N. Circulating natural killer T cells in patients with asthma. J Asthma
2004; 41:877-82.
23. Oishi Y, Sakamoto A, Kurasawa K, Nakajima H, Nakao A,
Nakagawa N, Tanabe E, Saito Y, Iwamoto I. CD4-CD8- T cells
bearing invariant Valpha24JalphaQ TCR alpha-chain are decreased in patients with atopic diseases. Clin Exp Immunol 2000;
119:404-11.
24. Takahashi T, Nakamura K, Chiba S, Kanda Y, Tamaki K, Hirai
H. V alpha 24+ natural killer T cells are markedly decreased in
atopic dermatitis patients. Hum Immunol 2003; 64:586-92.
25. Hong S, Wilson MT, Serizawa I, Wu L, Singh N, Naidenko OV,
Miura T, Haba T, Scherer DC, Wei J, Kronenberg M, Koezuka
Y, Van Kaer L. The natural killer T-cell ligand alphagalactosylceramide prevents autoimmune diabetes in non-obese
diabetic mice. Nat Med 2001; 7:1052-6.
26. van der Vliet HJ, Nishi N, Koezuka Y, von Blomberg BM, van
den Eertwegh AJ, Porcelli SA, Pinedo HM, Scheper RJ,
Giaccone G. Potent expansion of human natural killer T cells
using alpha-galactosylceramide (KRN7000)-loaded monocytederived dendritic cells, cultured in the presence of IL-7 and IL15. J Immunol Methods 2001; 247:61-72.
The print version of this article was created on 30 Aug 2007. This reflects all typographical corrections and errata to the article through that
date. Details of any changes may be found in the online version of the article. α
1567
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Manuscript
.
1
2
3
Tailored approach to the treatment of vernal keratoconjunctivitis
4
5
Marta Sacchetti MD1 , Alessandro Lambiase MD PhD1, Flavio Mantelli MD1, Velika
6
Deligianni MD2, Andrea Leonardi MD2Stefano Bonini MD1
7
8
1
9
2
Department of Ophthalmology, University of Rome, Campus Bio-Medico, Rome, Italy
Dept. of Neuroscience, Ophthalmology Unit, University of Padua, Padua, Italy
10
11
Meeting presentation: None
12
Financial Support: None
13
Conflict of Interest: No authors have any financial/conflicting interests to disclose
14
Running head: clinical grading of vernal keratoconjunctivitis
15
16
17
18
Address for reprints:
19
Prof. Stefano Bonini
20
Department of Ophthalmology
21
University of Rome, Campus Bio-Medico
22
Via Alvaro del Portillo, 21
23
00128 Rome, Italy
24
Phone number. +3906225419185
25
Fax. +390622541456
26
E-mail. [email protected]
27
28
1
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
29
Abstract
30
Purpose: To develop a standardized clinical grading system for the management of vernal
31
keratoconjunctivitis (VKC) patients and to identify the risk factors associated with a worsened
32
outcome of the disease.
33
Design: Retrospective cohort study
34
Participants: Two-hundred seven consecutive patients with VKC, referred to our center from
35
1997 to 2007, were included in the study. One-hundred ten of those patients were included in
36
the follow-up study (range 1-10 years).
37
Methods: Classification tree analysis (CART®) was performed to separate the patients into 5
38
subgroups by therapeutic approach. Regression tree analysis and multivariate logistic
39
regression analysis were performed during follow-up to identify predictors of worse visual
40
outcome.
41
Main Outcome Measures: Age, gender, duration and course of disease, signs, symptoms,
42
overall symptoms score, history of atopy, markers of allergy, best corrected visual acuity and
43
therapy were collected at baseline and during follow up. Number of relapses and the final best
44
corrected visual acuity were also evaluated in follow-up.
45
Results: A decision tree for VKC treatment was developed by CART analysis and a new
46
clinical grading system was proposed accordingly. Sixteen patients were classified as grade 0
47
(absence of symptoms and no therapy); 59 patients were grade 1 (presence of symptoms
48
without photophobia, occasional use of anti-allergic eye drop); 74 patients were graded as 2
49
(presence of symptoms including photophobia, daily anti-allergic treatment); 22 patients with
50
superficial punctuate keratopathy were graded as 3 (daily anti-allergic treatment associated
51
with occasional topical steroid); and 36 were graded as 4 (diffuse SPK and/or corneal ulcer;
52
pulsed high dose topical steroid). A higher number of relapses and a higher baseline grade of
53
VKC were the main predictor factors for worse visual outcome.
2
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
54
Conclusions: This grading system allows for identifying the more severe forms of VKC that
55
are at higher risk of recurrences, corneal ulcer, and worse final visual outcome.
56
3
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
57
Introduction
58
Vernal keratoconjunctivitis (VKC) is a chronic allergic disease with seasonal recurrences of
59
ocular surface inflammation characterised by intense itching, tearing, photophobia and
60
mucous discharge, associated with conjunctival hyperemia and chemosis.1-3 Most severe cases
61
show corneal signs of inflammation ranging from superficial punctate keratitis to corneal
62
ulcers that can lead to visual impairment.1,4, 5 Signs and symptoms of VKC are variable and
63
may present with daily fluctuations in individual patients. Episodes of acute itching and
64
redness lasting for several hours are often referred by the patients’ parents following short
65
symptom-free periods.
66
are variable among patients. As a consequence, the management of VKC is a challenge to
67
ophthalmologists, since the therapy needs frequent adjustments according to the specific
68
needs of each patient.1,2,6,8,9
69
Anti-allergic eye drops have been shown to control ocular signs and symptoms when used on
70
a routine basis while acute episodes of the disease require more potent agents such as ocular
71
topical steroids.8 These compounds are very effective but their use is limited due to possible
72
complications associated with chronic use, such as cataract development and glaucoma.1-5, 9-10
73
A standardized clinical grading system based on VKC severity has been recently proposed in
74
order to provide a common description of the disease and to avoid selection bias in the
75
recruitment of patients for clinical trials.11 However, a standardized therapeutic approach
76
corresponding to these different grades has not yet been defined.
77
In this study, we retrospectively review the clinical records of 207 patients with VKC
78
observed in our cornea and external disease Unit over the last ten years. On the basis of the
79
treatments prescribed in this patient population, we developed a decision tree for VKC
80
treatment that accurately reflects the clinical grading of the disease. We also identified the
4
1,3,6,7
Intervals between acute symptomatic and symptom-free periods
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
81
occurrence of relapses, variability of clinical grading during follow-up and the predictive
82
factors for worse clinical outcome, including final visual acuity.
83
5
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
84
Methods
85
Patients
86
We retrospectively reviewed the clinical records of 207 patients with VKC referred to our
87
Cornea and External Disease Unit from 1997 to 2007. Institutional Review Board
88
(IRB)/Ethics Committee approval was obtained. The diagnosis was based on a history of
89
ocular surface inflammation characterised by itching, photophobia, tearing and mucous
90
discharge, the presence of a papillary reaction on the upper tarsal conjunctiva and/or at the
91
limbus associated with the presence of eosinophils in conjunctival scrapings.1,10 Patients had a
92
complete examination by the same physician (SB) at least once a year. Additional visits were
93
planned by the physician according to the clinical severity of the disease or if required by
94
patients/parents in the case of worsening ocular symptoms.
95
The following clinical and demographic data were collected for each patient: age, gender,
96
familial history of atopy, associated ocular diseases, presence of associated atopic diseases,
97
positive reaction to skin PRICK tests, age of onset of VKC, seasonal/perennial course of
98
VKC, history of corneal shield ulcer and any previous topical treatments used. Each clinical
99
sign (conjunctival hyperemia, chemosis and secretion, upper tarsal and limbal papillary
100
reaction, subconjunctival fibrosis, corneal ulcer) and symptom (itching, tearing, burning and
101
photophobia) observed at the first clinical examination was assessed and scored: 0=absent,
102
1=mild, 2=moderate, and 3=severe. Corneal involvement was scored as 0=spared,
103
1=superficial punctate keratopathy in less than half the cornea, 2= superficial punctate
104
keratopathy in more than half the cornea, and 3= corneal ulcer. In addition, patients and/or
105
their parents were asked to score the overall symptoms according to the following scale:
106
0=absence of symptoms, 1=presence of mild intermittent symptoms, 2=presence of mild
107
persistent or moderate symptoms, 3= presence of severe symptoms. The best corrected visual
6
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
108
acuity (BCVA) and the topical treatments prescribed were also recorded and evaluated at each
109
visit.
110
111
Vernal keratoconjunctivitis decision tree
112
Classification tree (CT) analysis (CART® V6.0; Salford system, CA, USA) was performed on
113
the entire population (n=207) of patients with VKC in order to develop a decision tree for
114
treatment.
115
analysis:
12
Five therapeutic approaches were considered as dependent variables for the CT
116
-
Score 0 = no treatment;
117
-
Score 1 = anti-allergic eye-drop treatment used occasionally;
118
-
Score 2 = anti-allergic eye-drop treatment used daily;
119
-
Score 3 = anti-allergic eye-drop treatment used daily or associated with
120
low
121
dose topical steroid pulsed treatment (i.e. no more than 10-15 drops for
122
a month)
123
-
Score 4 = high dose pulsed treatment with topical steroids (4-6 times
124
daily for
125
-
3 days, tapered in one week).
126
The clinical sign (conjunctival hyperemia, chemosis and secretion, upper tarsal and limbal
127
papillary reaction, subconjunctival fibrosis, superficial punctate keratitis and corneal ulcer)
128
and symptom (itching, tearing, burning and photophobia) scores and the overall symptoms
129
score (OSS) collected at the first clinical examination were included in CT analysis as
130
independent variables.
131
The CART® method generates a classification procedure by partitioning the entire patient
132
population into subdivisions according to the clinical variable that produces the best split in
7
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
133
the population. All possible separations or cut-off points (for continuous variables) are
134
examined to determine which variable produces the best population split. In each of the
135
resulting strata, the process is repeated until none of the variables shows significant influence.
136
The resulting decision tree is composed of a root node (including all of the data), a set of
137
internal nodes (splits), and a set of terminal nodes. A class label is assigned to each terminal
138
node.12
139
140
141
Follow-up study
142
Patients with at least 1 year of follow-up (n=110) were included in this phase of the study.
143
Vernal keratoconjunctivitis severity at the time of each follow-up visit was retrospectively
144
graded according to the new decision tree. All patients with incomplete follow-up visits and
145
patients included in clinical trials requiring pre-established control visits and treatments were
146
excluded.
147
At the end of the follow-up period, the mean number of recurrences of ocular inflammation
148
per year, the development of corneal shield ulcer, the mean number of visits per year and the
149
mean number of changes in clinical grading were evaluated as outcome parameters. The
150
BCVA at the last examination in the quiescent phase was also recorded. Lastly, any
151
development of long term ocular complications (i.e. glaucoma and cataract) was noted.
152
Bivariate and multivariate logistic regression analyses were performed to obtain a relative risk
153
evaluation of worse visual outcome associated with the potential predictor variables. A
154
regression tree of predictors of worse visual outcome was constructed using the CART®
155
method. 12,13 The following clinical and demographic features were used as predictor variables
156
for a worse BCVA at the final examination: 1) gender (male/female); 2) course of VKC
157
(seasonal/perennial); 3) presence of associated atopic diseases (yes/no); 4) familial history of
8
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
158
atopy (yes/no); 5) history of corneal ulcer (yes/no); 6) upper tarsal papillary reaction score (0-
159
3); 7) limbal papillary reaction score (0-3); 8) recurrence rate of inflammation during the
160
follow-up period; 9) total duration of disease (years); 10) VKC grade at presentation (VKC
161
grade 0-4); 11) age of onset of VKC (years).
162
To perform logistic regression analyses, the final BCVA was used as a dependent variable:
163
patients with a final BCVA of 1 were classified as having “excellent vision“, patients with a
164
final BCVA<0.9 were classified as having “fair/poor vision”.
165
166
167
Statistics
168
The classification regression tree analysis (CART® V6.0; Salford system, CA, USA) was
169
performed to develop a decision tree for treatment of VKC and to identify predictive factors
170
for a worse visual outcome.
171
Bivariate logistic regression analyses were conducted to examine the relationship between
172
each demographic and clinical potential predictive factor and final BCVA (outcome variable).
173
Lastly, all significant predictors resulting from the bivariate analysis were included in a
174
multivariate logistic regression analysis for predicting fair/poor final BCVA. The clinical
175
grading of patients at the first visit was correlated to the mean number of recurrences of
176
inflammation per year, to the mean number of visits and to BCVA at the final examination,
177
using the Spearman rho test (SPSS V15 software, Illinois, CA, USA).
178
179
9
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
180
Results
181
VKC decision tree
182
Two-hundred seven patients with VKC were included in the tree analysis. The demographic
183
and clinical characteristics of the population are described in Table 1.
184
The VKC decision tree is shown in Figure 1. The most optimal tree was generated by splitting
185
the population by overall symptoms score (OSS): patients without symptoms (OSS=0) were
186
graded as 0-quiescent (n=16). The presence of ocular symptoms (OSS>1) but not photophobia
187
identified patients with grade 1-mild VKC (n=59), while patients graded as 2-moderate
188
(n=74) also complained of photophobia. Patients with corneal involvement were graded as 3-
189
severe (mild to moderate SPK; n=22) and 4-very severe (diffuse SPK and/or corneal ulcer;
190
n=36) based on the severity of corneal involvement. This new VKC grading system and
191
related treatments are summarized in Table 2.
192
Follow-up study
193
One-hundred and ten patients were included in the follow-up analysis (range 1-10 years;
194
mean ± SD: 4 ± 2 years). Twenty-four were females and 86 were males, aged from 4 to 31
195
years (mean, 10 ± 6 years).
196
During the entire follow-up period, patients underwent 2.3 ± 1.9 (mean ± SD) visits per year,
197
showing changes in VKC grade from 0 to 8 times per year (mean ± SD: 2 ± 1.6 changes per
198
year). Patients had from 0 to 3.5 recurrences per year (mean ± SD: 0.4 ± 0.6 recurrences for
199
year). Moreover, 14% of patients developed a corneal shield ulcer and 30% of patients
200
showed complete recovery of the disease after a mean duration of 10 ± 6 years. The BCVA at
201
final examination ranged from 0.2 to 1 (mean ± SD: 0.9 ± 0.1). No patients developed
202
glaucoma and/or cataract during the follow-up period.
10
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
203
A higher VKC grade at the first examination was significantly related to a higher number of
204
recurrences per year (p<0.001; rho=0.36), a higher number of visits (p=0.002; rho=0,29) and
205
a worse final BCVA (p=0.001; rho=-0.36).
206
All 11 potential predictive factors were included in the regression tree model performed with
207
CART® to predict a worse BCVA. The CART® decision tree for VKC treatment is shown in
208
Figure 2. The mean recurrence rate of inflammation appeared at the root node: patients (n=9)
209
with a higher mean recurrence rate (> 1.1 per year) showed a higher risk of worse visual
210
outcome (mean ± SD BCVA: 0.6±0.3). The remaining patients were then split based on VKC
211
grade at presentation and then by age of onset of VKC: a higher baseline VKC grade and
212
lower age of onset resulted in a mean BCVA of 0.7±0.2 (i.e., medium risk). Conversely, a
213
lower baseline VKC grade and a higher age of onset were associated with a lower risk of
214
visual impairment (mean ± SD BCVA: 0.9 ± 0.1).
215
Bivariate logistic regression analysis revealed a significant risk for worse BCVA with the
216
following factors: a perennial VKC course (p=0.013), the limbal VKC form (p=0.036), a
217
history of corneal ulcer (p=0.004), the severity of baseline VKC grade (p<0.05) and mean
218
recurrences of ocular inflammation per year (p=0.001). Multivariate logistic regression,
219
conducted with all significant risk items included as predictors, showed that the number of
220
recurrences per year (p=0.003) and a more severe baseline VKC grade at presentation
221
(p=0.048) were significantly associated with worse final visual outcome.
222
223
11
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
224
Discussion
225
We retrospectively analysed data from 207 patients with VKC treated in our Cornea and
226
External Disease Unit over a 10-year period. Results showed that these patients underwent
227
from 1 to 9 examinations per year and showed a great variability of clinical manifestations
228
with improvement and/or worsening of clinical signs and symptoms up to 8 times per year.
229
Such high clinical variability forces the physician to almost constantly check and modify the
230
patient’s treatment .1,4,8 A simple clinical decision tree and a grading system that allows
231
ophthalmologists to share a common language in the assessment and treatment of VKC and in
232
the development of clinical trials on potential new therapeutic compounds, would greatly
233
improve the management of this challenging disease.1,6,8
234
Starting from the retrospective evaluation of therapies used in our case series of 207 VKC
235
patients, we developed a standardized grading system using CART®, a statistical approach to
236
generating a decision tree.14,15,16 Classification tree analysis has the advantage that the results
237
are easier to interpret than in conventional statistical analyses. In fact, decision trees have
238
intuitive appeal because the classification structure is explicit. In our study, the decision tree
239
obtained allowed us to identify five classes of VKC severity, characterised by different signs
240
and symptoms and requiring different therapeutic approaches. Our analysis identified the
241
presence of ocular symptoms and corneal involvement as the two most important features of
242
VKC that influence therapy. The overall presence and severity of ocular symptoms should be
243
considered the foremost parameter when prescribing topical anti-allergic therapy1,4,6,8-10 The
244
frequency of instillation of ocular therapy may be decided by the course of symptomatology:
245
anti-allergic eye drops may be used as needed in patients with mild intermittent symptoms, or
246
daily in patients complaining of persistent symptoms. 17-19 Of ocular surface symptoms, the
247
presence of photophobia appears to discriminate the most severe stages, which are mostly
248
characterized by corneal involvement. In these cases, topical steroids are successfully used to
12
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
1,4,6,8
249
control ocular inflammation.
250
stages of disease, these parameters were not appropriate splitting criteria for the decision tree,
251
although they still are considered the main diagnostic criteria of VKC.
252
The new VKC grading system proposed in this study is based on a retrospective analysis and,
253
therefore, its validity should be confirmed by a prospective study. Nevertheless, it must be
254
noted that the VKC grading system developed using CART® alone correctly identified
255
patients with more severe forms of VKC, since severity grade was significantly related to a
256
higher number of recurrences per year, a higher number of visits and a lower final BCVA.
257
Similarly, the logistic regression analysis showed that a higher recurrence rate and higher
258
grade of VKC at presentation were associated with a higher risk of poor visual outcome.
259
These same predictive factors were identified by the regression tree analysis performed with
260
CART. Furthermore, CART identified a lower age of VKC onset as an additional risk factor
261
for a worse final visual outcome.
262
Our results indicate that VKC patients with frequent recurrences of inflammation and/or those
263
with a severity grade of 3 or 4 (i.e., with corneal involvement), and a lower age of onset of the
264
disease, need to be more closely followed and treated with a more aggressive approach to
265
control the disease and to prevent a reduction in BCVA. The therapeutic approach described
266
in this study allowed us to reduce long-term complications due to prolonged or self-
267
administered topical steroids, which was shown in our previous case series of 195 patients to
268
be responsible for glaucoma in 2.1% of patients and cataract in one patient.1 Furthermore,
269
this new approach to clinical grading of VKC might be incorporated into clinical trials to
270
improve evaluation of new treatment options that better control signs, symptoms and
271
recurrences of VKC.
272
In conclusion, in this study, we propose a new clinical grading system for VKC based on a
273
simple decision tree that can be easily applied to patients by any ophthalmologist. Our aim is
13
Since itching and conjunctival papillae are present in all
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
274
to achieve a standardized approach to VKC treatment based on clinical severity of the disease
275
as defined by the decision tree. This new grading system will also allow us to identify severe
276
forms of VKC, patients who are at higher risk of developing recurrences, corneal ulcer, and a
277
worse final visual outcome, and should therefore be followed by ophthalmologists on a more
278
frequent basis or addressed to referral centers for corneal diseases.
279
14
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
280
References
281
1.
Bonini S, Bonini S, Lambiase A, et al. Vernal keratoconjunctivitis
282
revisited: a case series of 195 patients with long-term follow-up. Ophthalmology.
283
2000;107:1157–63
284
2.
285
Leonardi A. Vernal keratoconjunctivitis: pathogenesis and treatment.
Prog Retin Eye Res 2002;21:319–39.
286
3.
Bonini S, Coassin M, Aronni S, et al. Vernal Keratoconjunctivitis. Eye.
287
2004;18:345-51.
288
4.
Leonardi A, Busca F, Motterle L et al. Case series of 406 vernal
289
keratoconjunctivitis patients: a demographic and epidemiological study. Acta
290
Ophthalmol Scand. 2006;84:406-10.
291
5.
292
Ophthalmol. 1999;34:88-92.
293
6.
294
demographic and epidemiological study on vernal keratoconjunctivitis: a glimpse of
295
ocular surface in Italian population. Ophthalmic Epidemiol. 2009;16:38-41
296
7.
297
quality of life in children with vernal keratoconjunctivitis questionnaire. Am J
298
Ophthalmol. 2007;144:557-63.
299
8.
300
randomised clinical trials on topical treatments for vernal keratoconjunctivitis. Br J
301
Ophthalmol. 2007;91:1656-61.
302
9.
303
2003;43:41–58.
15
Tabbara KF. Ocular complications of vernal keratoconjunctivitis. Can J
Lambiase A, Minchiotti S, Leonardi A et al. Prospective, multicenter
Sacchetti M, Baiardini I, Lambiase A et al. Development and testing of the
Mantelli F, Santos MS, Petitti T, et al. Systematic review and meta-analysis of
Leonardi A, Secchi AG. Vernal keratoconjunctivitis. Int Ophthalmol Clin
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
304
10.
305
allergy. J Allergy Clin Immunol. 2000;106:1019-32.
306
Bielory L. Allergic and immunologic disorders of the eye. Part II: ocular
11.
307
Bonini S, Sacchetti M, Mantelli F, Lambiase A. Clinical grading of
vernal keratoconjunctivitis. Curr Opin Allergy Clin Immunol. 2007;7:436-41.
308
12. Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and
309
Regression Trees. Wadsworth & Books/Cole Advanced Books & Software, Monterey,
310
CA, 1984.
311
13. Worth AP, Cronin MTD The use of discriminant analysis, logistic
312
regression and classification tree analysis in the development of classification models
313
for human health effects. J Mol Structures (Theochem). 2003; 622:97-111
314
14. Muller R, Möckel M. Logistic regression and CART in the analysis of
315
multimarker studies. Clin Chim Acta. 2008;394:1-6.
316
15.
317
Podgorelec V, Kokol P, Stiglic B, Rozman I. Decision trees: an
overview and their use in medicine. J Med Syst. 2002;26:445-63.
318
16. Costanza MC, Paccaud F. Binary classification of dyslipidemia from the
319
waist-to-hip ratio and body mass index: a comparison of linear, logistic, and CART
320
models. BMC Med Res Methodol. 2004;4:7
321
17. Verin P, Allewaert R, Joyaux JC et al. Comparison of lodoxamide 0.1%
322
ophthalmic solution and levocabastine 0.05% ophthalmic suspension in vernal
323
keratoconjunctivitis. Eur J Ophthalmol. 2001;11:120-5.
324
18. Avunduk AM, Avunduk MC, Kapicioglu Z et al. Mechanisms and
325
comparison of anti-allergic efficacy of topical lodoxamide and cromolyn sodium
326
treatment in vernal keratoconjunctivitis. Ophthalmology. 2000;107:1333-7.
16
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
.
327
19. Verin PH, Dicker ID, Mortemousque B. Nedocromil sodium eye drops are
328
more effective than sodium cromoglycate eye drops for the long-term management of
329
vernal keratoconjunctivitis. Clin Exp Allergy. 1999;29:529-36.
17
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
* Precis
Precis (35 words)
This study presents a decision tree for vernal keratoconjunctivitis based on a classification regression
analysis that provides an intuitive means of optimizing treatment and identifying patients at higher risk
and in need of closer follow-up.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Table 1
Table 1 Characteristics of patients included in this retrospective study of VKC patients
followed over a ten year period in our referral center.
Patients (N)
207 (%)
Sex
Male
162 (78%)
Female
45 (22%)
Age (years)
Range
3-32
Mean ± SD
10±6
Age of onset of VKC (years)
Range
0.5-26
Mean ± SD
6.2±4.5
VKC type (N)
Tarsal
151 (73%)
Limbal
20 (10%)
Mixed
36 (17%)
VKC course (N)
Seasonal
143 (69%)
Perennial
64 (31%)
Patients with atopic
91 (44%)
associated diseases (N)
Skin PRICK tests (N)
Positive
98 (47.3%)
Negative
69 (33.3%)
Not done
40 (19.3%)
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Table 2
Table 2. Clinical grading of VKC obtained from the classification tree analysis (CART®)
Grade
Clinical findings
Treatment
0 quiescent
Absence of symptoms
No treatments
1 mild
Presence of symptoms with no corneal
Anti-allergic eye drops occasionally
involvement
2 moderate
Presence of symptoms associated with
Anti-allergic eye drops daily
photophobia with no corneal involvement
3 severe
Presence of symptoms associated with
Anti-allergic eye drops daily
photophobia and mild to moderate SPK
associated with pulsed low dose
topical steroid
4 very severe Presence of symptoms associated with
Pulsed high dose topical steroid
photophobia and diffuse SPK and/or corneal ulcer eventually associated with surgical
removal of corneal plaque
Figure 1
Click here to download high resolution image
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Figure 2
Click here to download high resolution image
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Legends
Figure Legends
Figure 1. Classification tree analysis (CART®) stratified the VKC population into 5 subsets defined
by severity grade of signs and symptoms.
Figure 2. Regression tree analysis (CART®) identified that a higher frequency of recurrences, a
more severe VKC grade and a younger age of onset of VKC were risk factors for a worse visual
outcome.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Graefes Arch Clin Exp Ophthalmol (2008) 246:435–441
DOI 10.1007/s00417-007-0682-6
INFLAMMATORY DISORDERS
Preliminary evidence of the efficacy of probiotic eye-drop
treatment in patients with vernal keratoconjunctivitis
Alfonso Iovieno & Alessandro Lambiase &
Marta Sacchetti & Barbara Stampachiacchiere &
Alessandra Micera & Stefano Bonini
Received: 20 February 2007 / Revised: 11 July 2007 / Accepted: 25 August 2007 / Published online: 27 November 2007
# Springer-Verlag 2007
Abstract
Background Probiotics have been shown to improve allergic
inflammation. The aim of this study was to evaluate the
efficacy of Lactobacillus Acidophilus eye-drops in controlling
signs and symptoms of vernal keratoconjunctivitis (VKC).
Methods Seven patients (mean age 11.8±4.3; five M,
two F) with mild to moderate VKC were included in the
study. Lactobacillus Acidophilus diluted in saline solution
(2×108 CFU/ml) was administrated as eye-drops four times
daily for 4 weeks in both eyes. Clinical signs (conjunctival
hyperemia, chemosis, secretion, Trantas dots, superficial
punctuate keratitis) and symptoms (itching, photophobia,
burning, tearing) were evaluated and scored from 0 to 3 at
baseline, after 2 and 4 weeks of treatment. Total sign (TSS)
and symptom (TSyS) scores were calculated. Conjunctival
impression cytology was performed in three patients at
baseline and after 4 weeks of treatment, in order to evaluate
the expression of ICAM-1 and TLR-4.
Results In the six out of seven patients who completed the
study, symptoms were significantly improved after both
2 weeks (TSyS: baseline 6.7±0.9 vs 4.1±1.2; p=0.017) and
4 weeks (TSyS: baseline 6.7±0.9 vs 3.6±1.2, p=0.011) of
treatment. A significant improvement of clinical signs was
observed after 4 weeks of treatment (TSS: baseline 7.5±1.6
vs 3.9±1.7, p=0.034) but not after 2 weeks of treatment
(TSS: baseline 7.5±1.6 vs 5.3±1.5; NS). In particular,
photophobia was significantly reduced (2±0.6 vs 1±0.3;
p=0.023) at 2 weeks, while at 4 weeks the scores for
itching (1.8±0.3 vs 1±0.3), tearing (1.6±0.4 vs 0.8±0.2),
conjunctival hyperemia (2.3±0.2 vs 1.4±0.5) and chemosis
(1.2±0.4 vs 0.4±0.4) were significantly lower compared to
baseline. A down-regulation of ICAM-1 and TLR-4 was
observed in two patients showing clinical improvement
after 4 weeks of treatment.
Conclusion Our open pilot study showed that 1-month
treatment with probiotic eye-drops improves signs and symptoms in patients with VKC. Additional double-blind controlled
clinical trials with a larger sample of patients are needed to
confirm the effects of topical Lactobacilli on VKC patients.
Keywords Vernal keratoconjunctivitis . Allergy .
Conjunctiva . Lactobacillus Acidophilus . Probiotic
Introduction
Presented at the annual meeting of the Association for Research in Vision
and Ophthalmology (ARVO), Fort Lauderdale, Florida, May 2006.
A. Iovieno : A. Lambiase : M. Sacchetti : B. Stampachiacchiere :
A. Micera : S. Bonini (*)
Interdisciplinary Center for Biomedical Research (CIR),
Laboratory of Ophthalmology,
University of Rome “Campus Bio-Medico”,
Via E. Longoni, 83,
00155 Rome, Italy
e-mail: [email protected]
B. Stampachiacchiere : A. Micera
IRCCS-G.B. Bietti Eye Foundation,
Rome, Italy
Vernal keratoconjunctivitis (VKC) is a chronic allergic eye
disease affecting children in pre-puberal age. However,
VKC is not associated with a positive skin test or RAST in
42–47% of patients, confirming that it is not solely an IgEmediated disease, but that other mechanisms are involved in
VKC pathogenesis [2, 3]. It is characterized by recurrent
ocular surface inflammation leading to conjunctival hyperemia, mucus discharge and tarsal and/or bulbar papillary
reaction. Patients complain of intense ocular symptoms
such as itching, photophobia, burning and tearing, lasting
all year with seasonal recurrences [2, 3].
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
436
Graefes Arch Clin Exp Ophthalmol (2008) 246:435–441
Topical antiallergic treatment is commonly used to reduce
signs and symptoms of the disease but is not always
successful. Topical cyclosporine has shown good effectiveness in long-term maintenance of clinical remission in VKC
patients, but it is not commercially available for the treatment
of VKC [2, 3]. Topical steroids represent the most effective
therapy for moderate to severe forms of VKC; however, their
long-term use should be strictly limited as it exposes patients
to potential ocular side effects. If untreated, VKC leads to
severe corneal complications and visual impairment [2, 3].
A novel therapeutic approach to allergic diseases based on
the oral administration of probiotic bacteria has been recently
proposed [5, 18, 27, 30]. Probiotics are defined as “live
microorganisms which when administered in adequate
amounts confer a health benefit on the host” [11]. The
best-known and commonly used probiotics are strains of
Bifidobacterium and Lactobacillus species. Lactobacilli are
nonpathogenic, gram-positive bacteria, and represent the
major components of the commensal microbial flora of the
small and large intestinal tract of both humans and animals.
Previous clinical trials demonstrated the efficacy of
Lactobacilli therapy for the prevention and treatment of
atopic dermatitis, food allergy and allergic rhinitis [14–16,
23, 28, 31]. The health-promoting properties attributed to
Lactobacilli strains are multiple, and include their capacity
to interact with the host immune system. The ingestion of
Lactobacilli has been shown to enhance IL-10 serum
concentrations in patients with atopic dermatitis, therefore
displaying anti-inflammatory activities [24]. The chronic
use of Lactobacilli may strengthen the mucosal immunological barrier of the gut through the promotion of local IgA
production and the reduction of epithelial permeability to
allergens [1, 9, 10, 17]. In vitro studies have demonstrated
that Lactobacilli are able to induce Th1-type cytokines such
as IL-12 and IFN-γ; the stimulation of the Th1 phenotype
may normalize the Th1/Th2 imbalance present in allergic
conditions [19, 26].
Since VKC is mainly characterized by the increase of Th2type cytokines and by conjunctival immune cell infiltration,
the aim of this study was to investigate the effects of the
topical administration of Lactobacillus Acidophilus on signs
and symptoms of patients with active VKC.
Materials and methods
Lactobacillus Acidophilus eye drops were prepared as
follows: freeze-dried inactivated Lactobacillus Acidophilus
(Lacteol forte, Bruschettini srl, Genova, Italy) was diluted in
saline solution (NaCl 0.9% solution) to obtain a final
concentration of 200 millions CFU/ml. The preparation was
then aliquoted in eye-drop bottles at PH 7–7.4 and stored at
−70°C until use. The eye-drop solution was prepared once
for the 4 weeks of treatment under the hood in the hospital
pharmacy using sterile eye-drop bottles, therefore preserving
a sterile condition, aliquoted in eye-drop bottles at PH 7–7.4
and stored at −70°C. One bottle of eye-drop solution (7 ml)
was given to the patient once every week, for 1 month. The
patients were instructed to keep the eye-drops bottles at 4°C.
This study followed the guidelines of the Declaration of
Helsinki for research involving human subjects, and
approval was received from The Intramural Committee, in
accordance with the ethical principles for medical research
involving human subjects. Informed consent was obtained
from each patient or his/her parents.
Seven patients with mild to moderate VKC in the active
phase (mean age 11.8±4.3 years; range: 7–17 years; sex:
five M, two F; Table 1) were included in the study during
Table 1 Characteristics of patients enrolled in the study
Patient
Age/
gender
VKC
form
Duration
(ys)
Previous
therapies
*TSyS
(baseline)
*TSyS (postLactobacilli treatment)
**TSS
(baseline)
**TSS (postLactobacilli treatment)
1
13/M
4
Lodoxamide
12
8
10
8
2
13/M
4
Ketotifen
16
14
20
19
3
9/F
4
Lodoxamide
16
12
25
19
4
7/M
6
Ketotifen
16
8
18
6
5
7/M
2
Ketotifen
6
6
6
6
6
17/M
2
None
16
12
14
12
7
17/F
Tarsal/
perennial
Mixed/
perennial
Tarsal/
perennial
Mixed/
perennial
Tarsal/
seasonal
Limbal/
seasonal
Tarsal/
seasonal
9
Ketotifen
12
0
12
0
*TSyS = total symptoms score; **TSS = total sign score.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Graefes Arch Clin Exp Ophthalmol (2008) 246:435–441
springtime. Diagnosis of VKC was based on history,
clinical presentation (presence of mild to severe cobblestone-like appearance in the upper tarsal and/or limbal
papillary reaction) and the presence of eosinophils in upper
tarsal conjunctival scrapings. None of the patients were
using any form of systemic therapy or contact lenses, had
corneal ulceration, had a history of infectious conjunctivitis,
or had undergone eye-surgery in past three months.
After 3 days of wash-out, in which patients were only
treated with artificial tears and cold compresses, patients
received probiotic eye-drops four times daily in both eyes
for 1 month.
Clinical symptoms (itching, photophobia, burning and
tearing) and signs (conjunctival hyperemia, chemosis,
secretion, Trantas dots and superficial punctuate keratitis)
were evaluated according to slit lamp examination and
fluorescein staining, and scored from 0 to 3 (0=absent, 1=
mild, 2=moderate, 3=severe) at baseline, after 2 weeks and
after 4 weeks of treatment with probiotic eye-drops. Total
sign (TSS; range: 0–24) and symptom (TSyS; range: 0–30)
scores were calculated as the sum of each symptom and
sign score. At each time point, patients were asked about
the tolerability of Lactobacillus eye-drops. Tolerability was
expressed as a score from 0 to 3 (0=no discomfort, 1=mild
discomfort, 2=moderate discomfort, 3=severe discomfort,
cannot use study drug).
Conjunctival impression cytology (Millicell 0.22 μm
filters, Millipore, Milan, Italy) was performed at baseline
and after 1 month of Lactobacillus Acidophilus eye drop
treatment in the three patients who had given their written
consent to sampling (patients n° 4-5-6; see Table 1).
Millicell metilcellulose membranes were removed from
plastic supports with a surgical blade and placed in an
autoclaved microtube containing 300 μl cell lysis solution
(Puregene RNA purification kit; Gentra Systems, MI,
USA). Membranes were immediately processed to obtain
maximum recovery of total RNA from each sample. Total
RNA was reverse transcribed, and amplification reaction
437
was carried out in a programmable PTC100 thermocycler
and an Opticon2 machine respectively (MJ Research,
Watertown, MA, USA) as described elsewhere [4] (Table 2).
Samples were amplified in duplicate and from these
replicates, averages were calculated and differences in C(t)
data were evaluated by the REST software package [25]. Target
gene expressions were shown in the graph as percentages of
increase/decrease values that were obtained after calculating
differences between real pre and post Ct values.
All sterile RNase-Free plasticware and analytical
reagents were purchased from NUNC (Roskilde, Denmark),
Euroclone (Milan, Italy) and GIBCO-Invitrogen (Carlsbad,
CA, USA), unless otherwise specified in the text.
The non-parametric Mann-Whitney U-test was used to
compare signs and symptoms at different time-points.
Analysis was performed by using the statistical package
StatView II for PC (Abacus Concepts Inc., Berkley, CA,
USA) [32]. A probability <0.05 was considered statistically
significant. All data is reported as mean ± SEM.
Results
Six out of seven patients (86 %) completed the entire study.
Patient 3 discontinued treatment because there was no
improvement in his clinical condition, and dropped out from
the study at day 14. No side-effects were observed during
clinical examination, and all patients tolerated probiotic eyedrop administration (0 score at each time point).
All six patients (100%) reported improvement of clinical
conditions after 2 weeks of treatment, and five out of six
patients (83%) reported improvement of clinical conditions
after 4 weeks of treatment. Accordingly, total symptom
score (TSyS) was significantly lower after both 2 weeks
(TSyS 6.7±0.9 vs 4.1±1.2; p=0.017) and 4 weeks (TSyS:
6.7±0.9 vs 3.6±1.2, p=0.011) of treatment when compared
to baseline (Fig. 1a). In particular, photophobia was
Table 2 Sequence of primers used for gene amplification in real-time PCR
Gene (amplicon size)
Sequence
Reference
ICAM-1 (107 bp)
Sense: 5′-ATGAGTGCCCAGGGAATATG-3′
Antisense: 5′-CCCTGATCACTGCAGGAAA -3′
Sense: 5′-AAT CCC CTG AGG CAT TTA GG-3′
Antisense: 5′- CAG GGC TAA ACT CTG GAT GG-3′
Sense: 5′-GAA GGG GTC ATT GAT GGC AAC-3′
Antisense: 5′- GGG AAG GTG AAG GTC GGA GTC-3′
J03132
TLR-4 (102 bp)
GAPDH (100 bp)
U88880
BC013310
cDNAs were run for amplification with primers (10 pM, prepared by MWG, Biotech, Ebersberg, Germany) specific for ICAM-1 and TRL4
designed by the primer3 software available online at http://www-genome.wi.mit.edu/cgi-bin/primer/primer3_www.cgi [29]. GenBank software
was used to select the mRNA complete sequence of each gene investigated (http://www.ncbi.nlm.nih.gov/ Genbank; provided to the public
domain by the National Center for Biotechnology Information, Bethesda, MD, USA). The PCR amplification profile included: 1 cycle of
activation 95°C/15 min followed by 43 cycles of denaturation at 94°C/30 sec, annealing at 60°C/25 sec and extension at 75°C/30 sec, completed
by a further extension at 75°C/5 min.
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
438
Graefes Arch Clin Exp Ophthalmol (2008) 246:435–441
Fig. 1 Effect of Lactobacillus Acidophilus eye-drops on symptoms of
VKC patients. a Total symptom score at different time-points. A
significant improvement (*) in TSyS was observed after 2 and 4 weeks
of treatment. b Symptom scores at different time-points. Photophobia
was significantly improved (*) after 2 weeks of treatment while
itching and tearing were significantly in improved after 4 weeks of
treatment
significantly improved (2±0.6 vs 1±0.3; p=0.023) at two
weeks time-point, while at 4 weeks time-point itching
(1.8±0.3 vs 1±0.3) and tearing (1.6±0.4 vs 0.8±0.2) were
significantly improved (Fig. 1b).
A significant improvement in total sign score (TSS)
was observed after 4 weeks of treatment with respect to
baseline (TSS: 7.5±1.6 vs 3.9±1.7, p=0.034) but not after
2 weeks (TSS: 7.5±1.6 vs 5.3±1.5; NS) (Fig. 2a). In
particular, conjunctival hyperemia (2.3±0.2 vs 1.4±0.5)
and chemosis (1.2±0.4 vs 0.4±0.4) scores were significantly lower at the 4-week time-point compared to
baseline (Figs. 2b, 3).
Figure 4 shows modifications of conjunctival epithelial
expression of ICAM-1 and TLR-4 after 4 weeks of
treatment with Lactobacillus Acidophilus eye-drops. Interestingly, a down-regulation of both ICAM-1 and TLR-4 was
observed in patient 4 and patient 6, and both these patients
showed clinical improvement after 4 weeks of treatment. On
the other hand, up-regulation of both conjunctival markers
was observed in patient 5, who showed no improvement
after treatment.
Discussion
Fig. 2 Effect of Lactobacillus Acidophilus eye-drops on clinical signs
of VKC patients. a Total sign score at different time-points. A
statistically significant improvement (*) of TSS was observed after
4 weeks of treatment. b Symptom scores at different time-points The
improvement in hyperemia and chemosis reached statistical significance (*) at the 4-week time-point
This pilot open study demonstrated that 4-week treatment
with Lactobacillus Acidophilus eye-drops was effective in
reducing signs and symptoms of patients with mild to
moderate vernal keratoconjunctivitis in the active phase.
Lactobacilli eye-drops did not cause any side effects and
were well-tolerated by patients, as reported after systemic
administration.
All patients reported improvement of symptoms, except
one who dropped out of the study because his clinical
condition did not improve after 2 weeks of treatment. This
patient had the most severe form of VKC included in the
study, with the highest total symptom score, total sign score
and punctuate keratopathy scores at baseline.
Thus, total symptom score of the remaining patients was
significantly improved after 2 and 4 weeks of treatment,
demonstrating that Lactobacillus Acidophilus eye-drops can
improve symptoms in patients with VKC in the active
phase. A statistically significant improvement of clinical
signs was also observed after 1 month of treatment; in
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Graefes Arch Clin Exp Ophthalmol (2008) 246:435–441
439
Fig. 3 Patient characteristics at
slit-lamp examination. An
improvement of conjunctival
hyperemia (A, B; p<0.05),
Trantas dots (C, D; p>0.05) and
secretion (E, F; p>0.05) was
observed after 4 weeks of
Lactobacilli eye-drop treatment
particular, hyperemia and chemosis scores were significantly lower with respect to baseline.
Little is known regarding the precise mechanisms by
which lactobacilli may improve the clinical conditions of
allergic patients. The therapeutic effects of Lactobacillus
Acidophilus on VKC patients after 1 month of therapy
could be related to its antiinflammatory properties. Lactobacilli act by inducing antinflammatory cytokines such as
IL-10 e TGF-β, that play a crucial role in down-regulating
inflammatory cascades. Pessi et al. showed that serum IL10 concentrations were significantly elevated after giving
oral Lactobacillus rhamnosus GG at a daily dose of 2×
1010 CFU for 4 weeks to nine children affected by atopic
dermatitis [24]. Peripheral blood mononuclear cells, monocytes and lymphocytes from healthy donors, if stimulated
with lactobacilli and with polyclonal T cell stimulator
Fig. 4 Characteristics of the patient that underwent TLR4/ICAM-1
analysis. A significant down-regulation in ICAM-1 and TLR-4 mRNA
was observed in patients (Pt4 and Pt6) showing a reduction in total
symptoms score (TSyS) and total signs score (TSS) after 4 weeks of
treatment with Lactobacilli eye-drops. A slightly increase of both
ICAM-1 and TLR-4 mRNA was detected in the patient (Pt5) that did
not show an improvement of TSyS and TSS following Lactobacilli
treatment
phytohaemagglutinin (PHA), produce high levels of IL-10
and low levels of Th2-type cytokines [20]. In line with this
hypothesis, the reduction of conjunctival epithelial ICAM-1
expression observed in two patients showing clinical
improvement supports the hypothesis of an antiinflammatory effect of topical Lactobacillus on the ocular surface.
Another hypothesis is based on a direct effect of
Lactobacilli eye-drops in modulating the allergic reaction.
The concept of probiotics as possible means of antiallergic
therapy emerged from substantial but indirect evidence
linking low incidence rates of allergies in poor countries
with a certain composition of intestinal flora. These finding
are in line with the “hygiene hypothesis”, reporting that the
exposure to microbial products early in life could be
essential for the proper development of the immune system
[30]. The greatest microbial exposure throughout life, and
the newborn’s first major challenge, is the intestinal
microbiota. Bjorkstein et al. observed that Lactobacilli are
more commonly found in the intestinal microflora of
populations (eg. Estonian) with low incidence of allergic
diseases [6]. Besides, Kalliomaki et al. showed that children
who developed allergic diseases were less often colonized
by lactic acid producing bacteria, but had higher counts of
Clostridia when compared with healthy children [13].
There is evidence that probiotic microorganisms preferentially elicit T-helper 1 cells (Th1) and T-helper3/T
regulatory cells (Treg) that counterbalance the predominance of T-helper 2 (Th2) direct immune responses in
allergic disease. The ability of probiotic bacteria to induce
Th1 and Treg responses is based on the recognition of
bacterial cell components by cell receptors such as Toll-like
receptors (TLR), a family of glycoproteins expressed by
epithelial cells, dendritic cells, monocytes and mast cells/
basophils [8, 12]. TLRs are involved in the production of
inflammatory cytokines, cell stimulation and activation of
the specific immune response [12]. The expression of TLR4 has been correlated with the allergic phenotype. Dabbagh
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
440
et al. showed that TLR4-defective mice subjected to
sensitization and pulmonary challenge with a protein allergen
had reductions in airway inflammation by eosinophils,
allergen-specific IgE levels, and Th2 cytokine production,
compared with wild-type mice [7]. In addition, in vitro
studies observed that TLR-4 activation on mast cells
resulted in the induction of a subset of genes including
Th2 cytokines and chemokines [21, 22]. In a recent study,
VKC conjunctiva displayed upregulation of TLR-4, when
compared to healthy conjunctiva [4]. Thus, the reduction of
conjunctival expression of TLR-4 observed in patients after
4 weeks of therapy could be indirect evidence of the
immunomodulating effects of Lactobacillus Acidophilus.
Our preliminary data could suggest that topical treatment
with Lactobacillus Acidophilus may offer a safe and welltolerated support to standard antiallergic therapy for the
treatment of mild to moderate cases of vernal keratoconjunctivitis. However, it is not possible to exclude that the
beneficial effects referred by patients after 2 weeks of
treatment might be due to washing out of allergens from the
ocular surface rather than the effect of Lactobacillus
administration. The topical administration of Lactobacillus
Acidophilus may require at least 4 weeks of treatment to
exert a clinically significant effect. Additional double-blind
controlled clinical trials with a larger sample of patients are
needed to confirm the therapeutic effects of topical
Lactobacilli on VKC patients.
In conclusion, the administration of Lactobacilli eyedrops in VKC patients represents the first description of a
topical use of probiotic bacteria in humans.
References
1. Ait-Belgnaoui A, Han W, Lamine F, Eutamene H, Fioramonti J,
Bueno L, Theodorou V (2006) Lactobacillus farciminis treatment
suppresses stress induced visceral hypersensitivity: a possible
action through interaction with epithelial cell cytoskeleton
contraction. Gut 55:1090–1094
2. Bonini S, Bonini S, Lambiase A, Marchi S, Pasqualetti P, Zuccaro O,
Rama P, Magrini L, Juhas T, Bucci MG (2000) Vernal keratoconjunctivitis revisited: a case series of 195 patients with long-term
followup. Ophthalmology 107:1157–1163
3. Bonini S, Coassin M, Aronni S, Lambiase A (2004) Vernal
keratoconjunctivitis. Eye 18:345–351
4. Bonini S, Micera A, Iovieno A, Lambiase A, Bonini S (2005)
Expression of Toll-like receptors in healthy and allergic conjunctiva. Ophthalmology 112:1528; discussion 1548–1549
5. Boyle RJ, Tang ML (2006) The role of probiotics in the
management of allergic disease. Clin Exp Allergy 36:568–576
6. Bjorksten B, Sepp E, Julge K, Voor T, Mikelsaar M (2001)
Allergy development and the intestinal microflora during the first
year of life. J Allergy Clin Immunol 108:516–520
7. Dabbagh K, Dahl ME, Stepick-Biek P, Lewis DB (2002) Toll-like
receptor 4 is required for optimal development of Th2 immune
responses: role of dendritic cells. J Immunol 168:4524–4530
Graefes Arch Clin Exp Ophthalmol (2008) 246:435–441
8. Feleszko W, Jaworska J, Hamelmann E (2006) Toll-like receptorsnovel targets in allergic airway disease (probiotics, friends and
relatives). Eur J Pharmacol 533:308–318
9. Galdeano CM, Perdigon G (2006) The probiotic bacterium
Lactobacillus casei induces activation of the gut mucosal immune
system through innate immunity. Clin Vaccine Immunol 13:
219–226
10. Heyman M, Terpend K, Menard S (2005) Effects of specific lactic
acid bacteria on the intestinal permeability to macromolecules and
the inflammatory condition. Acta Paediatr Suppl 94:34–36
11. Joint FAO/WHO Working Group Report on Drafting Guidelines
for the Evaluation of Probiotics in Food London, Ontario, Canada,
April 30 and May 1, 2002
12. Kaisho T, Akira S (2006) Toll-like receptor function and
signaling. J Allergy Clin Immunol 117:979–987
13. Kalliomaki M, Kirjavainen P, Eerola E, Kero P, Salminen S,
Isolauri E (2001) Distinct patterns of neonatal gut microflora in
infants in whom atopy was and was not developing. J Allergy Clin
Immunol 107:129–134
14. Kalliomaki M, Salminen S, Arvilommi H, Kero P, Koskinen P,
Isolauri E (2001) Probiotics in primary prevention of atopic
disease: a randomised placebo- controlled trial. Lancet 357:1076–
1079
15. Kalliomaki M, Salminen S, Poussa T, Arvilommi H, Isolauri E
(2003) Probiotic and prevention of atopic disease: 4-year followup of a randomised placebo-controlled trial. Lancet 361:1869–
1871
16. Majamaa H, Isolauri E (1997) Probiotics: a novel approach in the
management of food allergy. J Allergy Clin Immunol 99:179–185
17. Malin M, Suomalainen H, Saxelin M, Isolauri E (1996) Promotion
of IgA immune response in patients with Crohn’s disease by oral
bacteriotherapy with Lactobacillus GG. Ann Nutr Metab 40:
137–145
18. Matricardi PM, Bjorksten B, Bonini S, Bousquet J, Djukanovic R,
Dreborg S, Gereda J, Malling HJ, Popov T, Raz E, Renz H, Wold
A; EAACI Task Force 7 (2003) Microbial products in allergy
prevention and therapy. Allergy 58:461–471
19. Miettinen M, Matikainen S, Vuopio-Varkila J, Pirhonen J, Varkila
K, Kurimoto M, Julkunen I (1998) Lactobacilli and streptococci
induce interleukin-12 (IL-12), IL-18, and gamma interferon
production in human peripheral blood mononuclear cells. Infect
Immun 66:6058–6062
20. Niers LE, Timmerman HM, Rijkers GT, van Bleek GM, van Uden
NO, Knol EF, Kapsenberg ML, Kimpen JL, Hoekstra MO (2005)
Identification of strong interleukin-10 inducing lactic acid bacteria
which down-regulate T helper type 2 cytokines. Clin Exp Allergy
35:1481–1489
21. Nigo YI, Yamashita M, Hirahara K, Shinnakasu R, Inami M,
Kimura M, Hasegawa A, Kohno Y, Nakayama T (2006)
Regulation of allergic airway inflammation through Toll-like
receptor 4-mediated modification of mast cell function. Proc Natl
Acad Sci USA 103:2286–2291
22. Okumura S, Kashiwakura J, Tomita H, Matsumoto K, Nakajima
T, Saito H, Okayama Y (2003) Identification of specific gene
expression profiles in human mast cells mediated by Toll-like
receptor 4 and FcepsilonRI. Blood 102:2547–2554
23. Peng GC, Hsu CH (2005) The efficacy and safety of heat-killed
Lactobacillus paracasei for treatment of perennial allergic rhinitis
induced by house-dust mite. Pediatr Allergy Immunol 16:433–438
24. Pessi T, Sutas Y, Hurme M, Isolauri E (2000) Interleukin-10
generation in atopic children following oral Lactobacillus rhamnosus
GG. Clin Exp Allergy 30:1804–1808
25. Pfaffl MW, Horgan GW, Dempfle L (2002) Relative expression
software tool (REST) for group-wise comparison and statistical
analysis of relative expression results in real-time PCR. Nucleic
Acids Res 30(9):e36
Tesi di dottorato in Immunologia Oculare, di Marta Sacchetti,
discussa presso l’Università Campus Bio-Medico di Roma in data 15/03/2010.
La disseminazione e la riproduzione di questo documento sono consentite per scopi di didattica e ricerca,
a condizione che ne venga citata la fonte.
Graefes Arch Clin Exp Ophthalmol (2008) 246:435–441
26. Pohjavuori E, Viljanen M, Korpela R, Kuitunen M, Tiittanen M,
Vaarala O, Savilahti E (2004) Lactobacillus GG effect in
increasing IFN-gamma production in infants with cow’s milk
allergy. J Allergy Clin Immunol 114:131–136
27. Rautava S, Kalliomaki M, Isolauri E (2005) New therapeutic
strategy for combating the increasing burden of allergic disease:
Probiotics-A Nutrition, Allergy, Mucosal Immunology and Intestinal Microbiota (NAMI) Research Group report. J Allergy Clin
Immunol 116:31–37
28. Rosenfeldt V, Benfeldt E, Nielsen SD, Michaelsen KF, Jeppesen
DL, Valerius NH, Paerregaard A (2003) Effect of probiotic
441
29.
30.
31.
32.
Lactobacillus strains in children with atopic dermatitis. J Allergy
Clin Immunol 111:389–395
Rozen S, Skaletsky H (2000) Primer3 on the WWW for general users
and for biologist programmers. Methods Mol Biol 132:365–386
Strachan DP (1989) Hay fever, hygiene, and household size. BMJ
299:1259–1260
Vanderhoof JA, Young RJ (2004) Current and potential uses of
probiotics. Ann Allergy Asthma Immunol 93:S33–S37
Wilcox RR (2007) New statistical procedures for the social
sciences: modern solution to basic problems. Lawrence Erlbaum
Associates, Hillsdale (NJ)