PAZIENTE IMMUNOTOLLERANTE E PORTATORE INATTIVO
Dr. Giuliano Alagna
StorianaturaleHBV
Replicazione
viarle
Immunità/risposta
dell’ospite
Liver
Failure
3%
INFEZIONE
ACUTA
INFEZIONE
CRONICA
5%
INACTIVE
CARRIER
Cirrosi
30%
Liver
Cancer
3%
MORTE
ALT
HBVDNA
HBeAg Anatomiapatologica
Immuno-tolerant
Normali
Elevate:>1milioneIU/ml
POS
Minimainfiammazioneofibrosi
HBeAg+
Immuneac:ve
Elevete
Elevate>20,000IU/ml
POS
Infiammazionemoderatasevera
ofibrosi
Inac:veCHB
Normali
Bassoononrilevabile
<2,000IU/ml
NEG
Minimanecroinfiammazionema
fibrosivariabile
HBeAg-immune
reac:va:on
Elevate
Elevate
>2,000IU/ml
NEG
Infiammazionedamoderataa
severaofibrosi
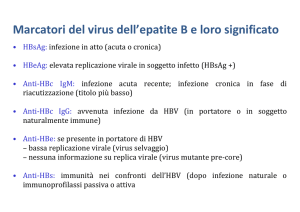
I fase: “immuno tolerant”: HBeAg+, alti livelli di replicazione virale (HBV DNA +++), livelli
normali o bassi di transaminasi lenta progressione della di fibrosi con scarsi segni di
infiammazione/necrosi. Questa fase è più frequente e lunga nei pazienti con infezione
perinatale
o contratta nei primi anni di vita. Basso tasso di perdita dell’ Hbe.
Ifase:“immunotolerant”:HBeAg+,alXlivellidireplicazionevirale(HBV
Fase
altamente contagiosa
DNA+++),livellinormaliobassiditransaminasilentaprogressionedella
difibrosiconscarsisegnidiinfiammazione/necrosi.Questafaseèpiù
IIfrequenteelunganeipazienXconinfezioneperinataleocontrabanei
fase: “immuno reactive phase”: HbeAg+, bassa replica virale con basso HBV DNA,
livelli aumentati o fluttuanti di transaminasi, segni di moderata o severa necrosi ed
primiannidivita.Bassotassodiperditadell’HBe.Fasealtamente
infiammazione
epatica e più rapida progressione verso la fibrosi rispetto alla fase I.
Piutipica
dell’ età adulta
contagiosa
III fase: “inactive HBV carrier state”: può seguire la sieroconversione da HBeAg+ ad
HbeAg negativo. E' caratterizzata da bassissimi valori di HBV DNA e livelli normali di
aminotransferasi. Questo stadio è associato ad una bassa probabilità di progressione
verso
la cirrosi e l'HCC….
IIIfase:“inacXveHBVcarrierstate”:puòseguirelasieroconversioneda
HBeAg+adanXHBeAg.E'caraberizzatadabassissimivaloridiHBVDNA
IV fase: “HBeAg-negative CHB” .: E' caratterizzata da periodiche riattivazioni con
elivellinormalidiaminotransferasi.E’necessariounfollowupminimo
fluttuazioni
sia dell'HBV DNA che delle transaminasi.
diunannomonitorizzandoleALT(<40UI/ML)el’HBVDNA(<2000U/
Vml).Questostadioèassociatoadunabassaprobabilitàdiprogressione
fase: “HBsAg negative phase” dopo la perdita dell'antigene di superficie bassi valori di
HBV
DNA possono persistere. La perdita dell' HBsAg è associata ad un miglioramento
versolacirrosiel'HCC
dell' outcome con una riduzione del rischio di progressione verso la cirrosi e verso l'HCC.
IN QUESTI PAZIENTI L'IMMUNOSOPPRESSIONE PUO' PORTARE ALLA RIATTIVAZIONE DELL'HBV
HBV carriers (HBsAg+):
attivo HBeAg o anti HBe+ HBV DNA>20000 UI/ml
inattivo HBeAg – Anti HBe+HBV DNA<2000 UI/ml
Occult HBV carriers (HBsAg-):
HBV DNA rilevabile come CCC DNA o HBV
DNA nel siero molto basso
IMMUNOTOLLERANTE
need for treatment. Of note, some persons will be in the
“gray zones,” meaning that their HBV DNA and ALT
evels do not fall into the same phase. Longitudinal
ollow-up of ALT and HBV DNA levels and/or assessment of liver histology can serve to clarify the phase of
nfection.
i. Immune-tolerant phase: In this highly replicative/
low inflammatory phase, HBV DNA levels are
elevated, ALT levels are normal (<19 U/L for
females and <30 U/L for males), and biopsies
are without signs of significant inflammation or
fibrosis. The duration of this phase is highly variable, but longest in those who are infected perinatally. With increasing age, there is an
increased likelihood of transitioning from
immune-tolerant to the HBeAg-positive immuneactive phase.
ii. HBeAg-positive immune-active phase: Elevated
ALT and HBV DNA levels in conjunction with
liver injury characterize this phase. Median age of
onset is 30 years among those infected at a young
age. The hallmark of transition from the HBeAgpositive immune-active to -inactive phases is
HBeAg seroconversion. The rate of spontaneous
Ø HBVDNAelevato
Ø ALTnormali(F<19UI/ml;
M<30UI/ml)
Ø Nofibrosi
Ø Fasepiùfrequentenelleprime
duedecadi
Guarigione
Formacronica
90-95%
5-10%
Bambinie
AdolescenX
40%
60%
NeonaX
10%
90%
AdulX
PerinatalvspostnatalacquisiXon(1)
Journal of Hepatology 48 (2008) 335–352
www.elsevier.com/locate/jhep
Review
Natural history of chronic hepatitis B: Special emphasis
on disease progression and prognostic factorsq
1,*
2
Giovanna Fattovich , Flavia Bortolotti , Francesco Donato
1
3
Department of Surgical and Gastroenterological Sciences, University of Verona, Piazzale L.A. Scuro, 10, Verona 37134, Italy
2
Fifth Medical Clinic, University of Padova, Padova, Italy
3
Institute of Hygiene, Epidemiology and Public Health, University of Brescia, Brescia, Italy
The natural history of chronic hepatitis B virus (HBV) infection and disease is complex and highly variable. We review
the natural history of chronic hepatitis B with emphasis on the rates of disease progression and factors influencing the
course of the liver disease. Chronic hepatitis B is characterized by an early replicative phase (HBeAg positive chronic hepatitis) and a late low or non-replication phase with HBeAg seroconversion and liver disease remission (inactive carrier
state). Most patients become inactive carriers after spontaneous HBeAg seroconversion with good prognosis, but progression to HBeAg negative chronic hepatitis due to HBV variants not expressing HBeAg occurs at a rate of 1–3 per 100 person years following HBeAg seroconversion. The incidence of cirrhosis appears to be about 2-fold higher in HBeAg negative
compared to HBeAg positive chronic hepatitis. In the cirrhotic patient the 5-year cumulative risk of developing hepatocellular carcinoma is 17% in East Asia and 10% in the Western Europe and the United States and the 5-year liver related
death rate is 15% in Europe and 14% in East Asia. There is a growing understanding of viral, host and environmental
factors influencing disease progression, which ultimately could improve the management of chronic hepatitis B.
! 2007 European Association for the Study of the Liver. Published by Elsevier B.V. All rights reserved.
Keywords: Chronic hepatitis B; Natural history; Prognostic factors
1. Introduction
Chronic infection with hepatitis B virus (HBV) currently affects about 400 million people, particularly in
developing countries, and it is estimated that worldwide
over 200,000 and 300,000 chronic HBV carriers die each
year from cirrhosis and hepatocellular carcinoma
(HCC), respectively [1,2]. The natural history of chronic
HBV infection and disease is variable and complex and
has still not been completely defined. A careful understanding of the clinical outcomes and factors affecting
Associate Editor: R.P. Perrillo
q
The authors declare that they do not have anything to disclose
regarding funding from industries or conflict of interest with respect to
this manuscript
*
Corresponding author. Tel./fax: +39 045 8124205.
E-mail address: [email protected] (G. Fattovich).
Perinatale
Ø InasiaibambiniinfebaXinepocaperinatale,presentanonormalivaloridiALT
conminimodannoepaXco(immunotolerantphase),essendoperaltro
asintomaXci
disease progression is important in the management of
chronic hepatitis B. This article reviews the natural history of chronic hepatitis B, with emphasis on summarizing the available data to estimate the rates of disease
progression according to the stage of the disease and
factors influencing its course.
2. Phases of chronic HBV infection
The likelihood of developing chronic HBV infection is
higher in individuals infected perinatally (90%) or during
childhood (20–30%), when the immune system is thought
to be immature, compared with immunocompetent subjects infected during adulthood (<1%). The phases of
chronic HBV infection described herein refer to patients
infected early in life. The natural course of chronic HBV
infection can be divided into four phases based on the
0168-8278/$32.00 ! 2007 European Association for the Study of the Liver. Published by Elsevier B.V. All rights reserved.
doi:10.1016/j.jhep.2007.11.011
Ø LapercentualedisieroconversioneadanXHBeèmoltovariabileaseconda
deglistudi(1,2)essendocompresatrail10edil75%a10/13annid’età
Ø QuandosihalasieroconversionedaHBeadanXHBe,siassisteall’incremento
delleALTedallariduzionedell’HBVDNA(puntonodale)
Ø Studilongitudinalidocumentanochelasieroconversioneconduceallostadio
diportatoreinamvo(clearancedell’HBsAg0.6%/anno);neibambiniincuisiha
unaseveranecroinfiammazionedurantelasieroconversioneanXHBesipuò
avereunarapidaprogressioneversolacirrosielosviluppodiHCC
1ChuCM,LiawYF.ChronichepaXXsBvirusinfecXonacquiredinchildhood:specialemphasisonprognosXcandtherapeuXcimplicaXonof
delayedHBeAgseroconversion.JViralHepat2007;14:147–152.
2MarxG,MarXnSR,ChicoineJF,AlvarezF.Long-termfollow-upofchronichepaXXsBvirusinfecXoninchildrenofdifferentethnicorigin.J
InfectDis2002;186:295–301.
Journal of Hepatology 48 (2008) 335–352
www.elsevier.com/locate/jhep
Review
Natural history of chronic hepatitis B: Special emphasis
on disease progression and prognostic factorsq
PerinatalvspostnatalacquisiXon(2)
Giovanna Fattovich1,*, Flavia Bortolotti2, Francesco Donato3
1
Department of Surgical and Gastroenterological Sciences, University of Verona, Piazzale L.A. Scuro, 10, Verona 37134, Italy
2
Fifth Medical Clinic, University of Padova, Padova, Italy
3
Institute of Hygiene, Epidemiology and Public Health, University of Brescia, Brescia, Italy
The natural history of chronic hepatitis B virus (HBV) infection and disease is complex and highly variable. We review
the natural history of chronic hepatitis B with emphasis on the rates of disease progression and factors influencing the
course of the liver disease. Chronic hepatitis B is characterized by an early replicative phase (HBeAg positive chronic hepatitis) and a late low or non-replication phase with HBeAg seroconversion and liver disease remission (inactive carrier
state). Most patients become inactive carriers after spontaneous HBeAg seroconversion with good prognosis, but progression to HBeAg negative chronic hepatitis due to HBV variants not expressing HBeAg occurs at a rate of 1–3 per 100 person years following HBeAg seroconversion. The incidence of cirrhosis appears to be about 2-fold higher in HBeAg negative
compared to HBeAg positive chronic hepatitis. In the cirrhotic patient the 5-year cumulative risk of developing hepatocellular carcinoma is 17% in East Asia and 10% in the Western Europe and the United States and the 5-year liver related
death rate is 15% in Europe and 14% in East Asia. There is a growing understanding of viral, host and environmental
factors influencing disease progression, which ultimately could improve the management of chronic hepatitis B.
! 2007 European Association for the Study of the Liver. Published by Elsevier B.V. All rights reserved.
Keywords: Chronic hepatitis B; Natural history; Prognostic factors
1. Introduction
Chronic infection with hepatitis B virus (HBV) currently affects about 400 million people, particularly in
developing countries, and it is estimated that worldwide
over 200,000 and 300,000 chronic HBV carriers die each
year from cirrhosis and hepatocellular carcinoma
(HCC), respectively [1,2]. The natural history of chronic
HBV infection and disease is variable and complex and
has still not been completely defined. A careful understanding of the clinical outcomes and factors affecting
Associate Editor: R.P. Perrillo
q
The authors declare that they do not have anything to disclose
regarding funding from industries or conflict of interest with respect to
this manuscript
*
Corresponding author. Tel./fax: +39 045 8124205.
E-mail address: [email protected] (G. Fattovich).
Postnatal
disease progression is important in the management of
chronic hepatitis B. This article reviews the natural history of chronic hepatitis B, with emphasis on summarizing the available data to estimate the rates of disease
progression according to the stage of the disease and
factors influencing its course.
Ø Lamaggiorpartedeibambiniconinfezioneacquisitaarrivaall’osservazionein
unafasediincrementodelleALTconmalamaamva
2. Phases of chronic HBV infection
The likelihood of developing chronic HBV infection is
higher in individuals infected perinatally (90%) or during
childhood (20–30%), when the immune system is thought
to be immature, compared with immunocompetent subjects infected during adulthood (<1%). The phases of
chronic HBV infection described herein refer to patients
infected early in life. The natural course of chronic HBV
infection can be divided into four phases based on the
0168-8278/$32.00 ! 2007 European Association for the Study of the Liver. Published by Elsevier B.V. All rights reserved.
doi:10.1016/j.jhep.2007.11.011
Ø SieroconversioneadanXHBetrail14-16%/annoduranteiprimi10anni
Ø InunostudiolongitudinaleItaliano(*)il95%dibambiniandaXincontroa
sieroconversioneHBesonodiventaXportatoriinamviprimadelraggiungimento
dell’etàadulta
*BortolomF,GuidoM,BartolacciS,CadrobbiP,CrivellaroC,NoventaF,etal.ChronichepaXXsBinchildrenavereanXgen
seroclearance:finalreportofa29yearlongitudinalstudy.Hepatology2006;43:556–562.
Table 2. Among 17 studies of inter
47
Ageand
overRationale
40 years is associa
years.
Evidence
tolerant
adults,
only
two examined
Recommendations
Quality/Certainly
of
Evidence:
Moderate
The
evidence
profile
is summ
lihood
of
significant
histological
Technical Remark
than
ULNs,
whereas
most
used
AL
Strength of Recommendation: Strong
Table
2.
Among
17
studies
of
inte
positivefor
persons
with All
normal
ALT
The AASLD status
recommends
against
inclusion.
were
RCTsle
1.2A.Immune-tolerant
should be
definedantiviral
by ALT ULNs
tolerant adults,
only two
examined
Technical
Remark
thanofULNs,
whereas
24-48 weeks
formost
IFN orused
48 wA
therapy
adults with
CHB.!19 U/L tion
levelsforutilizing
!30immune-tolerant
U/L for men and
ULNs
forand
inclusion.
All werefollow
RCT
1. Immune-tolerant
status
should
defined
by ALT Evidence
12
months
of Rationale
post-treatment
for women as ULNs
rather
thanbe local
laboratory
of 24-48 weeks for IFN or 48
Quality/Certainly
Evidence:
Moderate
levels utilizing of
!30
U/L for
men and !19 U/L tion
The
evidence
profile is summa
HBeAg
loss and
seroconversion
as t
ULNs.
12
months
of
post-treatment
follo
for
women
as
ULNs
rather
than
local
laboratory
Strength of Recommendation: Strong
Table
2. Among
interv
whereas
onlyand
two17seroconversion
studies ofevaluate
HBeAg
loss
as
ULNs.
2B. The AASLD suggests that ALT levels be tested tolerant
whereascomparing
only only
twoantiviral
studies
evaluat
studies
therapy
adults,
two
examined
2B.
The
AASLD
suggests
that
ALT
levels
be
tested
at least Remark
every 6 months for adults with immune- ment
studies comparing antiviral therap
Technical
were thewhereas
primarymost
studies
ULNs,
usedinform
AL
at least every 6 months for adults with immune- than
ment
were
the
primary
studies
info
tolerant
CHB
to
monitor
for
potential
transition
to
CHB to monitor for potential transition to ULNs
dation.
The
remaining
1212RCTs
studies
for
inclusion.
All
were
dation.
The
remaining
studi
1.tolerant
Immune-tolerant
status
should
be
defined
by
ALT
immune-active
or
-inactive
CHB.
immune-active or -inactive CHB.
comparisons
antiviral
comparisons
ofdifferent
different
antiviral
tion
of 24-48 ofweeks
for IFN
or 48the
wth
levels
utilizing
!30
U/L
for
men
and
!19
U/L
Comparedtotountreated/placebo
untreated/placebo
Quality/Certainly
Very low
low
Compared
Quality/Certainly of
of Evidence:
Evidence: Very
12
months
of
post-treatment
follow
for women
as ULNs rather than
local laboratory ralral therapy
therapy resulted in a signifi
Strength
of Recommendation:
Conditional
resulted
in a95%
significa
Strength of Recommendation: Conditional
HBeAg
loss
(RR,
2.69;
HBeAg
loss
and
seroconversion
asCI:th
ULNs.
2C.
The AASLD suggests antiviral therapy in the HBeAg
loss (RR,
(RR, 2.22;
2.69;95%
95%CI:
CI:11
conversion
onlyby(RR,
two
studies
evaluate
2C.group
The AASLD
antiviral
in the whereas
select
of adultssuggests
>40 years
of agetherapy
with normal
of
results
treatment
type
conversion
2.22;
95%
CI:(IFN
1.2
2B.
The
AASLD
suggests
that
ALT
levels
be
tested
ALT
and
elevated
HBV
DNA
("1,000,000
IU/mL)
select group of adults >40 years of age with normal studies
comparing
therapy
dine)
yielded
RR antiviral
that type
included
of
results
by
treatment
(IFN1a
and
liver
biopsy
showing
significant
necroinflammaatALT
leastandevery
6
months
for
adults
with
immuneferentwere
from
controls).
T
elevated HBV DNA ("1,000,000 IU/mL) ment
theuntreated
primary
studies
inform
tion or fibrosis.
dine)
yielded
RR
that
included
1
(
low-to-moderate
quality
and
the
tolerant
CHB
to
monitor
for
potential
transition
to
and liver biopsy showing significant necroinflamma- dation.
Thebaseline
remaining
12
studies
ferent
from
untreated
Th
sons with
ALTcontrols).
values
less
Quality/Certainly of Evidence: Very low
immune-active
or -inactive CHB.
tion
or fibrosis.
low to low quality.
comparisons
of different
Strength
of Recommendation: Conditional
low-to-moderate
qualityantiviral
and thetheR
There are no studies demons
Compared
to untreated/placebo
sons
with baseline
ALT values less t
Quality/Certainly
of
Evidence:
Very
low
Quality/Certainly
of
Evidence:
Very
low
therapy is beneficial in reducing ra
Technical Remark
toliver-related
low quality.
rallow
resulted
in ina persons
significa
StrengthofofRecommendation:
Recommendation:Conditional
Conditional
Strength
andtherapy
death
1. Moderate-to-severe necroinflammation or fibrosis
CHB.
Finite
duration
Thereloss
are(RR,
notreatment
studies95%
demonst
HBeAg
2.69;
CI: 1
therapy for adults with immune-tolerant CHB.
INACTIVECARRIER
q Qualisonoicriterioggemviperindividuarlo?
q Qualeèilrischiodiprogressionedimalamae
sviluppoHCC?
q Rischiodiriamvazione
q QualeXpodifollowupbisognaapplicareinquesX
pazienX?
Ø L’interazionetravirusedimmunitàdell’ospitespiegaladinamicitàdelle
fasidimalama
Ø Lacompressionedellasuddebadinamicitàdellastorianaturalehaindobo
adunavariazionedellaterminologiauXlizzata
1960
Healtycarrier
AsyntomaXcHBsAgcarrier
InacXveHBsAgcarrier
InacXvecarrierstate
2016
LowreplicaXvechronicHBVInfecXon(APASL)
Qualisonoicriterioggemviperindividuarlo?
ü ALT
ü LivelliHBVDNA
ü IstologiaepaXca?
ü ALT
Clinical Practice Guidelines
EASL Clinical Practice Guidelines: Management of chronic
hepatitis B virus infection
European Association for the Study of the Liver⇑
Introduction
Our understanding of the natural history of hepatitis B virus
(HBV) infection and the potential for therapy of the resultant disease is continuously improving. New data have become available
since the previous EASL Clinical Practice Guidelines (CPGs) prepared in 2008 and published in early 2009 [1]. The objective of
this manuscript is to update the recommendations for the optimal management of chronic HBV infection. The CPGs do not fully
address prevention including vaccination. In addition, despite the
increasing knowledge, areas of uncertainty still exist and therefore clinicians, patients, and public health authorities must continue to make choices on the basis of the evolving evidence.
been increasing over the last decade as a result of aging of the
HBV-infected population and predominance of specific HBV
genotypes and represents the majority of cases in many areas,
including Europe [4,9,10]. Morbidity and mortality in CHB are
linked to persistence of viral replication and evolution to cirrhosis
and/or hepatocellular carcinoma (HCC). Longitudinal studies of
untreated patients with CHB indicate that, after diagnosis, the
5-year cumulative incidence of developing cirrhosis ranges
from 8% to 20%. The 5-year cumulative incidence of hepatic
decompensation is approximately 20% for untreated patients
with compensated cirrhosis [2–4,11–13]. Untreated patients with
decompensated cirrhosis have a poor prognosis with a 14–35%
probability of survival at 5 years [2–4,12]. The worldwide incidence of HCC has increased, mostly due to persistent HBV and/
or HCV infections; presently it constitutes the fifth most common
cancer, representing around 5% of all cancers. The annual incidence of HBV-related HCC in patients with CHB is high, ranging
from 2% to 5% when cirrhosis is established [13]. However, the
incidence of HBV related HCC appears to vary geographically
and correlates with the underlying stage of liver disease and possibly exposure to environmental carcinogens such as aflatoxin.
Population movements and migration are currently changing
the prevalence and incidence of the disease in several low endemic countries in Europe and elsewhere. Substantial healthcare
resources will be required for control of the worldwide burden
of disease.
Aminimumfollow-upof1yearwithalanineaminotransferase(ALT)levelsatleast
every3–4monthsandserumHBVDNAlevelsisrequiredbeforeclassifyingapaXent
asinacXveHBVcarrier.ALTlevelsshouldremainpersistentlywithinthenor-mal
Context
rangeaccordingtotradiXonalcut-offvalues(approximately40IU/ml)
Epidemiology and public health burden
Approximately one third of the world’s population has serological
evidence of past or present infection with HBV and 350–400 million people are chronic HBV surface antigen (HBsAg) carriers. The
spectrum of disease and natural history of chronic HBV infection
are diverse and variable, ranging from an inactive carrier state to
progressive chronic hepatitis B (CHB), which may evolve to cirrhosis and hepatocellular carcinoma (HCC) [2–4]. HBV-related
end stage liver disease or HCC are responsible for over 0.5–1 million deaths per year and currently represent 5–10% of cases of
Natural history
ü ALT
Digestive and Liver Disease 43S (2011) S8–S14
Contents lists available at ScienceDirect
Digestive and Liver Disease
journal homepage: www.elsevier.com/locate/dld
Ø on
MolXdeglistudicondomperindividuare
Natural history of chronic HBV infection: special emphasis
the
prognostic implications of the inactive carrier state versus chroniceventualirischilegaXallostatodiportatore
hepatitis
inamvosonostaXviziaXdalfabocheèstata
a, 1
b,1
a
b
Erica Villa *, Giovanna Fattovich , Antonella Mauro , Michela Pasino considerataun’unicamisurazionedelleALT
a Gastroenterology and Liver Clinic, Azienda Ospedaliero-Universitaria, University of Modena and Reggio Emilia, Modena, Italy
b Gastroenterology Clinic, Department of Medicine, Azienda Ospedaliero-Universitaria, University of Verona, Verona, Italy
Abstract
Ø Glistudicondomconabentomonitoraggiodelle
ALThannoevidenziatocomepiùdell’85%dei
pazienXritenuXcarrier,loeranoeffemvamente
inaccordoconl’esameistologico
The evaluation of the natural history of chronic hepatitis B virus (HBV) infection requires the precise definition of the various clinical
conditions that can be encountered (i.e. inactive carrier state or subject with liver disease activity). This can be achieved by repeat monitoring
of ALT, serum HBV-DNA levels (over a period of at least 1 year, according to international guidelines) and/or evaluation of HBsAg titre.
Liver biopsy may offer additional information although it is not mandatory.
Overall, the natural history of the true inactive carrier is benign: reactivation of hepatitis, especially in Western countries, is rare and is
usually due to co-factors (like alcohol or drugs); spontaneous HBsAg loss is frequent (around 1% per year) and HCC development rare. On
the other hand, in patients with chronic hepatitis B or cirrhosis, the risk of reactivation, of HCC development and of liver-related mortality is
much higher, especially in Eastern countries, and should therefore lead to antiviral therapy.
© 2010 Editrice Gastroenterologica Italiana S.r.l. Published by Elsevier Ltd. All rights reserved.
Keywords: Chronic hepatitis; Hepatitis B virus; Inactive carrier state; Prognosis
During the last few years there has been a substantial mod-
carrier”. Although several studies on the natural history of
implications. Indeed, several conditions have to be fulfilled for
of an “inactive carrier state” rather than an “inactive carrier”,
NaturalhistoryofchronicHBVcarriersinNorthernItaly:morbidityandmortalityaver30years.MannoM,Camma`C,SchepisF,etal.
ification of the nomenclature regarding Hepatitis B surface patients with chronic HBV infection have been published,
Gastroenterology2004;127:756−63.
Antigen (HBsAg) carriers with no or scarce evidence of active a comprehensive analysis is hampered by the different
DeFranchisR,MeucciG,VecchiM,etal.ThenaturalhistoryofasymptomaXchepaXXsBsurfaceanXgencarriers.AnnInternMed1993
liver disease. The definition of “healthy carrier” used in the study designs (case–control, cross-sectional, longitudinal) and
1960s has been changed to “asymptomatic HBsAg carrier”, the heterogeneity of the patient populations relative to the
VilleneuveJP,DesrochersM,Infante-RivardC,etal.Along-termfollow-upstudyofasymptomaXchepaXXsBsurfaceanXgen-posiXvecarriersin
and recently this has been further modified to “inactive clinical setting (inactive carrier, asymptomatic carrier, chronic
Montreal.Gastroenterology1994
HBsAg carrier”. This progressive modification is more than hepatitis). Available data have called into question the concept
a mere semantic process, as it has substantial clinical of inactive carrier, and proposals have been made to speak
Long-termoutcomeofhepaXXsBeanXgen-negaXvehepaXXsB
surfaceanXgencarriersinrelaXontochangesofalanine
aminotransferaselevelsoverXme
4376HBsAg+,HBeAg-“carrier”
ALTvalutateogni3mesi/annoper3anni
1720pazienX(46.8%)neisuccessivitrediciannihannoavutounincrementodelle
transaminasi
Transaminasipersistentementenormalicorrelanoconun’eccellenteprognosi
Unincremento2ULNduranteilFUèassociatoadun’aumentatamorbiditàemortalità
Unincremento2ULNpuòessereconsideratoilcut-offdecisionaleriguardolaterapia
TaiDietal.Hepatology.2009Jun;49(6):1859-67
ü ALT
Clinical Practice Guidelines
EASL Clinical Practice Guidelines: Management of chronic
hepatitis B virus infection
European Association for the Study of the Liver⇑
Introduction
Our understanding of the natural history of hepatitis B virus
(HBV) infection and the potential for therapy of the resultant disease is continuously improving. New data have become available
since the previous EASL Clinical Practice Guidelines (CPGs) prepared in 2008 and published in early 2009 [1]. The objective of
this manuscript is to update the recommendations for the optimal management of chronic HBV infection. The CPGs do not fully
address prevention including vaccination. In addition, despite the
increasing knowledge, areas of uncertainty still exist and therefore clinicians, patients, and public health authorities must continue to make choices on the basis of the evolving evidence.
been increasing over the last decade as a result of aging of the
HBV-infected population and predominance of specific HBV
genotypes and represents the majority of cases in many areas,
including Europe [4,9,10]. Morbidity and mortality in CHB are
linked to persistence of viral replication and evolution to cirrhosis
and/or hepatocellular carcinoma (HCC). Longitudinal studies of
untreated patients with CHB indicate that, after diagnosis, the
5-year cumulative incidence of developing cirrhosis ranges
from 8% to 20%. The 5-year cumulative incidence of hepatic
decompensation is approximately 20% for untreated patients
with compensated cirrhosis [2–4,11–13]. Untreated patients with
decompensated cirrhosis have a poor prognosis with a 14–35%
probability of survival at 5 years [2–4,12]. The worldwide incidence of HCC has increased, mostly due to persistent HBV and/
or HCV infections; presently it constitutes the fifth most common
cancer, representing around 5% of all cancers. The annual incidence of HBV-related HCC in patients with CHB is high, ranging
from 2% to 5% when cirrhosis is established [13]. However, the
incidence of HBV related HCC appears to vary geographically
and correlates with the underlying stage of liver disease and possibly exposure to environmental carcinogens such as aflatoxin.
Population movements and migration are currently changing
the prevalence and incidence of the disease in several low endemic countries in Europe and elsewhere. Substantial healthcare
resources will be required for control of the worldwide burden
of disease.
Aminimumfollow-upof1yearwithalanineaminotransferase(ALT)levels
atleastevery3–4monthsandserumHBVDNAlevelsisrequiredbefore
classifyingapa:entasinac:veHBVcarrier.
Context
Epidemiology and public health burden
Approximately one third of the world’s population has serological
evidence of past or present infection with HBV and 350–400 million people are chronic HBV surface antigen (HBsAg) carriers. The
spectrum of disease and natural history of chronic HBV infection
are diverse and variable, ranging from an inactive carrier state to
progressive chronic hepatitis B (CHB), which may evolve to cirrhosis and hepatocellular carcinoma (HCC) [2–4]. HBV-related
end stage liver disease or HCC are responsible for over 0.5–1 million deaths per year and currently represent 5–10% of cases of
liver transplantation [5–8]. Host and viral factors, as well as coinfection with other viruses, in particular hepatitis C virus (HCV),
hepatitis D virus (HDV), or human immunodeficiency virus
BruneboMR,Hepatology1989;CPG,EASL2012
(HIV) together with other co-morbidities including alcohol abuse
Liuj1Hepatology.2016
and obesity, can affect the natural course of HBV infection as well
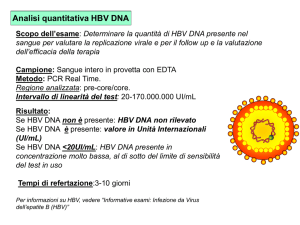
Ø HBVDNA<2000UI/mL
Ø HBsAg<1000UI/mL
Natural history
ü HBVDNA
Chronic HBV infection is a dynamic process. The natural history
of chronic HBV infection can be schematically divided into five
phases, which are not necessarily sequential.
Digestive and Liver Disease 43S (2011) S8–S14
Contents lists available at ScienceDirect
Digestive and Liver Disease
journal homepage: www.elsevier.com/locate/dld
ü ISTOLOGIA
Natural history of chronic HBV infection: special emphasis on the
prognostic implications of the inactive carrier state versus chronic hepatitis
Erica Villaa, 1*, Giovanna Fattovichb,1, Antonella Mauroa , Michela Pasinob
a Gastroenterology and Liver Clinic, Azienda Ospedaliero-Universitaria, University of Modena and Reggio Emilia, Modena, Italy
b Gastroenterology Clinic, Department of Medicine, Azienda Ospedaliero-Universitaria, University of Verona, Verona, Italy
Abstract
The evaluation of the natural history of chronic hepatitis B virus (HBV) infection requires the precise definition of the various clinical
conditions that can be encountered (i.e. inactive carrier state or subject with liver disease activity). This can be achieved by repeat monitoring
of ALT, serum HBV-DNA levels (over a period of at least 1 year, according to international guidelines) and/or evaluation of HBsAg titre.
Liver biopsy may offer additional information although it is not mandatory.
Overall, the natural history of the true inactive carrier is benign: reactivation of hepatitis, especially in Western countries, is rare and is
usually due to co-factors (like alcohol or drugs); spontaneous HBsAg loss is frequent (around 1% per year) and HCC development rare. On
the other hand, in patients with chronic hepatitis B or cirrhosis, the risk of reactivation, of HCC development and of liver-related mortality is
much higher, especially in Eastern countries, and should therefore lead to antiviral therapy.
© 2010 Editrice Gastroenterologica Italiana S.r.l. Published by Elsevier Ltd. All rights reserved.
Ø Pochistudi*hannoriportatodaXriguardol’istologianeiportatoriinamvi;
difabosoloil3%presenterebbeun’epaXtecronicamoderata
Keywords: Chronic hepatitis; Hepatitis B virus; Inactive carrier state; Prognosis
During the last few years there has been a substantial modification of the nomenclature regarding Hepatitis B surface
Antigen (HBsAg) carriers with no or scarce evidence of active
liver disease. The definition of “healthy carrier” used in the
1960s has been changed to “asymptomatic HBsAg carrier”,
and recently this has been further modified to “inactive
HBsAg carrier”. This progressive modification is more than
a mere semantic process, as it has substantial clinical
implications. Indeed, several conditions have to be fulfilled for
a subject to be included in this subgroup of inactive hepatitis B
virus (HBV) carriers, namely: hepatitis B e antigen (HBeAg)
negative, antibody to HBeAg (anti-HBe) positive, persistently
normal alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels, serum HBV-DNA<2000IU/ml,
and, whenever available, liver histology with low grade
inflammation (less than 4) [1].
The evidence, however, for these stringent criteria is
supported by limited data as there are only few longitudinal
cohort studies with a clear-cut definition of “inactive HBsAg
*Corresponding author. Prof. Erica Villa. Gastroenterology and Liver
Clinic, Azienda Ospedaliero-Universitaria, University of Modena and Reggio
Emilia, Modena, Via del Pozzo 71, 41124 Italy.
Tel.: +390594225308; fax: +390594224363.
E-mail address: [email protected] (E. Villa).
1
carrier”. Although several studies on the natural history of
patients with chronic HBV infection have been published,
a comprehensive analysis is hampered by the different
study designs (case–control, cross-sectional, longitudinal) and
the heterogeneity of the patient populations relative to the
clinical setting (inactive carrier, asymptomatic carrier, chronic
hepatitis). Available data have called into question the concept
of inactive carrier, and proposals have been made to speak
of an “inactive carrier state” rather than an “inactive carrier”,
implying a possible reversion of the condition [2]. A careful
understanding of the clinical features and outcome of the
inactive HBsAg carrier is relevant for the management of
chronic HBV infection. For this purpose this article will
review the literature regarding liver function, viral replication,
liver histology and clinical course in an attempt to better
define the features of the inactive HBsAg carrier state and to
evaluate differences in prognosis according to clinical settings
(inactive carrier state or chronic hepatitis).
1. Liver function
Ø L’associazionedelsolodosaggiodelletransaminasiedell’HBVDNApuò
portareadunaperditadicircail10%dimalameepaXcheistologicamente
significaXve
A major bias influencing the results of studies on patients
with chronic HBV infection is the cross-sectional, instead
These authors contributed equally.
© 2010 Editrice Gastroenterologica Italiana S.r.l. Published by Elsevier Ltd. All rights reserved.
DeFranchisR,MeucciG,VecchiM,etal.ThenaturalhistoryofasymptomaXchepaXXsBsurfaceanXgencarriers.AnnInternMed
1993;118:191−4.
VelascoM,González-CerónM,delaFuenteC,etal.ClinicalandpathologicalstudyofasymptomaXcHBsAgcarriersinChile.Gut1978
MarXnot-PeignouxM,BoyerN,ColombatM,etal.SerumhepaXXsBvirusDNAlevelsandliverhistologyininacXveHBsAgcarriers.JHepatol
2002;36:543−6.
Liver International ISSN 1478-3223
REVIEW ARTICLE
The prognosis and management of inactive HBV carriers
! 2, Glenda Grossi1 and Pietro Lampertico1
Federica Invernizzi1, Mauro Vigano
1 ‘A. M. and A. Migliavacca’ Center for Liver Disease, Division of Gastroenterology and Hepatology Fondazione IRCCS Ca’ Granda Ospedale
Maggiore Policlinico, Universit!
a di Milano, Milano, Italy
2 Hepatology Unit, Ospedale San Giuseppe, Universit!
a degli Studi di Milano, Milano, Italy
DOI: 10.1111/liv.13006
Abstract
Patients with chronic hepatitis B virus (HBV) infection lacking the serum hepatitis B e antigen (HBeAg) and with antibodies
against HBeAg (anti-HBe), are the prevalent subgroup of HBV carriers worldwide. The prognosis of these patients is different
Ø UXlizzodellatransientelastography(TE)perdiscriminareICdaHBsAgnegaXveCHB
from inactive carriers (ICs), who are characterized by persistently normal serum alanine aminotransferase (ALT) and low
(<2000 IU/ml) serum HBV DNA levels, a serological profile that may also be intermittently observed in patients with HBeAgnegative chronic hepatitis. This is why a confirmed diagnosis of IC requires quarterly ALT and HBV DNA measurements for at
least 1 year, while a single-point detection of combined HBsAg <1000 IU/ml and HBV DNA <2000 IU/ml has a robust predictive value for the diagnosis of IC. Characteristically, ICs have minimal or no histological lesions of the liver corresponding to
liver stiffness values on Fibroscan of <5 kPa. Antiviral treatment is not indicated in ICs since the prognosis for the progression
of liver disease is favourable if there are no cofactors of liver damage such as alcohol abuse, excess weight or co-infection with
the hepatitis C virus or delta virus. Moreover, spontaneous HBsAg loss frequently occurs (1–1.9% per year) in these patients
while the development of hepatocellular carcinoma (HCC) is rare, at least in Caucasian patients. However, an emerging issue
reinforcing the need for clinical surveillance of ICs is the risk of HBV reactivation in patients who undergo immunosuppressive
therapy without receiving appropriate antiviral prophylaxis. After diagnosis, management of ICs includes monitoring of ALT
and HBV DNA every 12 months with periodic measurement of serum HBsAg levels to identify viral clearance.
Ø NegliIcslasXffnessmediacalcolataneglistudièdi5KPa(limitesuperioredi7.9Kpa)
Ø L’evidenzadipiùelevaXdisXffnessinpazienteconsoppressioneviraleenormaliAlt
puòindicareundannoepaXcosecondarioadaltracausa,suggerendounpiùabento
monitoraggiool’esecuzionediunabiopsiaepaXca
Keywords
antiviral treatment – HCC – hepatitis B virus – inactive carriers – natural history – prophylaxis
Olivieri
from patients with HBeAg-negative
2008 4.3+/-1KPa
hepatitis because of the different
Maimone
2009 4.83+/-1KPa
Castera
2011 4.8+/-2KPa
An estimated 340 million individuals are chronically
infected with the hepatitis B virus (HBV) with a risk of
developing end-stage liver complications (1–3). Patients
with antibodies against the hepatitis B e antigen (antiHBe) are the largest subgroup of HBV carriers worldwide, and characterized by a broad spectrum of clinical
conditions ranging from the inactive carrier (ICs) state
to chronic active hepatitis progressing to liver complications such as cirrhosis, liver failure and hepatocellular
carcinoma (HCC) (2–4). ICs must be distinguished
chronic active
prognosis and
management of these groups, with a substantial risk of
cirrhosis, clinical decompensation and HCC in the latter
(4, 5). The distinctive virological feature of patients with
chronic active HBV is infection with HBV variants that
cannot produce HBeAg because of the presence of precore or basal core promoter mutations. The livers of
these patients show persistent necroinflammation characterized by fluctuations of both viral replication and
QualeèilrischiodiprogressionedimalamaesviluppoHCC?
May 2010
LONG-TERM HEALTH OUTCOMES OF INACTIVE HBV CARR
Natural history of chronic hepatitis B
C-J Chen and H-I Yang
89 293 individuals invited
to participate in 1991–1992
23 820 enrolled in the
cohort
4155 HBsAg (+)
19 665 HBsAg (–)
3653 HBV DNA available
and anti-HCV (–)
565 HBeAg (+)
3088 HBeAg (–)
2780 HBV DNA detectable
873 HBV DNA undetectable
1520 genotype B
801 genotype C
1619 HBV DNA
84 genotype B+C
104 copies/mL
543 precore 1896 wild-type
705 BCP 1762/2764 wild-type
Supplementary
Figure 1. Flow
of participants
750 precore 1896 mutant
578chart
BCP 1762/2764
mutant in the inactive
hepatitis B virus carrier and control subcohorts. ALT, alanine aminotransferase; HBsAg, hepatitis B surface antigen; HCV, hepatitis C virus.
30
1932inacXvecarriers(HBsAg+,
HBVDNA<10,000copie/mL;
ALT<45)
Followupsemestralecon
ecografiaaddominaleedesami
ematochimici
10 000–99 999,
Figure 1 Flow of the Risk Evaluation of Viral
Load Elevation and Associated Liver Disease/
Cancer-Hepatitis B Virus (REVEAL-HBV)
study participants.
REVEALHBV
100 000–999 999,
1 000 000–99 999 999,
Ø IncidenzaHCCinacXve
carriers:64/100000
Ø Incidenzacasicontrollo
15/100000
Ø NondifferenzasignificaXva
interminidiincidenzatrai
portatoriinamviconvalori
diHBVDNAnonrilevabili
rispeboaipazienXcon
HBV<2000UI/ml
CLINICAL–LIVER,
Figure 1. Cumulative hazards of progression to hepatocellular carcinoma in the inactive hepatitis B virus
(HBV) carrier and control subcohorts.
95% CI: 0.6!4.5). For inactive HBV carriers with undetectable baseline serum HBV DNA, an alcohol drinking
A total of 1775 (91.9%) inactive HBV carriers, including
92.2% (772 of 837) and 91.6% (1003 of 1095) of those
FATTORIDIRISCHIOHCCNEIPORTATORIINATTIVI
Table 2. Multivariate-Adjusted Hazard Ratios (95% Confidence Intervals) of the Risk Predictors for Newly Developed
Hepatocellular Carcinoma Included in the Cox Regression Models
All participants (n " 20,069)
Variable
Cohort
Control
Inactive HBV carrier
Undetectable HBV DNA
HBV DNA 300!10,000 copies/mL
Age (increment by every decade)
Male sex (vs female)
ALT (high-normal vs low-normal)
Alcohol drinking habit (ever vs never)
Cigarette smoking habit (ever vs never)
Hazard ratio
(95% CI)
1.0
(referent)
3.5a
5.7a
2.7
1.3
2.2
2.4
1.7
(1.5!8.3)
(2.8!11.5)
(1.9!3.8)
(0.6!2.9)
(1.2!4.1)
(1.3!4.7)
(0.8!3.5)
Inactive HBV carriers (n " 1932)
P value
Hazard ratio
(95% CI)
P value
1.0
1.6
2.6
2.9
0.5
5.0
0.5
(referent)
(0.6!4.5)
(1.4!4.6)
(0.7!11.8)
(0.1!2.3)
(1.6!15.6)
(0.2!1.6)
.362
.002
.133
.374
.005
.245
—
.005
#.001
#.001
.545
.011
.008
.151
ALT, alanine aminotransferase; CI, confidence interval; HBV, hepatitis B virus.
" .349 for the difference between serum HBV DNA 300-10,000 copies/mL vs undetectable.
aP
CarriersofInac:veHepa::sBVirusAreS:llatRiskforHepatocellularCarcinomaandLiver-RelatedDeath.Jin-deChenetal.
GASTROENTEROLOGY2010;138:1747–1754
liver) car-
CLINICAL–LIVER,
PANCREAS, AND
BILIARY TRACT
Liverrelatedmortality
44/100000vs21/100000
FATTORIDIRISCHIODI“LIVERRELATEDDEATH”NEIPORTATORIINATTIVI
Table 3. Multivariate-Adjusted Hazard Ratios (95% Confidence Intervals) of the Risk Predictors for Liver-Related Death
Included in the Cox Regression Models
All participants (n ! 20,069)
Variable
Cohort
Control
Inactive HBV carrier
Undetectable HBV DNA
HBV DNA 300-10,000 copies/mL
Age (increment by every decade)
Male sex (vs female)
ALT (high-normal vs low-normal)
Alcohol drinking habit (ever vs never)
Cigarette smoking habit (ever vs never)
Hazard ratio
(95% CI)
Inactive HBV carriers (n ! 1932)
P value
1.0
(referent)
—
2.4a
1.9a
2.3
1.8
1.9
2.1
1.7
(1.0"5.5)
(0.7"4.7)
(1.7"3.2)
(0.9"4.0)
(1.1"3.4)
(1.2"3.8)
(0.9"3.3)
.048
.188
$.001
.120
.025
.013
.094
Hazard ratio
(95% CI)
P value
1.0
0.8
2.6
1.7
0.3
5.8
1.2
(referent)
(0.2"2.7)
(1.2"5.3)
(0.3"10.9)
(0.04"2.7)
(1.5"21.9)
(0.3"4.6)
.733
.011
.552
.307
.010
.837
ALT, alanine aminotransferase; CI, confidence interval; HBV, hepatitis B virus.
aP ! .695 for the difference between serum HBV DNA 300"10,000 copies/mL vs undetectable.
hepatocellular carcinoma was the most striking risk pre- death for inactive HBV carriers through a communitydictor for liver-related death (HRa ! 611; 95% CI: based long-term follow-up study. As antiviral therapy for
CarriersofInac:veHepa::sBVirusAreS:llatRiskforHepatocellularCarcinomaandLiver-RelatedDeath.Jin-deChenetal.
325"1151). Older age was the only significant risk pre- chronic hepatitis B was not reimbursed by national
GASTROENTEROLOGY2010;138:1747–1754
skTable
Predictors
for Newly Developed
3. Multivariate-Adjusted
Hazard Ratios (95% Confidence Intervals) of the Risk Predictors for Liver-Related Death
Liverrelateddeath
Included inHCC
the Cox Regression Models
Inactive HBV carriers (n " 1932)
Hazard ratio
Variable (95% CI)
Cohort
Control
Inactive HBV carrier
1.0
(referent)
Undetectable HBV DNA
1.6
(0.6!4.5)
HBV DNA 300-10,000 copies/mL
2.6
(1.4!4.6)
Age (increment by every decade)
2.9
(0.7!11.8)
Male sex (vs female)
0.5
(0.1!2.3)
ALT (high-normal vs low-normal)
5.0
(1.6!15.6)
Alcohol drinking
habit
(ever
vs never)
0.5
(0.2!1.6)
Cigarette smoking habit (ever vs never)
HBVDNA
All participants
(n ! 20,069)
P value
Hazard ratio
Inactive HBV carriers (n ! 1932)
neg
(95% CI)
P value
Hazard ratio
(95% CI)
P value
1.0
0.8
2.6
1.7
0.3
5.8
1.2
(referent)
(0.2"2.7)
(1.2"5.3)
(0.3"10.9)
(0.04"2.7)
(1.5"21.9)
(0.3"4.6)
.733
.011
.552
.307
.010
.837
HBVDNA<2000UI/ml
.362
.002
.133
.374
.005
.245
1.0
(referent)
2.4a
1.9a
2.3
1.8
1.9
2.1
1.7
(1.0"5.5)
(0.7"4.7)
(1.7"3.2)
Alcool
(0.9"4.0)
(1.1"3.4)
(1.2"3.8)
(0.9"3.3)
ETA’
—
.048
.188
$.001
.120
.025
.013
.094
ALT, alanine aminotransferase; CI, confidence interval; HBV, hepatitis B virus.
ble.
aP ! .695 for the difference between serum HBV DNA 300"10,000 copies/mL vs undetectable.
hepatocellular carcinoma was the most striking risk pre- death for inactive HBV carriers through a communitydictor for liver-related death (HRa ! 611; 95% CI: based long-term follow-up study. As antiviral therapy for
325"1151). Older age was the only significant risk pre- chronic hepatitis B was not reimbursed by national
dictor independent of hepatocellular carcinoma for con- health insurance in Taiwan until 2003, the participants
trols, but not for inactive HBV carriers. Subcohort was no in this study had not received any antiviral treatment.
longer
an independent risk predictor for liver-related
CarriersofInac:veHepa::sBVirusAreS:llatRiskforHepatocellularCarcinomaandLiver-RelatedDeath.Jin-deChenetal.
Few studies in the past have addressed the long-term
GASTROENTEROLOGY2010;138:1747–1754
mortality when newly developed hepatocellular carci- follow-up of inactive HBV carriers. Gigi and colleagues10
Ø IlrischiodisviluppodiHCCperiportatoriinamviHBV
èmaggiorepercolorochepresentanounHBVDNA
misurabilerispeboacolorocherisultanoHBVDNA
NEGATIVI.TaledifferenzaNONèsignificaXva
Ø Inconsiderazionedelleevidenzeemerselasogliadi
HBVDNAconsiderataaffidabilenell’individuareil
portatoreinamvoèdi10000copie/ml
Ø L’etàèunimportantefaboredirischioperlosviluppo
diHCC
Ø IpazienXcheraggiungonoprimalostadiodiportatore
inamvohannounaminorpossibilitàdiavereuna
progressionedimalama
Tassoannualediincidenza
HCC0.06%
Tassoannualediincidenzadi
“liverrelateddeath”0.04%
Ø Valorinormali-alXdiALTnoncorrelanoconilrischiodi
HCCedimorte“fegatocorrelata”
Ø LosviluppodiHCCèilpiùimportantefaboredirischio
dimortalitàperiportatoriinamvi
CarriersofInac:veHepa::sBVirusAreS:llatRiskforHepatocellularCarcinomaandLiver-RelatedDeath.Jin-deChenetal.
GASTROENTEROLOGY2010;138:1747–1754
Natural history of chronic hepatitis B
C-J Chen and H-I Yang
Milestone 1:
Start of
decline of
HBV DNA
level
HBV DNA >108
copies/mL
HBeAg/Anti-HBe
status
Milestone 2:
HBeAg/
Anti-HBe
seroconversion
Milestone 3:
HBV DNA
decreased to
undetectable
level
Milestone 4:
Clearance of
HBsAg
HBV DNA level
HBeAg+, Anti-HBe-
HBeAg-, Anti-HBe+
Undetectable level
of HBV DNA
HBsAg+
HBsAg status
HBsAg-
ΔT
ALT level
Immune
tolerance
Immune
clearance
Residual
Figure 4 Natural history of chronic hepatitis B based on the Risk Evaluation of Viral Load Elevation and Associated Liver Disease/Cancer-Hepatitis
B Virus (REVEAL-HBV) Study findings.
MA…
Ø PazienX30-65anni
Ø Mancatodosaggioseriatodell’HBVDNA
Ø NonconsideraXigenoXpiHBV
CarriersofInac:veHepa::sBVirusAreS:llatRiskforHepatocellularCarcinomaandLiver-RelatedDeath.Jin-deChenetal.
GASTROENTEROLOGY2010;138:1747–1754
Digestive and Liver Disease 46 (2014) 427–432
Contents lists available at ScienceDirect
Digestive and Liver Disease
journal homepage: www.elsevier.com/locate/dld
Liver, Pancreas and Biliary Tract
Progression to cirrhosis, hepatocellular carcinoma and liver-related
mortality in chronic hepatitis B patients in Italy
Donatella Ieluzzi a,b,1 , Loredana Covolo c,1 , Francesco Donato c , Giovanna Fattovich a,d,∗
a
Division of Gastroenterology and Endoscopy, Azienda Ospedaliera Universitaria Integrata, Verona, Italy
Department of Surgery, University of Verona, Verona, Italy
Institute of Hygiene, Epidemiology and Public Health, University of Brescia, Brescia, Italy
d
Department of Medicine, University of Verona, Verona, Italy
b
c
a r t i c l e
i n f o
a b s t r a c t
Ø 105pazienX(F25,M80)etàmedia30anni
Article history:
Received 11 July 2013
Accepted 10 January 2014
Available online 16 February 2014
Keywords:
Chronic hepatitis B
Cirrhosis
Hepatocellular carcinoma
Liver-related mortality
Natural history
Background: The natural history of chronic hepatitis B is variable. We evaluated some of the risk factors for
cirrhosis, hepatocellular carcinoma and liver-related mortality in Italian patients with chronic hepatitis
B.
Methods: A cohort of 105 untreated patients with chronic hepatitis B without cirrhosis at diagnosis was
followed prospectively for a mean period of 23 years. Clinical, histological and ultrasound examinations,
biochemical and virological tests, and causes of death were analyzed.
Results: Forty-two (40%) patients became inactive carriers and 63 (60%) showed persistent alanine aminotransferase elevation: 13 (13%) associated with HBeAg persistence, 35 (33%) with detectable serum
HBV-DNA but HBeAg-negative, 11 (10%) with concurrent virus infection and 4 (4%) with non-alcoholic
fatty liver disease. Cirrhosis incidence was 1.56/100 person-years. Older age and sustained HBV replication predicted cirrhosis occurrence independently. Hepatocellular carcinoma incidence was 2.1/100
person-years in patients who developed cirrhosis and 0.06 in those who did not. Cirrhosis occurrence
was associated with an increased risk of hepatocellular carcinoma (hazard ratio 20.4, 95% confidence
interval 2.54–167.5) and liver-related death (16.5, 2.0–138.8).
Conclusions: In Italian patients with chronic hepatitis B cirrhosis strongly predicts hepatocellular carcinoma occurrence and disease-related mortality, thus indicating that early antiviral treatment should be
instituted before cirrhosis occurrence.
© 2014 Editrice Gastroenterologica Italiana S.r.l. Published by Elsevier Ltd. All rights reserved.
Ø Followupsemestrale(ecografia+esamiematochimici)peri
pazienXconepaXteamvaeannualepergliinacXvecarriers
(HBeAgnegaXvi,HBVDNA<limitesogliadirilievo)
1. Introduction
Chronic hepatitis B virus (HBV) infection is a worldwide public health problem, accounting for approximately half a million
deaths each year. The natural history of chronic HBV infection varies
from one individual to another and from one geographical area to
another, possibly due to differences in viral, host and environmental factors [1,2]. Several studies have described the characteristics,
clinical course and risk of liver-related complications of chronic
HBV infection in the Mediterranean area, but a comparison of the
results is hampered by different study design, the small number
of patients recruited, short follow-up and the heterogeneity of the
patient population in relation to the severity of chronic liver disease
at diagnosis.
A careful understanding of the clinical course and factors influencing progression of chronic hepatitis B (CHB) diagnosed at an
early stage would be particularly important for monitoring and taking evidence-based decisions on patient care in clinical practice. At
present many subjects with CHB undergo anti-viral treatment, the
standard of care consisting of life-long oral nucleos(t)ide analogues
(NAs), which have been found to suppress circulating viral loads
efficiently and can lead to regression of fibrosis [3]. At present few
data on the natural history of CHB in Western countries are available for evaluating the magnitude of the clinical benefit of antiviral
therapy.
In this study we aimed to investigate the natural history of CHB,
with emphasis on the risk of, and factors related to, clinical progression to cirrhosis, hepatocellular carcinoma (HCC) and liver-related
mortality in a cohort of Caucasian patients in Italy with CHB, without histological and clinical evidence of cirrhosis at diagnosis.
Ø Duratamediadelfollowup:23.2anni(28.8perIC*)
∗ Corresponding author at: Unità Operativa Complessa di Gastroenterologia
ed Endoscopia Digestiva dO, Dipartimento di Medicina, Azienda Ospedaliera
Universitaria Integrata Verona, Piazzale A. Stefani n. 1, 37126 Verona, Italy.
Tel.: +39 045 8127257; fax: +39 045 81272014.
E-mail address: [email protected] (G. Fattovich).
*InacXvecarrier
1
105pazienX
HBsAg-;AnXHBsAg+
2duranteHBeAg+prima
dellasieroconversionead
anXHBe
2HBeAgnegaXviprima
dellanormalizzazionedelle
transaminasi
38
NESSUNODEIPORTATORIINATTIVIHASVILUPPATOHCCo
èdecedutopercausecorrelateaproblemaXcheepaXche
*NB:difabopazienXgiàarrivaticirroXciprimadellafasediianmvità
LiverInternaXonal(2016)
IncidenceofhepatocellularcarcinomainuntreatedsubjectswithchronichepaXXsB:a
systemaXcreviewandmeta-analysis
ElenaRaffem1,GiovannaFabovich2andFrancescoDonato
Ø StudilongitudinalietrialsrandomizzaXcontrollaX(pz>18anni)
Ø SoggemcondiagnosidiepaXtecronica,cirrosi,portatoriinamvi(ALT
costantementenormali,HBeAgnegaXvi,anXHBeAgposiXvi),
portatoriasintomaXci
Ø StudidacuirilevaredaXidoneialcalcolodeitassidiincidenza
Ø 66studi,347859pazienX
Ø IncidenzaHCC
Outcomemeasure
Ø RischiorelaXvoHCCperareageografica,gradodimalama,genere,età
*
R
I
S
U
L
T
A
T
I
*x100/anno
EUROPA
Portatore
asintomaXco
0.07
N.AMERICA
ASIA
0.19
0.42
Portatoreinamvo
0.03
0.17
0.06
Ø L’incidenzadiHCCaumentainmanieracrescentedalportatoreinamvoalportatore
EpaXtecronica
0.12
0.48
0.49
asintomaXco,conepaXtecronicaeconcirrosicompensata
Cirrosi
2.03
2.89
3.37
Ø compensata
Correlazioneconetàmanonconareageografica
Ø Incrementodiduevoltedelrischioperunconsumoalcolicodi60g/die
Raffetti et al.
Incidence of HCC in subjects with chronic HBV
Ø MaggiorrischiodisviluppodiHCCpergenoXpoCrispeboalB
Ø HBsAg>1000IU/ml
Fig. 3. Five-year cumulative HCC risk according to macro-area and liver disease status (Europe and East Asia). Abbreviation: HCC, hepatocellular carcinoma.
Rischiodiriamvazione
E’ ufficio di chi governa fuggire
le guerre quanto si può, ma
appartiene anche alla sapienza
loro anticipare una guerra
molesta e pericolosa per fuggirne
una più molesta e pericolosa
Guicciardini-DiscorsipoliXci
HBsAg<1000,HBV
DNA<2000,normalALT
IMMUNOSOPPRESSIONE
IncrementoHBVDNA
RIPRISTINOIMMUNITA’
immunoricosXtuzione
IncrementoALT
EPATITEACUTA/FULMINANTE
KempinskaA,etall.Reac:va:onofhepa::sB
infec:onfollowingallogeneicbonemarrowLong-termsurveillance
ofhaematopoie:cstemcellrecipientswithresolved
transplanta:onina
TheoriginofIgG
hepa::sB:highriskofviralreac:va:oneveninarecipientwith
Changesinserologicmarkersofhepa::sBfollowingautologous
hepa::sB-immunepa:ent:casereportandreviewoftheliterature.
produc:onandhomogeneousIgGcomponentsa^erallogeneic
Severereac:va:onofhepa::sBvirusinfec:oninapa:ent
avaccinateddonor.JViralHepat2007;
hematopoie:cstemcelltransplanta:on.BiolBloodMarrow
ClinInfectDis2005;41:1277–1282
bonemarrowtransplanta:on.Blood1996;87:818–826
withhairycellleukemia:shouldlamivudineprophylaxisberecommended
Hepa::sBvirusreac:va:oninacaseofnon-Hodgkin’s
Transplant2007;13:463–468
toHBsAg-nega:ve,an:-HBc-posi:vepa:ents?
lymphomatreatedwithchemotherapyandrituximab:necessityof
Fatalhepa::s
Progressivedisappearanceofan:-hepa::sBsurface
Infec:on2006;34:282–284
prophylaxisforhepa::sBvirusreac:va:oninrituximabtherapy.
Breac:va:ona^erautologousbonemarrowtransplanta:on.
an:genan:bodyandreverseseroconversiona^erallogeneic
Thehepa::s
LeukLymphoma2004;45:627–629
BoneMarrowTransplant1989;4:207–208\
hematopoie:cstemcelltransplanta:oninpa:entswithprevious
Bviruspersistsfordecadesa^erpa:ents’recoveryfromacute
Fulminanthepa::sduetoreac:va:onof
hepa::sBvirusinfec:on.Transplanta:on2005;79:616–619
viralhepa::sdespiteac:vemaintenanceofacytotoxicT-lymphocyte
chronichepa::sBvirusinfec:ona^erallogeneicbonemarrow
Hepa::s
response.NatMed1996;2:1104–1108
transplanta:on.DigDisSci.1988;33:1185–91.
Bvirusreac:va:ona^erallogeneicbonemarrow
Lamivudinetherapyforchemotherapyinduced
transplanta:oninapa:entpreviouslycuredofhepa::sB.
reac:va:onofhepa::sBvirusinfec:on.AmJGastroenterol.
Hepa::s
GastroenterolClinBiol.1999;23:770–4.
Reac:va:onofhepa::sBa^ertransplanta:on
Bvirusreac:va:ona^erallogeneicbonemarrow
1999;94:249–51.
inpa:entswithpre-exis:ngan:-hepa::sBsurfacean:gen
Occurrenceandmanagementofhepa::sBvirus
transplanta:oninapa:entpreviouslycuredofhepa::sB.
an:bodies:reportonthreecasesandreviewoftheliterature.
reac:va:onfollowingkidneytransplanta:on.ClinNephrol.
GastroenterolClinBiol.1999;23:770–4.
Transplanta:on.1998;66:883.
Reac:va:onofhepa::sB
1998;49:385–8.
a^ertransplanta:onopera:ons.Lancet.1977;68:105–12
Hepa::sBvirusandhepa::sB-relatedviralinfec:onin
Reac:va:onofhepa::sBvirusinHBsAgnega:ve
renaltransplantrecipients.Gastroenterology1988;94:151–156
pa:entswithmul:plemyeloma:twocasereport
HepaXXsBreacXvaXoninthesemngofchemotherapyand
immunosuppression-prevenXonisbeberthancure
YoshidaetalIntJHematology.2010Jun,91(5):844-9
WJH2015
Tra)amentodell’epa2teBcronica:raccomandazionidaunworkshopitaliano-
Diges2veandLiverDisease40(2008)603-617
La profilassi è indicata:
Nei portatori inattivi di HBsAg sottoposti a chemioterapia antitumorale o a
trattamento immunosoppressivo ad alto rischio: anti-TNF, anti CD20, anti
CD56 a steroidi a dosaggi medio elevati (>7.5mg/die) per periodi
prolungati, ciclofosfamide, metotrexato, leflunomide, ciclosporina,
tacrolimus, azatioprina, micofenolato
I portatori cronici inattivi e i pazienti HBsAg negativi e anti-HBc-positivi
devono essere sottoposti a profilassi fin dall’inizio del trattamento
immunosoppressivo o, se possibile, a partire da 2-4 settimane prima che
cominci la somministrazione dei farmaci immunosoppressori (CIII)
La profilassi mirata deve essere iniziata al momento della riattivazione
della malattia (HBV-DNA >2000UI/ml) nei portatori di HBsAg, e
immediatamente dopo la sieroconversione nei pazienti che diventano
HBsAg positivi (CIII)
Risk stratification for HBV reactivation
Drugs
High
Disease
Oncohematology
and BMT
IBD
Medium
TNFa-inhibitors
Other biological DMARDs
Leflunomide
Methotrexate
Cyclophosfamide
HBsAg+
Combination therapies
Medium/high-dose prednisone (>7.5 mg/die)
Null Low
Rheum
RISK
HIV
HBsAg+
anti-HBc+
Rituximab
combined
therapy
SOTs
Virus
Calcineurin inhibitors
Azathioprine
6-mercaptopurine
Low-dose prednisone (<7.5 mg/die)
Sulfasalazine
Hydroxychlorochine
Marzano A et al., DLD 2007 (2011)
RischiodiriamvazioneneipazienX
immunocompromessi
BonemarroworstemcelltransplantaXon
HBsAg-posiXve
HBsAg-negaXve,anX-HBc-posiXve
32–50%
upto50%
AnX-CD20monoclonalanXbodies(rituximab)
HBsAg-posiXve
HBsAg-negaXve,anX-HBc-posiXve
50-80%
18%
SolidorgantransplantaXon
HBsAg-posiXve
HBsAg-negaXve,anX-HBc-posiXve
50-90%
0.9-5%
39-41%
3%
39%
5%
Systemiccancerchemotherapy
HBsAg-posiXve HBsAg-negaXve,anX-HBc-posiXve
TNF-alfaantagonists
HBsAg-posiXve HBsAg-negaXve,anX-HBc-posiXve
Hwang and Lok Nat Rev Gastroenterol 2013
Hepat Mon. 2016 April; 16(4):e35810.
doi: 10.5812/hepatmon.35810.
Review Article
Published online 2016 March 26.
Hepatitis B Reactivation During Immunosuppressive Therapy or
Cancer Chemotherapy, Management, and Prevention: A
Comprehensive Review
Soheil Tavakolpour,1 Seyed Moayed Alavian,1,* and Shahnaz Sali2
1
Baqiyatallah Research Center for Gastroenterology and Liver Diseases, Baqyiatallah University of Medical Sciences, Tehran, IR Iran
Infectious Diseases and Tropical Medicine Research Center, Shahid Beheshti University of Medical Sciences, Tehran, IR Iran
2
*
Corresponding author: Seyed Moayed Alavian, Baqiyatallah Research Center for Gastroenterology and Liver Diseases, Baqyiatallah University of Medical Sciences, Tehran, IR
Iran. Tel/Fax: +98-2181264070, E-mail: [email protected]
Tavakolpour
Received 2015 December 26; Revised 2016 January 17; Accepted 2016 January 27.
Ø Lalamivudinapuòessereconsideratacomelapiùcomunescelta
Abstract
perlaprofilassineipazienXHBV
avoided in cases under HSCT, even in the presence of complete remission (52, 61). Thus, prophylaxis longer than
24 months was recommended for these patients (54). On
the issue of HSCT, several studies have reported HBVr after
more than
Context: Due to the close relationship between the immune system and the hepatitis B virus (HBV) replication, it is essential
to 12 months, reaching a peak of 91 months (27, 54,
56, 61).
monitor patients with current or past HBV infection under any type of immunosuppression. Cancer chemotherapy, immunosupConsidering the high resistance to lamivudine (LAM),
in are
addition
pressive therapies in autoimmune diseases, and immunosuppression in solid organ and stem cell transplant recipients
the to various reported cases with a risk of reactivation following more than 6 months from the cessation
major reasons for hepatitis B virus reactivation (HBVr). In this review, the challenges associated with HBVr are discussed according
of immunosuppressive therapy or chemotherapy, it is recommended
to the latest studies and guidelines. We also discuss the role of treatments with different risks, including anti-CD20 agents,
tumor that referenced HBV antiviral agents, such as
entecavir (ETV) and TNV should be used in therapies that
necrosis factor-alpha (TNF- ) inhibitors, and other common immunosuppressive agents in various conditions.
need long-term prophylaxis. Recommendations of various
bodies
associated with HBVr are shown in Table 2.
Evidence Acquisition: Through an electronic search of the PubMed, Google Scholar, and Scopus databases, we selected the
studies
In a meta-analysis, LAM prophylaxis in HBsAg carriers
associated with HBVr in different conditions. The most recent recommendations were collected in order to reach a consensus
on
with breast cancer under chemotherapy was introduced as
an effective option in the reduction of HBVr (95). Based on
how to manage patients at risk of HBVr.
a systematic review, LAM prophylaxis had appeared as an
Results: It was found that the positive hepatitis B surface antigen (HBsAg), the high baseline HBV DNA level, the positive effective
hepatitis
option in the reduction of HBVr in HBsAg-positive
B virus e antigen (HBeAg), and an absent or low hepatitis B surface antibody (HBsAb) titer prior to starting treatment are lymphoma
the most patients undergoing chemotherapy. After that,
preventing reactivation caused a decrease in the disrupimportant viral risk factors. Furthermore, rituximab, anthracycline, and different types of TNF- inhibitors were identified
as the
tion of the chemotherapy (96).
high-risk therapies. By analyzing the efficiency of prophylaxis on the prevention of HBVr, it was concluded that those with a high
In risk
another report, anti-HBc-positive patients under immunosuppressive therapy were included (97). These paof antiviral resistance should not be used in long-term immunosuppressants. Receiving HBV antiviral agents at the commencement
tients suffered from various autoimmune diseases. Among
of immunosuppressant therapy or chemotherapy was demonstrated to be effective in decreasing the risk of HBVr. Prophylaxis
could
those
who had received antiviral therapy, none indicated
in HBV DNA levels, while 11.5% of the control group
also be initiated before the start of therapy. For most immune suppressive regimes, antiviral therapy should be kept up foraatrise
least
6
did experience an increase. ALT elevation was significantly
months after the cessation of immunosuppressive drugs. However, the optimal time of prophylaxis keeping should be increased
lower in in
the antiviral prophylactic group. Additionally, one
in the control group showed reverse seroconvercases associated with rituximab or hematopoietic stem cell transplants. According to the latest studies and guidelines frompatient
different
sion. In contrast, no reverse seroconversion was observed
bodies, recommendations regarding screening, monitoring, and management of HBVr are outlined.
in the prophylactic group.
LAM can be considered as the most common prophyConclusions: Identification of patients at the risk of HBVr before immunosuppressive therapy is an undeniable part of treatment.
laxis in HBV patients. However, there is a considerable risk
Starting the antiviral therapy, based on the type of immunosuppressive drugs and the underlying disease, could lead to better
manof LAM
resistance risk in patients with active HBV. Based on
the literature, LAM is an appropriate choice in cases with
agement of disease.
high viral replication that need short-term treatments. In
contrast, it was not recommended for HBsAg carriers with
Hepatitis B Virus, Reactivation, Immunosuppression, Rituximab, Prophylaxis
detectable HBV DNA levels at baseline, who are candidates
for long-term immunosuppressive therapy. Accordingly,
it can be concluded that LAM prophylaxis is a reasonable
choice for OBI/resolved HBV patients.
LAM is more common in countries with a high preva-
Ø Lalamivudinarappresentaunasceltaappropriataneicasicon
elevatareplicaviralechenecessitanoditrabamenXdibreve
↵
durata
Ø SceltaragionevolenegliOBI
Keywords:
↵
La lamivudina si è mostrata efficace nella profilassi della riacutizzazione
HBV(0.9% vs 25-85% dei non trattati negli studi retrospettivi e 5% vs 24 negli
studi prospettici)
2008
La profilassi con lamivudina è indicata nei pazienti HBsAg+ con HBV DNA <
2000 UI/ml,; nei pazienti con HBV DNA> 2000UI/ml , che devono essere
sottoposti a cicli di durata maggiore o ripetuti, è indicato l’utilizzo di analoghi
ad alta barriera genetica (tenofovir o entecavir)
2012
La terapia profilattica antivirale è raccomandata per i portatori di HBV all’
inizio della terapia ed almeno sei mesi dopo, i farmaci ad alta barriera genetica
sono raccomandati quando previsti trattamenti di lunga durata o quando
vengono utilizzati farmaci ad alto rischio come il Rituximab
2016
La profilassi è indicata nei pazienti HBsAg che devono essere sottoposti a
chemioterapia o a regimi di immunosoppressione sia durante che per 6-12
mesi dopo la fine del trattamento
2016
with normal baseline ALT has been reported to be higher during
the first year (15–20%) [12,14] and declines after 3 years of follow-up [9,14,15], frequent monitoring during the first 1–3 years
is critical in determining whether a patient has PNALT.
Besides the frequency of determinations and duration of follow-up, definition of PNALT should include standardized criteria
for the upper limit of normal (ULN) of ALT. Some investigators
have suggested that lower cut-offs than the traditional values
defined by most diagnostic laboratories (around 40 IU/L) should
be used. These suggestions were derived from studies based on
single ALT values in Italian blood donors [16], the associations
between normal ALT and increased rates of liver related deaths
in Koreans applying for life insurance [17], and high serum HBV
DNA levels or increased risks of complications of liver disease
tional cut-offs for the ULN of ALT values in patients with
HBeAg-negative chronic HBV infection.
Severe liver histological lesions were rare among HBeAg-negative patients with truly PNALT. In the four studies with good or
acceptable definitions of PNALT [7,8,11,12], more than a minimal
(always mild) inflammatory activity was detected in only 3% and
more than mild fibrosis always with minimal inflammatory activity in only 5% (moderate fibrosis: 4.5%, severe fibrosis: 0.5%, cirrhosis: 0%) of 215 patients with serum HBV DNA 620,000 IU/
ml. The prevalence of mild inflammatory activity and moderate
fibrosis was 7% and 10% among patients with HBV DNA levels
between 2000 and 20,000 IU/ml and 1.4% and 1% among those
with HBV DNA levels <2000 IU/ml. Similar mild histological findings in HBeAg-negative patients with HBV DNA 620,000 IU/ml
Qualefollowup?
Review
Follow-up and indications for liver biopsy in HBeAg-negative
chronic hepatitis B virus infection with persistently normal ALT:
A systematic review
George V. Papatheodoridis1,⇑, Spilios Manolakopoulos1, Yun-Fan Liaw2, Anna Lok3
1
HBeAg-negative patient with normal ALT at baseline
2nd Department of Internal Medicine, Athens University Medical School, ‘‘Hippokration’’ General Hospital of Athens, Greece; 2Liver Research
Unit, Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Taipei, Taiwan; 3Division of
Gastroenterology and Hepatology, University of Michigan Health System, Ann Arbor, MI, USA
ALT every 3-4 mo for one year
+ serum HBV DNA determination
Introduction
Background & Aims: The adequacy of monitoring HBeAg-negaALT >ULN
and/or
Persistently ALT <ULN and
Persistently ALT <ULN and
tive patients based
on ALT
activity is controversial and current
HBV DNA
IU/ml
HBVnorDNA 2000-20,000
IU/mlapproximately 400 million people
HBV DNA
<2000
IU/ml
Worldwide,
have
chronic
infecguidelines favor
liver>20,000
biopsy in
HBeAg-negative cases with
tion with hepatitis B virus (HBV), which usually runs a variable
mal ALT and HBV DNA >2000 IU/ml. We systematically reviewed
course lasting for decades and often the entire life, with outcomes
all the available histological data on HBeAg-negative patients
ALT every 3-4 mo,
ranging from asymptomatic carrier state to cirrhosis, liver failure,
with persistently normal ALT (PNALT) to determine the prevaHBV DNA every year and
and hepatocellular
carcinoma (HCC) [1–4].ALT
Theevery
natural
history of
lence of significant
liver
disease
and
its
associating
factors.
Liver biopsy
6 mo*
transient elastography
every year
chronic
Methods: Literature search to identify studies with adult HBeAgfor two more
yearsHBV infection has been divided into different phases, based
on hepatitis B e antigen (HBeAg) status, serum HBV DNA levels, and
negative patients who had PNALT as defined by the authors, a
alanine aminotransferase (ALT) activity [1,2].
minimum follow-up of 1 year and histological data. Traditional
In the HBeAg-negative phases, the majority of patients remain
cut-off values of normal ALT were used in all studies. The definiALT <ULN and
DNA 2000-20,000
IU/ml low-replicative state (inactive HBV carrier state).
in an inactive,
tions of PNALT were considered as acceptable or good HBV
if there
Inactive carriers are negative for HBeAg; and have persistently
were P3 ALT determinations at unspecified intervals during 6–
normal ALT (PNALT), low or undetectable serum HBV DNA levels,
12 months or predefined intervals during P12-month periods,
ALT every
6 mo, or no necroinflammation and generally minimal to mild
minimal
respectively.
HBV
DNA every
year and
fibrosis
on liver biopsy. A proportion of HBeAg-negative patients,
Results: Six studies including 335 patients met our inclusion
critransient
everymay
yearprogress to an immune active phase (HBeAg-neghowever,
teria. Of these, four studies with 246 patients had good or
accept-elastography
ative chronic hepatitis B) with persistently or transiently elevated
able definitions of PNALT. In the latter four studies, more than
ALT and high serum HBV DNA levels [1–3].
minimal (usually mild) necro-inflammatory activity was
ALT >ULN and/or,
Theoretically, serum levels of ALT, an enzyme that is released
observed in 10% and more than mild fibrosis in 8% of all patients
HBV DNA >20,000 IU/ml and/or
from hepatocytes
liver
should reflect the degree of
(moderate fibrosis: 7%, severe fibrosis: 1%, cirrhosis: 0%), and in
liverduring
stiffness
>9 injury,
kPa
liver damage [5]. However, several reports have suggested that
3% and 5% of patients with HBV DNA 620,000 IU/ml, respectively.
patients with chronic HBV infection who are HBeAg negative
Conclusions: Histologically significant liver disease is rare in
and have normal ALT may have high serum HBV DNA levels
HBeAg-negative patients with PNALT based on stringent criteria
Liver biopsy
and significant histological
liver damage [6,7]. Such cases have
and serum HBV DNA 620,000 IU/ml. Such cases can be considcreated debates and clinical dilemmas regarding the adequacy
ered as true inactive HBV carriers, who require neither liver
Fig. 1. Clinical algorithm for the optimal follow-up and management of patients with HBeAg-negative chronic HBV infection and normal alanine aminotransferase
of monitoring HBeAg-negative patients based on ALT activity
biopsy(ALT)
noractivity
immediate
therapy but continued follow-up.
at baseline. All patients should have ALT and HBV DNA monitoring every 3–4 months during the first year. Patients with ALT persistently below ULN and HBV
⁄
only,
the need
liver
biopsy, and
indication
for treatment
! 2012
European
Association
for the
the Liver.
Published
DNA
<2000 IU/ml
during the first
yearStudy
may beofmonitored
with
ALT every 6 months.
Periodical
HBVfor
DNA
measurements
may the
be also
helpful, although
the optimal
JV.Papatheodoridisetal.JournalofHepatology2012vol.57j196–202
[3].
Welimit
systematically
reviewed
all the
available
histological
data
by Elsevier
B.V.
All rights
reserved.
frequency
of HBV
DNA monitoring
is unclear. Patients with ALT persistently below the
upper
of normal (<ULN)
and HBV DNA
2000–20,000
IU/ml
during the first
year
Review
Grazieperl’abenzione
IngeneraleloscreeningèconsideratocosteffecXvequandol’incidenza
annualediHCCeccedelo0.2%neinoncirroXciel’1.5%neipazienXcirroXci