D.L.gs 9 aprile 2008, n.81
Segnale di rischio biologico
D.L.gs 9 aprile 2008, n.81
TITOLO X
Esposizione ad agenti biologici
Capo I
Art 267. Definizioni.
1. Ai sensi del presente titolo si intende per:
a) agente biologico: qualsiasi microorganismo anche se geneticamente
modificato, coltura cellulare ed endoparassita umano che potrebbe
provocare infezioni, allergie o intossicazioni;
b) microorganismo: qualsiasi entità microbiologica, cellulare o
meno, in grado di riprodursi o trasferire materiale genetico;
c) coltura cellulare: il risultato della crescita in vitro di
cellule derivate da organismi pluricellulari.
D.L.gs 9 aprile 2008, n.81
75. Classificazione degli agenti biologici.
1. Gli agenti biologici sono ripartiti nei seguenti quattro gruppi
a seconda del rischio di infezione:
a) agente biologico del gruppo 1: un agente che presenta poche
probabilità di causare malattie in soggetti umani;
b) agente biologico del gruppo 2: un agente che può causare
malattie in soggetti umani e costituire un rischio per i
lavoratori; è poco probabile che si propaga nella comunità; sono di
norma disponibili efficaci misure profilattiche o terapeutiche;
c) agente biologico del gruppo 3: un agente che può causare
malattie gravi in soggetti umani e costituisce un serio rischio per
i lavoratori; l'agente biologico può propagarsi nella comunità, ma
di norma sono disponibili efficaci misure profilattiche o
terapeutiche;
d) agente biologico del gruppo 4: un agente biologico che può
provocare malattie gravi in soggetti umani e costituisce un serio
rischio per i lavoratori e può presentare un elevato rischio di
propagazione nella comunità; non sono disponibili, di norma,
efficaci misure profilattiche o terapeutiche.
RISCHIO INFETTIVO NELLE
PROFESSIONI SANITARIE
• Infezione
– nosocomiale
– occupazionale
– operatore
paziente
• Stima rischio
– % sieropositività
– probabilità trasmissione (%sieroconversione)
– frequenza infortuni
+ possibilità immunizzazione
+ efficacia PEP
Prevalenza di infezioni da HBV, HCV e HIV
nella popolazione afferente alle
strutture sanitarie
8
7
%
6
5
4
3
2
1
0
HBV
HCV
HIV
Linee guida SIMLII-2003 draft
Contagio per contatto percutaneo con
sangue infetto da HBV, HCV, HIV
Stato del
paziente
Effetto
%
HbsAg+
HbeAg+
Sieroconversione 37-62%
HbsAg+
HbeAg-
Sieroconversione 23-37%
HCV+
Sieroconversione 1.8%
HIV+
Sieroconversione 0.3%
Distribuzione infortuni in ambiente
ospedaliero (Roma, n = 942)
100
80
60
40
% Infortuni
20
0
Area medica
Area
chirurgica
Servizi
Infortuni biologici/totale infortuni
aziende sanitarie Emilia Romagna
(2003-2006)
40
% infortuni
38
36
34
32
30
2003
2004
2005
2006
Tipologia infortuni biologici in
ambiente ospedaliero (Pisa 1993-95)
da taglio
da punta
da schizzo
altro
Infortuni sul lavoro in strutture sanitarie
della Regione Veneto denunciati all’INAIL
Modalità di accadimento
Anni 1994-2000
Totale n° 9053
Caduta, scivolamento
25%
Incidente stradale
23%
Urti-contatti con utensili, macchine, arredi...
17%
Movimentazione cose o persone
17%
Contatti con frammenti, liquidi, polveri
8%
Contatti con materiale biologico infetto
5%
Aggressioni
5%
(Bartolucci et al.; G Ital Med Lav Ergon 2002;24:392-397; www.gimle.fsm.it)
RISCHIO INFETTIVO NELLE
PROFESSIONI SANITARIE
Agenti
• HBV, HCV
• HIV
• Salmonella
• HAV
• TBC
• Influenza
• SARS-CoV
• (Sarcoptes scabiei,
hom.)
Tubercolosi
• Contagio: TBC polmonare non sospettata
• Aumento suscettibilità:
– tubercolino negativi
– immunodepressione
Tubercolosi
• Aumento rischio:
–
–
–
–
TBC polmonare o vie aeree
caverne
Espettorato BK+
non sufficiente chemioterapia
– Tosse ed espirazioni forzate
– Espettorato indotto
– ambienti piccoli
– scarsa ventilazione
– ricircolo aria
Tubercolosi
Prevenzione
• Ambienti
• Assunzione:
– test tubercolina (Quantiferon, Elispot)
– (Rx torace)
– vaccinazione BCG (non obbligatoria dal 2000)
• DPI
Severe Acute Respiratory Syndrome
OMS (sett. 2003): 8437 casi, 813 decessi, mortalità 9.6%
21% di casi in professioni sanitarie
Coronavirus from SARS isolated in FRhK-4 cells.
Thin section electron micrograph and negative stained virus particles
Department of Microbiology,
The University of Hong Kong and the Government Virus Unit,
Department of Health,
Hong Kong SAR China
Severe Acute Respiratory Syndrome
www.cdc.gov/ncidod/sars
www.who.int/sars/en
www.ministerosalute.it
scientifico.pneumonet.it/focus/sars
CORONA VIRUS
MHV: murine hepatitis virus
AIBV: avian infectious bronchitis virus
HcoV: human coronavirus
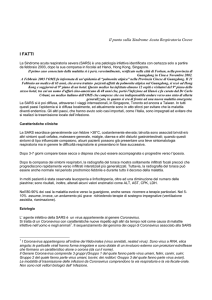
FACT SHEET
Basic Information about SARS
SARS Severe acute respiratory syndrome (SARS) is a viral
respiratory illness caused by a coronavirus, called SARS-associated
coronavirus (SARS-CoV). SARS was first reported in Asia in February
2003. Over the next few months, the illness spread to more than two
dozen countries in North America, South America, Europe, and Asia.
The SARS global outbreak of 2003 was contained; however, it is
possible that the disease could re-emerge.
How SARS spreads The main way that SARS seems to spread is by close
person-to-person contact. The virus that causes SARS is thought to be
transmitted most readily by respiratory droplets (droplet spread) produced when
an infected person coughs or sneezes. Droplet spread can happen when
droplets from the cough or sneeze of an infected person are propelled a short
distance (generally up to 3 feet) through the air and deposited on the mucous
membranes of the mouth, nose, or eyes of persons who are nearby. The virus
also can spread when a person touches a surface or object contaminated with
infectious droplets and then touches his or her mouth, nose, or eye(s). In
addition, it is possible that the SARS virus might spread more broadly through
the air (airborne spread) or by other ways that are not now known (Rat vector
hypothesis, Lancet 2003; 362:570-2).
Indice di trasmissibilità: R0 = 2.5-3 (influenza R0 = 7)
Symptoms of SARS
In general, SARS begins with a high fever (temperature greater than >38.0°C.
Other symptoms may include headache, an overall feeling of discomfort, and
body aches. Some people also have mild respiratory symptoms at the outset.
About 10 percent to 20 percent of patients have diarrhea.
After 2 to 7 days, SARS patients may develop a dry cough. Most patients
develop pneumonia.
Hong Kong:
linfopenia (<1000/mm3)(90%)
> LDH (71%)
Case definitions (WHO, revised may 2003)
Suspect case
1. A person presenting after 1 November 20021 with history of:
- high fever (>38 °C)
AND
- cough or breathing difficulty
AND one or more of the following exposures during the 10 days prior to onset of symptoms:
- close contact with a person who is a suspect or probable case of SARS;
- history of travel, to an area with recent local transmission of SARS
- residing in an area with recent local transmission of SARS
2. A person with an unexplained acute respiratory illness resulting in death after 1
November 2002, but on whom no autopsy has been performed
AND one or more of the following exposures during to 10 days prior to onset of symptoms:
- close contact, with a person who is a suspect or probable case of SARS;
- history of travel to an area with recent local transmission of SARS
- residing in an area with recent local transmission of SARS
Probable case
1. A suspect case with radiographic evidence of infiltrates consistent with pneumonia or
respiratory distress syndrome (RDS) on chest X-ray (CXR).
2. A suspect case of SARS that is positive for SARS coronavirus by one or more assays.
3. A suspect case with autopsy findings consistent with the pathology of RDS without an
identifiable cause.
Criteri diagnostici OMS: sensibilità 26%
Laboratory Criteria¶
• Confirmed
• Detection of antibody to SARS-associated coronavirus (SARS-CoV) in
a serum sample, or
• Detection of SARS-CoV RNA by RT-PCR confirmed by a second PCR
assay, by using a second aliquot of the specimen and a different set of
PCR primers, or
• Isolation of SARS-CoV.
• Negative
• Absence of antibody to SARS-CoV in a convalescent–phase serum
sample obtained >28 days after symptom onset.
• Undetermined
• Laboratory testing either not performed or incomplete.
Exclusion Criteria
A case may be excluded as a suspect or probable SARS case if:
• An alternative diagnosis can fully explain the illness.
• The case has a convalescent-phase serum sample (i.e., obtained >28
days after symptom onset) for which is negative for antibody to SARSCoV.
• The case was reported on the basis of contact with an index case that
was subsequently excluded as a case of SARS, provided other possible
epidemiologic exposure criteria are not present.
SARS: prevenzione in ambiente sanitario
Misure organizzative
• allertare P.S.
• segnalazione ASL e Ministero salute, dopo accertamento di
caso sospetto
• ventilazione ambienti
Operatore
• vaccinazione antiinfluenzale
• Precauzioni standard:
– igiene mani, DPI
• Precauzioni per trasmissione da contatto:
– cambiare i guanti, DPI e biancheria all’interno della stanza,
– disinfezione superfici
• Precauzioni per trasmissione per via aerea
– maschera FFP2 o FFP3 (nella stanza del paziente)
SARS: prevenzione in ambiente sanitario
Paziente (da sospetto)
• Isolamento
– stanza a pressione negativa
– stanza singola con bagno separato
– stanza con paz. = patologia
• Mascherina chirurgica, senza vavola, nel
trasporto
www.ecdc.eu.int
Influenza virus
Recommendations for Avian Influenza
All patients who present to a health-care setting with fever and
respiratory symptoms should be managed according to
recommendations for respiratory hygiene and cough etiquette
(www.cdc.gov/flu/professionals/infectioncontrol/resphygiene.htm)
and questioned regarding their recent travel history.
Patients with a history of travel within 10 days to a country with
avian influenza activity and are hospitalized with a severe febrile
respiratory illness, or are otherwise under evaluation for avian
influenza, should be managed using isolation precautions identical
to those recommended for patients with known Severe Acute
Respiratory Syndrome (SARS).
WHO: Influenza A/H5N1 (www.who.int)
Rationale for Enhanced Precautions
Human influenza is thought to transmit primarily via large respiratory
droplets.
Standard Precautions plus Droplet Precautions are recommended for the
care of patients infected with human influenza. However, given the
uncertainty about the exact modes by which avian influenza may first
transmit between humans additional precautions for healthcare workers
involved in the care of patients with documented or suspected avian
influenza may be prudent.
The rationale for the use of additional precautions for avian influenza as
compared with human influenza include the following:
• The risk of serious disease and increased mortality from highly
pathogenic avian influenza may be significantly higher than from infection
by human influenza viruses.
• Each human infection represents an important opportunity for avian
influenza to further adapt to humans and gain the ability to transmit more
easily among people.
• Although rare, human-to-human transmission of avian influenza may be
associated with the possible emergence of a pandemic strain.
Vaccination of Healthcare Workers against
Human Influenza
Health-care workers involved in the care of patients with
documented or suspected avian influenza should be vaccinated
with the most recent seasonal human influenza vaccine.
In addition to providing protection against the predominant
circulating influenza strain, this measure is intended to reduce the
likelihood of a healthcare worker’s being co-infected with human
and avian strains, where genetic rearrangement could take place,
leading to the emergence of potential pandemic strain.
• Standard Precautions
• Pay careful attention to hand hygiene before and after all
patient contact or contact with items potentially contaminated
with respiratory secretions.
• Contact Precautions
• Use gloves and gown for all patient contact.
• Use dedicated equipment such as stethoscopes, disposable
blood pressure cuffs, disposable thermometers, etc.
• Eye protection (i.e., goggles or face shields)
• Wear when within 3 feet of the patient.
Airborne Precautions
• Place the patient in an airborne isolation room (AIR). Such
rooms should have monitored negative air pressure in
relation to corridor, with 6 to 12 air changes per hour (ACH),
and exhaust air directly outside or have recirculated air
filtered by a high efficiency particulate air
(HEPA) filter.
If an AIR is unavailable, contact the health-care facility
engineer to assist or use portable HEPA filters to augment
the number of ACH.
• Use a fit-tested respirator, at least as protective as a
National Institute of Occupational Safety and Health
(NIOSH)-approved N-95 filtering face piece (i.e., disposable)
respirator, when entering the room.
Surveillance and Monitoring of Healthcare Workers
Instruct healthcare workers to be vigilant for the development of
fever, respiratory symptoms, and/or conjunctivitis (i.e., eye
infections) for 1 week after last exposure to avian influenzainfected patients.
Healthcare workers who become ill should seek medical care and,
prior to arrival, notify their healthcare provider that they may have
been exposed to avian influenza. In addition, employees should
notify occupational health and infection control personnel at their
facility.
With the exception of visiting a health-care provider, health-care
workers who become ill should be advised to stay home until 24
hours after resolution of fever, unless an alternative diagnosis is
established or diagnostic tests are negative for influenza A virus.
While at home, ill persons should practice good respiratory hygiene
and cough etiquette to lower the risk of transmission of virus to
others.
RISCHIO INFETTIVO NELLE
PROFESSIONI SANITARIE
Agenti
• HBV, HCV
• HIV
• Salmonella
• HAV
• TBC
• Influenza
• SARS-CoV
• (Sarcoptes scabiei,
hom.)
Contagio per contatto percutaneo con
sangue infetto da HBV, HCV, HIV
Stato del
paziente
Effetto
%
HbsAg+
HbeAg+
Epatite
Sieroconversione
22-31%
37-62%
HbsAg+
HbeAg-
Epatite
Sieroconversione
1-6%
23-37%
HCV+
Sieroconversione
1.8%
HIV+
Sieroconversione
0.3%
Sangue HIV+
contatto mucose: 0.09%
contatto cute: <0.09%
Precauzioni universali
• Guanti monouso
• Mascherine e occhiali
• Camici
• Lavaggio mani
• Prevenzione incidenti da oggetti taglienti
• Minimizzare respirazione bocca a bocca senza precauzioni
• No assistenza diretta o manipolazione apparecchiature per
portatori di lesioni essudative e dermatiti secernenti
• Adozione scrupolosa delle misure preventive in gravidanza
Protocollo di profilassi attiva-passiva in
caso di incidente biologico
• Pulizia della parte contaminata:
– cute: acqua e sapone, poi amuchina 5-10% o Betadine
– mucose: acqua corrente
• Prelievo di sangue all’operatore e al paziente
(consenso) per markers HBsAg, anti-HCV, anti-HIV
(test rapido) > recapitato dall’infortunato
• Se paziente HIV+ o dubbio > accesso a Mal.
Infettive entro 4 ore
• Se negativo o non identificabile > Mal. Infettive
entro 48 ore
Morb Mort Wkly Rep 2001; 50 (RR-11):1-42
Updated U.S. Public Health Service Guidelines for the management of occupational exposures
to HBV, HCV and HIV and recommendations for postexposure prophylaxis
Morb Mort Wkly Rep 2001; 50 (RR-11):1-42
Updated U.S. Public Health Service Guidelines for the management of occupational exposures
to HBV, HCV and HIV and recommendations for postexposure prophylaxis
Morb Mort Wkly Rep 2001; 50 (RR-11):1-42
Profilassi post-esposizione (PPE) per HIV
(Linee guida SIMLII-2003 draft)