FINASTERIDE (PROSCAR)
Dubbi
Un solo studio
Per quanto tempo deve durare il
trattamento?
Può essere prescritto anche alle
donne?
RIFAMPICINA (RIFADIN)
Farmaco antitubercolare che
blocca la trascrizione dell’RNA
Induce il citocromo P450,3A4, che
aumenta il metabolismo degli
steroidi
Razionale
Riduce i livelli endogeni di steroidi
RIFAMPICINA (RIFADIN)
Prima osservazione:
Miglioramento di CRSC con
terapia antitubercolare (che
comprendeva rifampicina) >
peggioramento dopo
sospensione rifampicina >
miglioramento con ripresa
farmaco
(Ravege. ARVO 2011)
RIFAMPICINA (RIFADIN)
Oral rifampin utilisation for the treatment of chronic
multifocal central serous retinopathy
RIFAMPICINA (RIFADIN)
Nathan C Steinle, Naina Gupta, Alex Yuan, Rishi P Singh
Department of Ophthalmology,
Cole Eye Institute, Cleveland
Clinic Foundation, Cleveland,
Ohio, USA
Correspondence to
Dr Rishi P Singh, Cole Eye
Institute, Cleveland Clinic
Foundation, 9500 Euclid
Avenue, i-32, Cleveland OH
44195, USA; [email protected]
Accepted 27 June 2011
Published Online First
3 November 2011
ABSTRACT
Chronic central serous retinopathy (CSR) is characterised
by frequent exacerbations and a poor visual prognosis.
Very few therapies exist for chronic CSR, and the
existing therapies are often ineffective. Thus, novel
therapies to combat this frustrating disorder are needed.
Presented here is a case detailing a patient with chronic
CSR with persistent subfoveal fluid of 2 years’ duration
that completely resolved with 1 month of oral rifampin
therapy. As a cytochrome P450, 3A4 inducer, rifampin is
thought to favourably alter the metabolism of
endogenous steroids, thereby leading to an improvement
in CSR manifestations.
on 12 May 2008. Because of the lack of the anticipated visual acuity improvement following cataract
surgery, the patient was referred to a retina
specialist for further evaluation.
On exam, the patient was noted to have diffuse
macular retinal pigmented epithelial changes
in both eyes. A fluorescein angiogram revealed
numerous patchy areas of hyperfluorescence in
both maculas consistent with the retinal pigment
epithelial changes noted on exam (figure 1). Spectral-domain optical coherence tomography (SDOCT) images revealed diffuse subretinal fluid in the
right eye, without intraretinal cystic spaces, with
preservation of the foveal contour and a thickened
underlying choroid (figure 2A). Both the clinical
exam and ophthalmic imaging exams pointed
towards a diagnosis of multifocal chronic central
serous retinopathy (CSR). The patient had
a history of non-insulin-dependent diabetes but had
no visible diabetic retinopathy in either fundus, and
his haemoglobin A1c was 6.1% at the time of the
1 case report con miglioramento
di CRSC dopo 2 anni di
osservazione
riassorbimento completo liquido
dopo 1 mese di terapia
CASE REPORT
A 68-year-old AfricaneAmerican male underwent
uncomplicated cataract extraction with posteriorchamber intraocular-lens placement in the right eye
(Steinle et al BJO 2012)
Downloaded from bjo.bmj.com on November 21, 2012 - Published by group.bmj.com
Innovations
Oral rifampin utilisation for the treatment of chronic
Figure 1 Fundus photographs
and fluorescein angiogram
(both serous
eyes). The photographs
reveal diffuse bilateral retinal
multifocal
central
retinopathy
pigment epithelium irregularities with patchy hyperpigmentation, while the fluorescein angiogram reveals corresponding
diffuse retinal pigment epithelium decompensation with granular hyperfluorescence secondary to chronic central serous
Nathan C Steinle, Naina Gupta, Alex Yuan, Rishi P Singh
retinopathy.
10
Department of Ophthalmology,
Cole Eye Institute, Cleveland
Clinic Foundation, Cleveland,
Ohio, USA
Br J Ophthalmol 2012;96:10e13. doi:10.1136/bjophthalmol-2011-300183
on 12 May 2008. Because of the lack of the anticiABSTRACT
pated visual acuity improvement following cataract
Chronic central serous retinopathy (CSR) is characterised
surgery, the patient was referred to a retina
by frequent exacerbations and a poor visual prognosis.
specialist for further evaluation.
Very few therapies exist for chronic CSR, and the
RIFAMPICINA (RIFADIN)
Dosaggio
300 mg 2 volte al giorno
Effetti collaterali
Rash cutaneo
Anoressia
Sintomi influenzali
Colorazione rossastra urine, saliva e lacrime (lac)
Aumento enzimi epatici
Esami da richiedere prima
Enzimi epatici (SGPT e SGOT)
Bilirubina
Creatinina serica
Emocromo
RIFAMPICINA (RIFADIN)
Dubbi
Solo 2 case reports
Per quanto tempo deve durare il
trattamento?
Effetti collaterali gravi (epatite,
shock anafilattico, insufficienza
renale, s. Steven-Johnson, etc)
KETOCONAZOLO (NIZORAL 200 mg)
Farmaco antimicotico usato per
terapia micosi orali e come
shampoo anticalvizie
Razionale
Inibisce sintesi steroidi
Utilizzato per ridurre i livelli di cortisolo
endogeno nel Cushing al dosaggio di 600
mg/die (Loli et al. J Clin Endocrinol Metab 1986)
KETOCONAZOLO (NIZORAL 200 mg)
Acta Ophthalmologica 2010
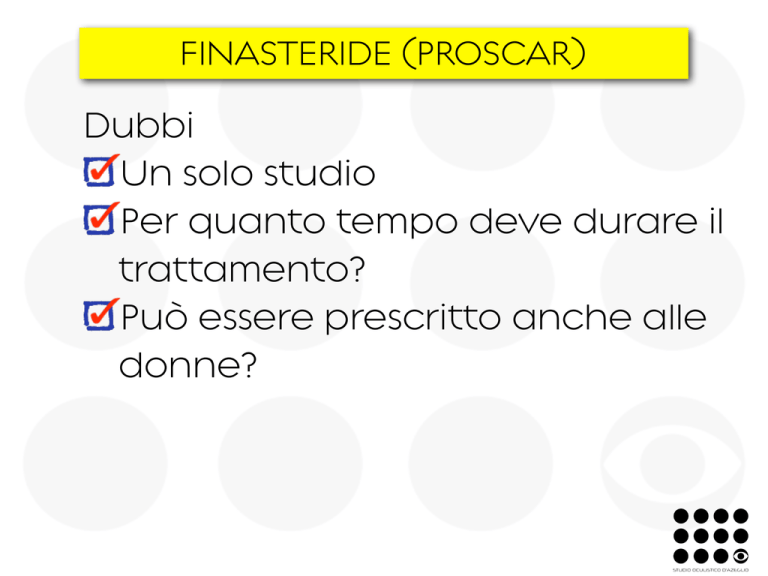
Fig. 1. Ketoconazole blocks P450scc and 11b-hydroxylase, thus leading to reduced synthesis of
pregnenolone and cortisol.
KETOCONAZOLO (NIZORAL 200 mg)
2 studi
Acta Ophthalmologica 2010
KETOCONAZOLE IN THE TREATMENT
OF CHRONIC IDIOPATHIC CENTRAL
SEROUS CHORIORETINOPATHY
CATHERINE B. MEYERLE, MD, K. BAILEY FREUND, MD,
PAWAN BHATNAGAR, MD, VIRAL SHAH, MD,
LAWRENCE A. YANNUZZI, MD
Purpose: To determine the effect of an adrenocorticoid antagonist (ketoconazole) in the
treatment of patients with central serous chorioretinopathy (CSC).
Methods: Ketoconazole was given at an oral dose of 600 mg per day for 4 weeks.
Laboratory monitoring included 24-hour urinary cortisol and liver function tests at baseline,
4 weeks, and 8 weeks. Changes in greatest linear dimension were followed with fluorescein
angiography at baseline, 4 weeks, and 8 weeks. Posterior pole anatomy was assessed with
optical coherence tomography at baseline, 4 weeks, and 8 weeks. Ophthalmic examination
and best-corrected visual acuity were assessed at each interval visit.
Results: Median visual acuity in the study eye remained stable at 20/40 throughout the
8-week follow-up. Median lesion height and greatest linear dimension were stable at 4
weeks and decreased at 8 weeks.
Conclusion: Ketoconazole lowered endogenous cortisol after 4 weeks of 600 mg daily.
While median visual acuity, lesion height, and greatest linear dimension remained unchanged during the month of drug treatment, there may have been a delayed therapeutic
response seen at 8 weeks.
RETINA 27:943–946, 2007
B
600 mg/die x un mese
Stabilità ad un mese,
miglioramento a 2 mesi
No gruppo di controllo
oth endogenous and exogenous corticosteroids
have been implicated in central serous chorioretinopathy (CSC). Many studies have confirmed that
exogenous steroid administration is a risk factor for
the development of CSC.1–3 Multiple routes of corticosteroid administration have been implicated in CSC
pathogenesis including oral, intravenous, inhaled, intranasal, intramuscular, and topical dermatologic.4 –10
There have even been isolated case reports of CSC
following vitrectomy with intravitreal triamcinolone
From the LuEsther T. Mertz Retinal Research Center/Manhattan
Eye, Ear & Throat Hospital, New York, and Vitreous-RetinaMacula Consultants of New York, New York.
This work was supported by The Macula Foundation, Inc.
The authors have no financial interest in any aspect of the article.
acetonide for diabetic macular edema11 and CSC after
a periocular steroid injection for iritis.12
Endogenous corticosteroids secreted by the cortex
of the adrenal glands are also thought to contribute to
the pathogenesis of disease. Bouzas and colleagues
reported the development of CSC in endogenous
Cushing disease.13 Other risk factors, such as pregnancy and stress, are associated with hypercortisolism.13,14 Many CSC patients have elevated 24-hour
urine corticosteroids or plasma cortisol.15,16
Based on the documented association of hypercortisolism with CSC, Jampol and colleagues proposed
treatment for chronic cases aimed at lowering endogenous cortisol levels.16 The suggested therapeutic
strategy involved corticosteroid antagonists such as
Ketoconazole in the treatment of
central serous chorioretinopathy:
a pilot study
Azadeh Golshahi,1 Dietrich Klingmüller,2 Frank G. Holz1 and
Nicole Eter1
1
Department of Ophthalmology, University of Bonn, Bonn, Germany
Institute of Clinical Biochemistry, University of Bonn, Bonn, Germany
2
ABSTRACT.
Purpose: The aim of this study was to evaluate a possible effect of systemic
ketoconazole on visual acuity (VA) and retinal thickness in patients with acute
central serous chorioretinopathy (CSCR).
Methods: Fifteen consecutive patients were treated with ketoconazole
200 mg ⁄ day for a period of 4 weeks. Another 15 patients served as a control
group. Baseline examination and review after 4 weeks included VA testing and
measurement of neuroretinal or pigment epithelial detachment by optical
coherence tomography (OCT). Fluorescein angiography was performed to verify the diagnosis.
Results: At baseline, mean VA in Snellen units was 0.6 ± 0.2 (logMAR
0.2 ± 0.7) in the treatment group and 0.7 ± 0.3 (logMAR 0.2 ± 0.5) in the
control group. On OCT, mean neuroretinal or pigment epithelial detachment
measured 288 ± 163 lm in the ketoconazole group and 225 ± 51 lm in the
control group, respectively. Four weeks later, mean VA improved in both
groups. On OCT, neuroretinal or pigment epithelial detachment decreased in
both the treatment and control groups. The differences were not statistically
significant.
Conclusions: Although a pharmacological decrease in endogenous cortisol synthesis appears to be a rational approach in the treatment of CSCR, systemic
ketoconazole at 200 mg ⁄ day was not associated with a significantly better outcome in this preliminary study.
Localized impairment of metabo
transport functions of the RPE, lea
ing to a reversal of the direction
ion secretion, has also been suggest
(Spitznas 1986). The common fin
pathway results in an accumulation
extracellular fluid in the subretin
and ⁄ or sub-RPE space.
Central serous chorioretinopathy
a disease characterized by sero
detachment of the neurosensory reti
secondary to one or more focal lesio
of the RPE. It afflicts young and m
dle-aged adults and concerns mo
men than women. Symptoms are bl
ring of vision (usually unilaterall
metamorphopsia, micropsia, relat
scotoma and colour desaturati
(Bennett 1955; Gass 1967; Wang et
2008). The condition is subdivid
into acute and chronic types. Acu
CSCR appears predominantly
young people and shows characteris
changes starting with a focal po
and resulting in an accumulation
200 mg/die
Miglioramento ad un
mese, ma non rispetto a
gruppo di controllo
Key words: central serous chorioretinopathy – CSC – CSCR – corticosteroids – ketoconazole
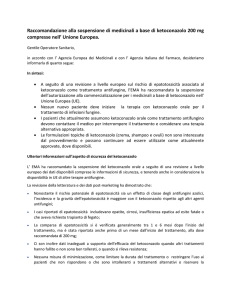
KETOCONAZOLO (NIZORAL 200 mg)
Dosaggio
600 mg/die per almeno un mese
Effetti collaterali
Epatotossicità, ginecomastia
Esami da richiedere prima
Funzionalità epatica
KETOCONAZOLO (NIZORAL 200 mg)
Interazioni farmacologiche
nifedipina e chinidina: effetto antiipertensivo intensificato
da ketoconazolo
rifampicina e isoniazide: riducono i livelli ematici di
ketoconazolo
antiacidi anti H2: inibiscono l’assorbimento di ketoconazolo
farmaci con metabolismo citocromo-dipendente:
anticoagulanti orali, digossina, ciclosporina, metilprednisone,
midazolam, ecc.
KETOCONAZOLO (NIZORAL 200 mg)
Dubbi
Dosaggi >200 mg sono tossici?
Un mese di terapia a 600 mg è
troppo breve?
Ancora scarsa evidenza e no
studi con gruppo di controllo
Terapia per tutti i pazienti con
CRSC cronica? O solo per quelli
con ipercortisolismo?