UNIVERSITY OF MESSINA
Department of Urology
School of Medicine
Chairman: Prof. Giuseppe Morgia
Prostatitis and BPH:
myth or real evolution ?
Introduction
•What is the BPH ?
•What is the prostatitis ?
Introduction
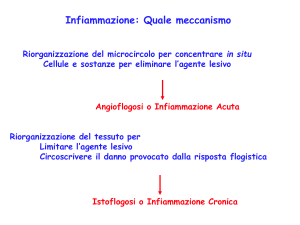
A causative role for inflammation in the pathogenesis of BPH was first
proposed by Moore RA in 1937 but for the major part of the 20th
century the “embryonal reawakening theory” dominated the field of
BPH
Recent studies assessed a strong relationship between Prostatitis and
Benign Prostatic Hyperplasia (BPH)
Flogosis could play a relevant role in the prostatic diseases progression
Today investigations of
experimentally induced
prostatitis in mice and rats
suggest that BPH is an
immune-mediated inflammatory
disease
BPH/PROSTATITIS
Traditionally, prostatitis has been considered a condition which affects
younger men but little attention has been given to the association
BPH/Prostatitis despite the high prevalence of both condition in ageing men
Nickel reported that approximately 8% of men over 50 years suffer with
some mild prostatitis like symptoms vs 11% of younger men.
5053 pts with prostatitis of which 57,2% + BPH
31681 pts
Collins MM et al J Urol 2002
7465 pts with BPH of which 38,7% + prostatitis
BPH/PROSTATITIS
Almost all surgery-derived BPH specimens show inflammatory
infiltrates at histologic examination
Even if there is a lack of association of histological prostatitis and
clinical prostatitis,the importance of inflammation, for years was
undervalued
Inflammatory
infiltrates were
always considered
of no clinical
relevance
BPH/PROSTATITIS
70% T
lymphocytes
Mean 28 fold increasing of Tcells infiltrates with ageing in
typical BPH
15% B cells
Contestually reversed ratio
between CD8
cytotossic/suppressor to CD4
helper T cells
15%macrophages
and mast cells
Increased presence may be
promoted by down-regulation
of the MIC-1 (macrophage
inhibitory cytokine 1) which is
suppressed in BPH tissues
Agenda
• Association of inflammation and
clinical BPH
• Role of inflammation in the
pathogenesis of BPH
• Flogosis and BPH progression
• Flogosis and BPH treatment
• Biomarkers of inflammation for BPH
Association of inflammation and
clinical BPH
This relationship has been observed by Di Silverio et al. in a study
conducted over 3942 histologic specimens of pts affected by BPH
No Flogosis
Flogosis
43%
57%
30%
chronic flogosis
Di Silverio Eur Urol 2003
REDUCE
REduction by DUtasteride of prostate Cancer Events
It was performed an additional
investigation from the actually
available data
Evaluation of the
baseline relationship
between histologic
prostate inflammation
and LUTS
Histologic flogosis
was detected in 78%
of men
Weak but statistically
significant correlation with
IPSS
REDUCE
REduction by DUtasteride of prostate Cancer Events
REDUCE: 5,597 pz
Conferma istopatologica di flogosi nel 94.5%
• Cronica: 78%
• Acuta: 16.5% (grado medio)
Nessuna correlazione tra:
Stato infiammatorio acuto e CPSI score
Correlazione statisticamente significativa:
Stato infiammatorio cronico e CPSI score
Nickel – J Urol 2007
Classificazione isto-patologica della flogosi prostatica
Localizzazione
anatomica
Pattern istologico
Ghiandolare
Infiltrato infiammatorio all’interno dei dotti/epitelio ghiandolare e/o
del lume
Perighiandolare
Infiltrato inf. nello stroma attorno ai dotti o acini (distanza<50µm)
Stromale
Infiltrato inf. nello stroma e comunque ad una distanza>50 µm
Estensione
Percentuale di tessuto coinvolta dagli infiltrati infiammatori
Focale
<10%
Multifocale
10-50%
Diffusa
>50%
Grado
Descrizione morfologica (densità delle cell.
Infiammatorie/mm2)
1 o Modesto
Cellule infiammatorie isolate (<100)
2 o Moderato
Aggregati di cell. Infiammatorie senza distruzione tissutale o
formazione di noduli/follicoli linfatici (100-500)
3 o Severo
Aggregati di cell. Infiammatorie con distruzione tissutale o
formazione di noduli/follicoli linfatici (>500)
Irani et al – J Urol 1997
Consensus Conference – Nickel 2001
REDUCE
REduction by DUtasteride of prostate Cancer Events
Histologic evaluation was performed using a classification proposed by a
central laboratory (Bostwick Laboratories Richmond, VA, USA)
Graded average acute and chronic inflammation based on a 4-point scale
I
II
III
Scale based on average cell density and
extent of tissue involvement
IV
Valutazione istopatologica prostatica su 167 autopsie:
BPH: 56%
PC: 29%
Flogosi: 67.6% (A 4%, C 53%, A+C 11%)
BPH + FC: 75%
No BPH + FC: 50% (p<0.01)
PC + FC: 55%
No PC + FC: 58% (p>0.1)
Nessuna correlazione tra FA e BPH/PC
Delongchamps et al, J Urol 2008
C+A
A
75%
55%
K + CF K
cronic
BPH + CF
BPH
113 (67,6%)
Delongchamps et al, J Urol 2008
Esistono segni clinici e parametri di
laboratorio che possono aiutare
l’individuazione dell’infiammazione ?
Esami clinici
• DRE
• TRUS con ecocolor doppler
– Scintigrafia con leuco In111 (non praticabile
routinariamente)
Esistono segni clinici e parametri di
laboratorio che possono aiutare
l’individuazione dell’infiammazione ?
Esami di laboratorio
• Esame urine e liquido seminale
– Dosaggio di citochine e chemichine (IL-1,IL-6,
IL-8, TNF α (non praticabili routinariamente)
– Dosaggio PGE-2, CRFR2 (nel tessuto) (non
praticabili routinariamente)
Role of inflammation in the
pathogenesis of BPH
BPH nodules are frequently composed by chronic inflammatory
infiltrates mainly represented by activated T-cells and macrophages
Why the leucocyte population increases in BPH ?
Several hypotheses have been generated based on
recent basic research
Role of inflammation in the
pathogenesis of BPH
After a probably primary injury it occurs an age dependent weakening of a
postulated population of suppressor cells that actively supresses the recognition
of prostatic agents which leads to gradual infiltration of the prostate by
lymphocytes and subsequent cascade of events that leads to BPH
Kramer G. Eur Urol 2007
Role of inflammation in the
pathogenesis of BPH
Flogosis
Increeased leucocyte population
IL-2; IL-6; IL-8; IL-17; IFN-γ
Perpetuate
chronic immune response
autoimmune
loop
Cox-2
Fibromuscolar Growth
Paracrine
loop
Role of inflammation in the
pathogenesis of BPH
Increased production of
IL-6; IL-8; IL-17
Immigration of T-cells into the area
Surrounding cells become targets
and are Killed
Vacant spaces replaced
by fibromuscolar nodes
Role of inflammation in the
pathogenesis of BPH
• Le cellule T CD4+ attivate secernono IL-17, una citochina
capace di stimolare le cellule epiteliali, endoteliali e
fibroblastiche di produrre diverse molecole pro-infiammatorie
come IL-1β, TNF-a, IL-8 e COX-2 (Steiner et al, Prostate
2003).
• Questi autori hanno dimostrato che il tessuto prostatico sano
non esprime IL-17, che però risulta elevato nelle cellule
muscolari liscie e nella parte apicale dei dotti epiteliali nella
IPB.
• Inoltre hanno dimostrato che il IL-17 aumenta la secrezione di
altre citochine pro-infiammatorie come IL-8, IL-6 e TGF- β.
• IL-8 e IL-6 sono 2 potenti fattori di crescita per le cellule
prostatiche epiteliali e stromali.
• Questi dati suggeriscono che l’IL-17 gioca un ruolo
fondamentale nel processo infiammatorio presente in pz con
IPB, essendo la principale citochina proinfiammatoria e
promuovendo una cascata di altre molecole proinfiammatorie.
Role of inflammation in the
pathogenesis of BPH
• Castro et al hanno dimostrato che le cellule
senescenti dell’epitelio prostatico secernono
FGF mediato dall’IL-8 e IL-1a.
• Le citochine proinfiammatorie inoltre inducono
l’espressione di COX-2. Wang et al hanno
dimostrato che le cellule che esprimono il COX-2
hanno un ritmo di proliferazione più alto e
determinano la up-regulation del gene
antiapoptotico Bcl2, offrendo così ulteriori
correlazioni fra infiammazione, apoptosi e
squilibrio nella crescita prostatica.
Inflammation and prostatic disease
Flogosis
BPH
Prostatitis
Oxidative Stress
PIA (Proliferative Inflammatory Atrophy)
HG PIN (High Grade Prostatic Intraepithelial Neoplasia)
Montorsi Arch It Urol Androl 2008
Prostatic
Cancer
Flogosis/BPH Progression
Does intraprostatic inflammation have a role in the pathogenesis
and progression of benign prostatic hyperplasia?
Mishra VC BJU Int 2007
Objective: to compare the incidence of acute and/or chronic
intraprostatic inflammation (ACI) in men undergoing TURP
for urinary retention and LUTS
374 pts
(TURP)
70% ACI
for AR
40% ACI
for LUTS
Conclusions: the risk of urinary retention due to BPH was
significantly greater in men with ACI than in those without,
and the association of TURP for retention with ACI was
stronger than that with prostate weight
Flogosis/BPH Progression
Data from the MTOPS study
( Medical Therapies of Prostatic Symptoms)
Chronic
inflammatory
infiltrate was found
in 43% of the men
It was hypothesized that the presence of
histological inflammation may be a predictor of
BPH clinical progression
In terms of:
• Symptoms
• Acute Uinary Retention (AUR)
• BPH related surgery
Flogosis/BPH Progression
Data from the MTOPS study
( Medical Therapies of Prostatic Symptoms)
Patients in all groups (placebo, finasteride, doxazosin and doxazosin
+ finasteride) with inflammation were more likely to progress
clinically
No Inflammation
Overall clinical progression: 13,2%
3,9% BPH related surgery
No AUR
Chronic Inflammation
Overall clinical progression: 21%
7,3% BPH related surgery
Accounted for
every AUR
event
5,6% AUR
Flogosis/BPH Progression
Is the diagnosis of clinical prostatitis at a young age a
risk factor for development of later BPH?
St Sauver JL try to determine whether physician-diagnosed
prostatitis was associated with later development of
symptomatic BPH in a longitudinal, population-based
sample of 2447 men residing in Olmsted County, Minnesota
Physician diagnosed prostatitis was associated
with a 2.4 fold increased odds of later onset of
several BPH-associated events
Prostatitis may therefore be an early
marker or a risk factor for
development of later prostatic or
urologic problems
St Sauver JL Urology 2008
Flogosis/BPH Treatment
Anti-inflammatory agents should be investigated as new
targets for the treatment of BPH?
Benign prostatic hyperplasia cell line viability and modulation of jm-27 by
doxazosin and Ibuprofen
Minnery CH J Urol 2005
Doxazosin + Ibuprofen
• Significantly decreased of cell
viability and induced apoptosis
in BPH prostate lines
• Decreased expression of JM-27
Protein highly up-regulated in
symptomatic BPH
Flogosis/BPH Treatment
Combination therapy with rofecoxib and finasteride in the treatment of men
with lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia
(BPH).
Di Silverio F Eur Urol 2005
Assumption of the study: Cyclooxygenase-2 (COX-2) is expressed
in human BPH tissue and displays either a pro-inflammatory effect
or a proliferative effect on prostate cells
46 pts
(LUTS + BPH)
Group A
Finasteride 5 mg/day
Group B
Randomized
Finasteride 5 mg/day +
Rofecoxib 25 mg/day
Flogosis/BPH Treatment
Combination therapy with rofecoxib and finasteride in the treatment of men
with lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia
(BPH).
Di Silverio F Eur Urol 2005
1 Month outcomes
Group A
Group B
0%
IPSS reduction > 4 points
34,7%
0%
Qmax > 3 ml/sec
8,7%
6 Months Outcomes: Differences between two groups were no significant
It was hypothesized that the
association of the drugs induced a
more rapid improvement until the
effect of finasteride becomes
predominant
Biomarkers for inflammation in BPH
If inflammation is associated with the pathogenesis,
symptoms and progression of BPH
Identification of specific Biomarkers
would be desirable
There are several candidates and many others
are currently being assessed by international
research group
These markers are generally nonspecific for prostate or BPH
They could be useful to stratify pts according to the risk of developing
BPH, to monitor symptoms and response to medical therapy
Biomarkers for inflammation in BPH
Malondialdehyde in benign prostate hypertrophy: a useful marker?
Merendino RA Mediators Inflamm 2003
44 pts
22 pts BPH
22 pts control
Measurement of serum malondialdehyde (MDA),
an index of inflammation and oxidative stress
Increased levels in the BPH pts and
positive correlation with PSA
Biomarkers for inflammation in BPH
Serum C-reactive protein concentration and lower urinary tract
symptoms in older men in the Third National Health and Nutrition
Examination Survey (NHANES III)
Rohrmann S Prostate 2005
2337 men
LUTS and BPH
Assessment of Symptoms and serum C- reactive
protein concentration measurement
0,32 mg/dl
Men without symptoms, no surgery
0,35 mg/dl
Men with three or four symptoms
0,36 mg/dl
Men with one or two symptoms
Men with
C-Reactive protein
> 3 mg/dl were
1.47 times more
likely to have 3 or
more symptoms
Biomarkers for inflammation in BPH
Seminal plasma cytokines and chemokines in prostate inflammation:
interleukin 8 as a predictive biomarker in chronic prostatitis/chronic
pelvic pain syndrome and benign prostatic hyperplasia
Penna G Eur Urol 2007
31 men
(CP/CPPS IIIB)
83 patients
20 men (controls)
9 men
(CP/CPPS IIIA)
23 men (BPH)
Were evaluated seminal plasma levels of 8
cytokines and 9 chemokins
Significantly increased levels of cytokines (IL1alpha, IL-1beta, IL-6, IL-10, IL12p70) and
chemokines (CCL1, CCL3, CCL4, CCL17,
CCL22, CXCL8/IL-8) were observed in
seminal plasmas from patients with CP/CPPS
or BPH. However, only IL-8 was significantly
elevated compared to controls in patients
with CP/CPPS IIIA - IIIB and BPH
IL-8 appears to be the
most reliable and
predictive surrogate
marker to diagnose
prostate inflammatory
conditions, such as
CP/CPPS and BPH
Conclusions
•Futher investigations about the role of inflammation in BPH will
expand our understanding of BPH pathogenesis, its histological
and clinical progression, allow risk stratification and suggest
novel treatent strategies
•Inflammation in the prostate gland appears to be more closely
related to BPH than the clinical syndrome chronic prostatitis
•In BPH enough evidence indicates that chronic immune
inflammation has a crucial role in the development of the disease
•Undestarding the mechanisms of the dysregulated immune
pathways may help to design novel anti-immune inflamatory
drugs
EFFETTI FARMACOLOGICI DI SERENOA
REPENS PIU’ LICOPENE E SELENIO
(PROFLUSS®) NELLA FLOGOSI CRONICA
ASSOCIATA A BPH: STUDIO
MULTICENTRICO ITALIANO (PROFLUSS
GROUP)
SCHEDULA DEL PROTOCOLLO
VALUTAZIONE DELLA RISPOSTA
AL TRATTAMENTO
La valutazione immunoistochimica sarà
condotta per la ricerca di linfociti T e di
macrofagi utilizzando rispettivamente gli
anticorpi monoclonali CD20, CD3 e CD68.
Per ciascun preparato con colorazione
positiva si procederà
alla conta delle
cellule positive in tre campi con obiettivo
20x; il valore medio sarà considerato
espressione della densità di linfociti T, B e
macrofagi presenti nel preparato.