www.fisiokinesiterapia.biz
Retrovirus e cancerogenesi
HTLV-1 e HTLV-2
I retrovirus
•
1911: Virus del Sarcoma di Rous
Francis Peyton Rous (1879-1970)
•
1970: trascrittasi inversa
Fonti: La Placa, Principi di
Microbiologia Medica, X
Edizione. Esculapio Ed.
Rapporto virus-cellula
•Il rapporto virus-cellula infetta può sfociare in:
•una infezione citocida (malattia acuta)
•latente (malattia recidivante)
•persistente (malattia cronica)
Infezione citocida
Infezione latente
Infezione latente
In vitro
Il virus realizza
Il virus realizza un rapporto
un rapporto di parassitismo
di parassitismo controllato
controllato,
con continua produzione
che consente alle cellule
di antigeni virali.
non solo di sopravvivere,
Le lesioni cellulari
ma anche di duplicarsi
sono dovute
Il genoma virale può
ad azioni lesive
essere integrato
esercitate in tempi
con quello della cellula ospite.
più o meno lunghi
Inclusioni cellulari
Il virus permane nella
dalle risposte immunitarie
degenerazione spongiforme
cellula in forma criptica
dell’ospite
Degenerazione cellulare
In vivo
La produzione di malattia è un evento raro
Risposta cellulare
Risposta ospite
Lisi cellulare
Decesso
Formazione inclusi virali
Malattia
Trasformazione cellulare
Disfunzioni cellulari
Moltiplicazione virale
in assenza di lesioni
Ciclo abortivo
Infezione asintomatica
Esposizione
senza infezione
Esposizione
senza penetrazione
Concetto iceberg
Rapporto virus-cellula
•Il rapporto virus-cellula infetta può sfociare in:
•una infezione citocida (malattia acuta)
•latente (malattia recidivante)
•persistente (malattia cronica)
•trasformazione neoplastica
I virus oncogeni hanno la capacità di trasformare
(immortalizzare) cellule normali in colture in vitro,
bloccandone la differenziazione e
conferendo loro numerose proprietà della cellula neoplastica.
I virus oncogeni
•Virus in grado di indurre o di concorrere alla comparsa di alterazioni del ciclo
cellulare.
L’oncogenesi è un processo graduale: non sempre la formazione del tumore
rappresenta una inevitabile conseguenza dell’infezione virale.
L’oncogenesi prevede una serie di cambi indipendenti ma irreversibili che insieme
contribuiscono alla dis-regolazione della crescita tumorale. L’infezione virale
rappresenta uno di questi step. E solo se succedono altri eventi nella stessa cellula,
assisteremo allo sviluppo del cancro.
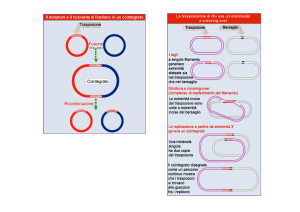
Oncogenesi virale: quali meccanismi?
I meccanismi con cui un virus provoca un tumore sono molto divergenti,
ma hanno tutti alcune caratteristiche in comune…
a) una singola particella virale è sufficiente per la trasformazione. Non è
necessaria una infezione multipla della stessa cellula.
b) tutto o parte del genoma persiste nella cellula trasformata. Comunque,
spesso non c’è produzione di progenie infettante.
c) in tutti i casi di trasformazione indotta del virus, almeno una parte del
genoma viene espresso nelle cellule trasformate
d) la trasformazione è il risultato della rottura dei segnali normali di
crescita cellulare.
Caratteristiche delle cellule neoplastiche
•
Immortalizzazione
•
Aumento dell'attività telomerasica: nella cellula normale la telomerasi è
repressa. La lunghezza del telomero è un orologio biologico, che ci dice
quanto la cellula può arrivare a vivere. Quando i telomeri sono troppo
corti, la cellula non è più in grado di replicarsi. La telomerasi è attiva
nelle cellule staminali
•
•
•
•
•
•
Mancanza della inibizione da contatto
Glicolisi aerobia aumentata (la produzione di ATP è aumentata)
Presentazione di nuovi antigeni (presenti solo nella vita fetale)
Genoma virale totalmente o parzialmente integrato
Produzione di proteine precoci
Corredo cromosomico alterato
Meccanismo dell’azione patogena
Oncogene (v-onc)
Protooncogeni (c-onc)
Sono pressoché identici ai geni
cellulari
Attivi durante il processo di
moltiplicazione e differenziazione
cellulare e cessano di funzionare nei
tessuti differenziati
I prodotti (proteine) intervengono
nelle varie fasi della mitosi cellulare
Sono sotto il controllo di antioncogeni o geni oncosoppressori
Meccanismo dell’azione patogena
Presenza di v-onc
Assenza di v-onc
Mancanza di controllo da parte di
anti-oncogeni o geni onco-soppressori
Il virus si integra vicino ad un
oncogene cellulare e ne induce la
trascrizione
oppure
influenzano negativamente la
funzione degli onco-soppressori
Aumentata proliferazione cellulare
Human pathogenic retroviruses
Lentivirinae
Human immunodeficiency virus type 1
Human immunodeficiency virus type 2
Oncovirinae
Human T-lymphotropic virus type 1 (HTLV-1)
Human T-lymphotropic virus type 2 (HTLV-2)
Human T-lymphotropic virus type 3 (HTLV-3) simian origin
Human T-lymphotropic virus type 4 (HTLV-4) no known primate counterpart
T-lymphotropic viruses
Human T-lymphotropic virus type 1 (HTLV-1) 1980
Human T-lymphotropic virus type 2 (HTLV-2) 1982
The long history of HTLV in human populations
Genetic heterogeneity and stability of the HTLV genome
Virus biology
The Associated diseases
Diagnosis
The long history of HTLV in human populations
The endemicity of HTLV-1 and HTLV-2 in some populations living in
remote areas of the globe, suggests the possibility that these viruses have
been infecting human since several thousands of years
oldest proto-Africans
Efe Mbuti Pygmies
The long history of HTLV in human populations
HTLV-1 and HTLV-2 infections among Pygmies are
ancient origin
result of more recent interspecies
transmission of STLVs:
jumping from primates to humans
STLV-1 infects most primate
species in Africa and Asia and
has been associated with
lymphoma and leukemia
PTLV-I: HTLV-1 and STLV-I
PTLV-II : HTLV-2/STLV-II
Stability of the HTLV genome
RNA viruses evolve at the rate of 10-3 to 10-5 nucleotide substitution per
site per year
but
HTLV-1 and HTLV-2 have a very stable genome
Why?
•
•
•
HTLVs are slowly replicating viruses
HTLV mutation rates are unusually low, due to a high fidelity reverse
transcriptase
After the integration in the host genome, HTLVs predominantly propagate as
proviral DNA during cellular mitosis using the host cell machinery.
HTLV-1 and 2 subtypes
•
•
•
•
HTLV-1a, the Cosmopolitan subtype,
joins strains from different
geographic regions
HTLV-1b, also known as Central
African subtype, joins strains
isolated from Central Africa
populations
HTLV-1c is the Melanesian subtype
to which belong the divergent strains
isolated in Papua New Guinea and
from Australian aboriginals
HTLV-1d has been recently
described as a new distinct molecular
subtype isolated from Cameroonian
pygmies and from an infected
Gabonese individual
•
•
•
HTLV-2 isolates: prevalent in
Southeastern Europe
HTLV-2a subtypes: prevalent in
Northern European IDUs, such as in
UK, Ireland and Sweden
HTLV-2b subtypes: isolated in
Florida, Panama, Colombia,
Argentina, Paraguay, Chile
Map of distribution of HTLV/STLV viral isolates of known geographic origin
HTLV-1
STLV-1
Slattery et al., 1999
HTLV-2
STLV-2
HTLVs Biology
HTLVs have a central icosahedral nucleocapsid surrounded by a
round shaped envelope and the virions are seen as spherical
particles of about 100 nm in diameter
HTLV 1 and 2: same genomic organization and up to 65-70% of nucleotide
similarity
The novel HTLV receptor
Endothelial
cells
GLUT1 glucose transporter
erythrocytes
Pericyte
Neuronal cells
Infection
Skeletal muscle cells
First step is the attachment of the virus to the cell surface through a specific
interaction between its envelope glycoproteins and a specific cell surface
receptor (GLUT1 glucose transporter)
Manel et al., Cell 2003
Glucose Transporter GLUT-1 and the paradox
The apparently restricted tropism of HTLV to T lymphocytes in infected
patients contrasts with the ability of the viral-encoded envelope
glycoprotein (Env) to bind to and direct entry into all vertebrate cell types
tested in vitro
In vitro
Several different cell types can be infected
In vivo
HTLV-1 and 2 can infect CD4+ and CD8+ T-cells
HTLV-1 primarily has a CD4+ tropism
HTLV-2 primarily has CD8+ tropism.
…….what happened during the first phase of infection?
Glucose Transporter GLUT-1
Envelope virus/GLUT interaction
inhibited glucose uptake and consumption
decreased lactate production and a drop in the acidification of the
extracellular milieu
GLUT-1 is not expressed on resting T lymphocytes whereas the GLUT 2-4
isoforms are present and GLUT-1 is induced upon immunological or
pharmacological activation.
1
2
Early after infection
Rapid and dramatic metabolic alterations
associated with decreased glucose
consumption. HTLV initially spreads with a
large tropism………..
3
In contrast, T lymphocytes that have a low
metabolic rate and as such are much less
dependent on glucose uptake, are more
likely to tolerate this effect and survive
infection.
the vast majority of cells that are
dependent on GLUT-1 activity
and concomitantly express the
HTLV envelope are rapidly
eliminated
tax
inhibition of
tumor suppressor
proteins
CREB, NF-KB, AP-1
Up-regulation of several
cytokines, cytokine receptor, and
induction of gene expression
(such as c-jun, API-1, c-Fra,
BCL-2)
Promotes viral transcription
Critical factors for
cancerogenesis
p53 repression
TGF-β inhibition
Cellular
proliferation
cytopenia
HTLV-1 Tax
tumor
Haematopoietic
precursors
TGF-β
stimulation
TGF-β
proliferation
TGF-β inhibition
HIV-Tat
The proliferation of infected cells is promoted by Tax expression
CTLs attack the Tax-expressing cells since Tax is their major target Rex, p30 and HBZ suppress Tax
expression.
Expansion of
infected CD4+ cells
Suppression of Tax
by Rex, p30 and
HBZ
ATL
Alterations of
HTLV-1 infected cells
Tax
genome
expression
Cell-to cell
transmission
Suppression of
Tax by CTL
On the other hand, loss of Tax expression is frequently observed in leukemic cells. Three mechanisms have been
identified for inactivation of Tax expression: 1) genetic changes of the tax gene (nonsense mutations, deletions or
insertions) 2) DNA methylation of the 5'-LTR and 3) deletion of the 5'-LTR
Loss of Tax expression gives ATL cells advantage for their survival since they can escape from CTLs.
Matsuoka et al. 2005
HTLV-1 and associated diseases
•
•
•
Adult T-cell Leukemia (ATL)
The lifetime risk of developing ALT in HTLV-1 seropositive individuals in
about 0.1% to 5%
The latency period is usually more than 20 years
ATL is classified in four clinical stages
Lymphoma
Smouldering
Chronic
Acute type
HTLV-1 and associated diseases
Tropical spastic paraparesis/HTLV associated myelopathy (TSP/HAM)
•
•
•
•
A slowly progressive myelopathy with spastic paraparesis of lower
extremities
Moreover…. variable peripheral sensory abnormalities, hyperreflexia,
bladder and bowel dysfunction, male impotence.
The lifetime risk of developing the disease in HTLV-1 seropositive
patients is less than 1%, with a mean age of onset of about 40 years
The incubation time can greatly vary and it can be as short as a few weeks
in patients who get the infection from blood transfusions.
HTLV-2 associated diseases
Firstly isolated from a patient with hairy-cell leukaemia
………………….
Most of the HTLV-2 infected individuals are asymptomatic during
their entire life.
Recently there have been increasing evidences that the infection
may be associated with neurological disorders
HTLV-2 RNA is found in HAM-like lesions of the central nervous
system
Moreover, an increased prevalence of infectious diseases, such as
pneumonia, minor fungal infection or kidney infection, has been
associated with the presence of HTLV-2
HTLV-2 is present at significant rate among injecting drug users
(IDUs) co-infected by HIV-1
HTLV-2 and human progenitor cells
No infection!
HTLV-2 Mo viral strain T cell derived
CD34
T cell
Apoptosis protection
CD34
CD34
CD34
by
enhancement of telomerase activity and the induction of bcl-2 expression
Casoli et al 1999; Re at al. 2000
HTLV-2 and HIV-1. Does an interaction exist?
• HTLV-II can interfere with the replicative potential of HIV-1 by upregulating viral suppressive CC-chemokines and, in particular, MIP1alpha.
•
HTLV-II can influence HIV replication, at least in vitro, via upregulation of HIV-suppressive chemokines
HTLV-2 and HIV-1. Does an interaction exist?
CD4
HIV-1
CTL
HTLV-2
CD8
CC-Chemokines (Mip1α, Mip1β, Rantes)
Spontaneous proliferation of T cell
•HTLV-II can interfere with the replicative potential of HIV-1 by up-regulating viral
suppressive CC-chemokines and, in particular, MIP-1alpha. …… HTLV-II can
influence HIV replication, at least in vitro, via up-regulation of HIV-suppressive
chemokines
HTLV-1 and 2: diagnosis of infection
•
•
•
Immunoenzymatic assay
Immunoblotting
Provirus detection (qualitative and/or quantitative PCR)
HTLV-1 and 2: diagnosis of infection
•
Immunoblotting: The first antibodies, which appeared within 2 months
after exposure, were directed against rgp21 and were followed by
antibodies to p24 and p19.
•
the Public Health Service Working Group has recommended that a serum
should be considered as HTLV-antibody positive when reactive to p24
and to gp46 or gp61/68
HTLV-1 and 2: diagnosis of infection
Blood donor screening for HTLV was introduced in:
•
•
•
1980s: first in Japan
1988 - 1989 in the United States and Canada
1991 in France
HTLV-1 and 2: diagnosis of infection
The prevalence of confirmed positive tests among tissue donors was
0.093 % for anti-HIV
0.229 % for HBsAg
1.091 % for anti-HCV
0.068 % for anti-HTLV
The estimated probability of viremia at the time of donation was
1 in 55,000 for anti-HIV
1 in 34,000 for HBsAg
1 in 42,000 for anti-HCV
1 in 128,000 for anti-HTLV
…………..the probability of collecting blood products from a viremic donor is extremely
low, it is not negligible.……………
An imported case of adult T cell leukemia in a HTLV-Iinfected patient, in Italy
•From an epidemiological point of view, it is important to report a case of
imported ATL in a non-endemic area, as it may explain the otherwise
untraceable origin of some rare and apparently autochthonous cases of ATL in
non-endemic areas ………………… Re et al. 2003 and 2004