LE NEOPLASIE DELLA
VESCICA
Normal Urothelium
• Normal urothelium consists of a flat mucosa lined by less
than approximately seven layers of urothelial cells covered
by an umbrella cell layer. There is no need to count the
number of cell layers in order to distinguish normal
urothelium from flat urothelial hyperplasia. Rather, only
overt thickening should be designated as hyperplasia. The
size of normal urothelial cells is approximately 3 times the
size of lymphocytes, which can almost always be found in
the underlying lamina propria. Flat lesions with benign
cytology and minimal disorder should not be designated as
mild dysplasia but rather as normal urothelium. Atypia in
umbrella cells should not be overdiagnosed as dysplasia or
CIS
UROTELIO NORMALE
Papillary Hyperplasia
• Papillary hyperplasia is characterized
by slight “tenting”, undulating, or an
elevated configuration of the
urothelium of varying thickness,
lacking nuclear atypia. The lesion
often has one or a few small, dilated
capillaries at its base but it lacks a
well-developed fibrovascular core.
IPERPLASIA PAPILLARE
Urothelial Papilloma
• Urothelial papilloma is defined as
discrete papillary growth with a
central fibrovascular cores lined by
urothelium of normal thickness and
cytology. There is no need for
counting the number of cell layers.
PAPILLOMA UROTELIALE
Papillary Urothelial Neoplasm of Low
Malignant Potential
• Papillary urothelial neoplasm of low malignant
potential is a papillary urothelial lesion with an
orderly arrangement of cells within papillae with
minimal architectural abnormalities and minimal
nuclear atypia irrespective of the number of cell
layers. The urothelium in papillary urothelial
neoplasms of low malignant potential is much
thicker than in papillomas and/or the nuclei are
significantly enlarged and somewhat
hyperchromatic. Mitotic figures are infrequent in
papillary urothelial neoplasms of low malignant
potential, and usually confined to the basal layer.
PUNLMP
• Queste lesioni sono ad un rischio un maggiore del papilloma di
recidivare o formare altre lesioni papillari.
• Queste nuove lesioni sono occasionalmente ad alto grado e
possono progredire.
PUNLMP
PUNLMP
PUNLMP
Low-grade Papillary Urothelial
Carcinoma
• Low-grade papillary urothelial carcinomas are
characterized by an overall orderly appearance but with
easily recognizable variation of architectural and or
cytologic features even at scanning magnification. Variation
of polarity and nuclear size, shape, and chromatin texture
comprise the minimal but definitive cytologic atypia. Mitotic
figures are infrequent and usually seen in the lower half,
but may be seen at any level of the urothelium. It is
important to recognize that there may be a spectrum of
cytologic and architectural abnormalities within a single
lesion, such that the entire lesion should be examined, with
the highest grade of abnormality noted.
LOW GRADE PAPILLARY UROTHELIAL
CARCINOMA
LG-papillare
High-grade Papillary Urothelial
Carcinoma
• High-grade papillary urothelial carcinomas are
characterized by a predominantly or totally disorderly
appearance at low magnification. The disorder results from
both architectural and cytologic abnormalities.
Architecturally, cells appear irregularly clustered and the
epithelium is disorganized. Cytologically, there is a
spectrum of pleomorphism ranging from moderate to
marked. The nuclear chromatin tends to be clumped and
nucleoli may be prominent. Mitotic figures, including
atypical forms, are frequently seen at all levels of the
urothelium. There is an option in the diagnosis of highgrade papillary urothelial carcinoma to comment on
whether there is marked nuclear anaplasia.
HG-papillare
HG-Papillare
HG-papillare
Flat Urothelial Hyperplasia
• Flat uothelial hyperplasia consists of a
markedly thickened mucosa without
cytological atypia. Rather than requiring a
specific number of cell layers, marked
thickening is needed to diagnose flat
hyperplasia. This lesion may be seen in
the flat mucosa adjacent to low-grade
papillary urothelial lesions. When seen by
itself there is no data suggesting that it
has any premalignant potential.
Iperplasia piatta
Reactive Urothelial Atypia
• Reactive (inflammatory) atypia consists of
nuclear abnormalities occurring in acutely or
chronically inflamed urothelium. In reactive
atypia, nuclei are uniformly enlarged and
vesicular, with central prominent nucleoli. Mitotic
figures may be frequent. A history of
instrumentation, stones, or therapy is often
present. In the absence of appreciable nuclear
hyperchromasia, pleomorphism, and irregularity
in the chromatin pattern, the lesion should not be
considered neoplastic.
Urothelial Atypia of Unknown
Significance
• In some cases it is difficult to differentiate
between reactive and neoplastic atypia. There
may be a greater degree of pleomorphism and/or
hyperchromatism out of proportion to the extent
of the inflammation, such that dysplasia can not
be ruled out with certainity. These cases should
be designated as "atypia of unknown
significance" so that the patients may be followed
more closely and re-evaluated once the
inflammation subsides.
Dysplasia
• Dysplastic urothelium has
appreciable cytologic and
architectural changes felt to be
preneoplastic, yet falling short of the
diagnostic threshold for carcinoma
in situ.
DISPLASIA
Carcinoma in situ
• Carcinoma in situ is a flat lesion of the urothelium
that is a documented precursor of invasive
cancer in some cases. The lesion is characterized
by the presence of cells with large, irregular,
hyperchromatic nuclei that may be either present
in the entire thickness of the epithelium or only
part of it. Mitotic activity is frequently observed,
often in the mid to upper urothelium. Carcinoma
in situ encompasses lesions which in the past
were designated as severe dysplasia or marked
atypia.
CIS
CIS
Carcinoma uroteliale infiltrante la
lamina propria
Carcinoma uroteliale infiltrante la
tonaca muscolare
Invasione endovascolare linfatica
• Montironi R, Lopez-Beltran A.
• The 2004 WHO classification of bladder
tumors: a summary and commentary.
• Int J Surg Pathol. 2005 Apr;13(2):143-53.
• Lopez-Beltran A, Luque RJ, Alvarez-Kindelan J,
Quintero A, Merlo F, Requena MJ, Montironi R.
• Prognostic Factors in Survival of Patients With Stage Ta
and T1 Bladder Urothelial Tumors The Role of G1-S
Modulators (p53, P21Waf1, p27Kip1, Cyclin D1, and Cyclin
D3), Proliferation Index and Clinicopathologic Parameters
• Am J Clin Pathol. 2004 Sep;122(3):444-52.
• Friedrich MG, Toma MI, Petri S, Cheng JC,
Hammerer P, Erbersdobler A, Huland H.
• Expression of Maspin in non-muscle invasive
bladder carcinoma: correlation with tumor
angiogenesis and prognosis.
• Eur Urol. 2004 Jun;45(6):737-43.
• Sugimoto S, Maass N, Takimoto Y, Sato K,
Minei S, Zhang M, Hoshikawa Y, Junemann
KP, Jonat W, Nagasaki K
• Expression and regulation of tumor
suppressor gene maspin in human bladder
cancer.
• Cancer Lett. 2004 Jan 20;203(2):209-15.
Papilloma uroteliale invertito
• Sebbene non faccia propriamente parte delle lesioni papillari
propriamente dette, questa entità condivide alcuni aspetti con il
papilloma esofitico. In alcuni casi ci sono aspetti ibridi in cui una quota
della lesione è costituita da una componente esofitica.
• In questi casi si dovrebbe classificare la lesione come papilloma con
aspetti endo-ed esofitici.
• Quando completamente escissa la lesione ha un basso rischio di
recidiva.
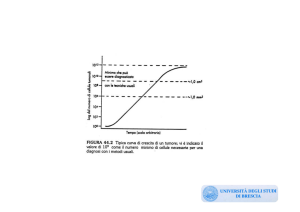
Percentuale di ricorrenza, progressione di grado, di stadio e sopravvivenza
tra le differenti categorie di carcinoma papillare non invasivo
Papilloma
Recidiva
0-8%
Progr-G
2%
Stage prog. 0%
Sopravv.
100%
PUNLMP
27-47%
11%
0-4%
93-100%
LG-PC
48-71%
7%
2-12%
82-96%
HG-PC
55-58%
not applicable
27-61%
74-90%
Neoplasie uroteliali invasive
• L’invasione della lamina propria è caratterizzata dalla presenza di nidi,
clusters o cellule uniche dentro la lamina propria; questa invasione può
essere associata ad una reazione di tipo desmoplastico dello stroma e
ad un infiltrato infiammatorio cospicuo.
• Nei carcinomi papillari di basso grado, si possono trovare dei nidi
cellulari di grandi dimensioni nella lamina propria, con disposizione a
palizzata degli elementi periferici, circondati da stroma, che
rappresentano un pattern di crescita invertito piuttosto che una
invasione.
Pattern di invasione della lamina propria
CIS con microinvasione: la microinvasione nel CIS è definita da
Farrow et al.(Clin Oncol 1982;1:609-14), come una componente
invasiva inferiore ai 5 mm in profondità. La microinvasione può
conferire a questi tumori la capacità di metastatizzare.
Pattern istologici di invasione nella lamina propria
•
•
•
•
-Carcinoma in situ con microinvasione
-Carcinoma papillare uroteliale con microinvasione
-Carcinoma papillare uroteliale con invasione dell’asse stromale
-Invasione certa della lamina propria
-invasione fino alla muscolaris mucosae
-invasione attraverso la muscolaris mucosae
-invasione della lamina propria non meglio precisata
• -Carcinoma uroteliale con patter di crescita endofitica o a fronte
ampio, con invasione stromale distruttiva
TNM
• I linfonodi regionali sono quelli della
piccola pelvi, vale a dire quelli al di sotto
della biforcazione delle arterie iliache
comuni.
• La lateralità non incide sulla classificazione
N.
TNM
•
•
•
•
Tx Tumore primitivo non definibile
T0 Tumore primitivo non evidenziabile
Ta Carcinoma papillare non invasivo
Tis Carcinoma in situ: “tumore piatto”
TNM
• T1 Tumore che invade il tessuto connettivo
sottoepiteliale
• T2 Tumore che invade la parete muscolare
•
T2a: invasione superficiale della parete
muscolare
•
T2b: invasione profonda della parete
muscolare
TMN
• T3 tumore che invade i tessuti perivescicali
•
T3a: Microscopicamente
•
T3b: Macroscopicamente (massa
extravescicale)
TNM
• T4 Tumore che invade qualsiasi delle
seguenti strutture: prostata, utero, vagina,
parete pelvica, parete addominale
•
T4a: tumore che invade prostata, utero,
vagina
•
T4b: tumore che invade la parete pelvica
o parete addominale
TNM
• Nx Linfonodi regionali non valutabili
• N0 Linfonodi regionali liberi da metastasi
• N1 Metastasi ad un singolo lnf della
dimensione massima di 2 cm
• N2 Metastasi in 1 o più lnf, delle
dimensioni comprese fra 2 e5 cm
• N3 Metastasi in 1 lnf della dimensione
massima superiore a 5 cm
TMN
• Mx Metastasi a distanza non accertabili
• M0 Metastasi a distanza assenti
• M1 Metastasi a distanza presenti
Raggruppamento in stadi
• Stadio I
• T1 N0 M0
Raggruppamento in stadi
• Stadio II
• T2a N0 M0
• T2b N0 M0
Raggruppamento in stadi
•
•
•
•
Stadio III
T3a N0 M0
T3b N0 M0
T4a N0 M0
Raggruppamento in stadi
•
•
•
•
Stadio IV
T4b N0 M0
Ogni T N1,N2,N3 M0
Ogni T ogni N M1