Vaccini
The eradication of smallpox by vaccination.
After a period of 3 years in which no cases of
smallpox were recorded, the World Health
Organization was able to announce in 1979 that
smallpox had been eradicated.
Adapted from Janeway et al., Immunobiology (2001)
Preclinical studies
In vitro Research
(5.000)
Animal models
Toxicology studies
(neck bottle)
Clinical Studies
Phase 1
Phase 2
Phase 3
Phase 4
GMP products
Vaccini preventivi
Vaccini terapeutici
Induzione della memoria
Efficacia e Sicurezza
patogeno extracellulare-risp B (IgG-IgA)
patogeno intracellulare-risp. CD8
Copertura:% della popolazione protetta (variazioni Ag <100%)
85-90% indiv non protetti riduce rischio infezioni
epitopi protettivi- valutazione in vitro e vivo
Sicurezza: dipende dal contesto- zone a rischio anche effetti collaterali
necessità di modelli preclinici
patogeni che non mutano sono + sicuri (morbillo)
al contrario quelli che mutano (HIV)
Tipi di vaccino
VACCINO ATTENUATO: stimola I.Inn e Adat. il microrg. replica Risp B e T
Buona immunità ma necessari richiami- costi mantenimento
Attenuazione per coltura in vitro o diverso ospite
Sistemi nuovi per attenuaz. per delezione di geni anziche mutazioni puntiformi
VACCINO UCCISO: raggi gamma o formalina (ag chimici), epitopi alterati?
Eliminata la virulenza; stabili; costi ridotti per mantenimento; piu richiami
necessari; bassa protezione batteri intracellulari; manca risposta CTL pres. B
TOSSOIDI: tossine chimicamente alterate (difterite, tetano, pertosse)
VACCINI A SUBUNITA: proteine e polisaccaridi- rischio ridotto
Proteine- x costi e difficoltà si usa DNA ric in E. coli; si puo aumentere la
immunogenicità; eliminati rischi di altre proteine; alterazioni proteiche con
perdita epitopi discontinui, quindi ass. risposta B ma CTL presente.
Polisaccaridi: facili da produrre, no effetti collaterali; sono T indipend. Scarsa o
nulla memoria, uso di carrier coniugato tipo TT.
Tipi di vaccino
PEPTIDi: sicuri, per assenza proteine tossiche; conservazione e trasporto
ideali
Stimolano molto CTL e CD4, poco B per assenza di epitopi conformazionali;
Utilizzo contemporaneo di molti peptidi, si possono ritagliare vaccini “su
misura” per popolazione dominante. Utili nel richiamo
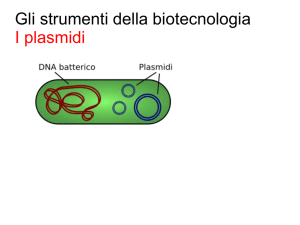
VACCINI A DNA per uso di vettori batterici o virali per introdurre DNA in
ospite, trascriverlo e tradurlo; DC infettate indotte in presentazione per via
endogena ed esogena; se rilasciato il prodotto stimola rispo B.
Vaccina virus: grande puo ospitare + geni di interesse;
Poliovirus: piccolo, ma infetta dotto gastrico;
Adenovirus: grande e facile da produrre.
Effetti indesiderati: si generano Abs anti vettore/uso peptidi o cambio vettore.
DNA NUDO: plasmide replicato in E.coli, purificato e inoculato in animali,
siringa, pistola o tramite elettroporatore.
Tumorigenesi per inserzione nel DNA ospite?!?
**Vaccini attenuati e vettori ricombinanti inducono risposta infiammatoria
adeguata
ADIUVANTI
Effetto deposito/ induzione molecole co-stimolatorie
Allume il solo ammesso per umano
Vettori di trasporto che proteggono l’antigene da proteasi e
nucleasi
Aumentano il numero di molecole da trasportare
Quali sono?: Liposomi= Ag + fosfolipidi, captate subito da DC.
Virosomi: virus + Ag
ISCOM: colesterolo, fosfolipidi e detergenti. VLPs
ALCUNI ESEMPI DI VACCINI PREVENTIVI
Vaccinazione per tossoidi: difterite, tetano e pertosse.
Vaccinazione per sub unità: HBV, Influenza, HPV
Vaccinazione attenuato: morbillo, parotite e rosolia
Vaccinazione con polisaccaridi: pneumococco, meningococco.
Vaccinazione con batteri vivi: nella Tubercolosi, il BCG.
Vaccination
Adaptive immunity to a specific
infectious agent can be achieved in
several ways.
One strategy is to deliberately
cause a mild infection with the
unmodified pathogen providing
protective immunity against the
infection without the risk of
significant disease.
This process is named vaccination
and consists in the administration
of antigens that stimulate an
immune response that confers
protection from the human disease.
Adapted from Janeway et al., Immunobiology (2001)
Relevant diseases for which effective
vaccines are not yet available
Data from WHO 2001
Viruses are traditionally attenuated by selecting for growth in
nonhuman cells. To produce an attenuated virus, the virus must first be
isolated by growing it in cultured human cells. The adaptation to growth in
cultured human cells can cause some attenuation in itself; the rubella
vaccine, for example, was made in this way. In general, however, the virus
is then adapted to growth in cells of a different species, until it grows only
poorly in human cells. The adaptation is a result of mutation, usually a
combination of several point mutations. It is usually hard to tell which of
the mutations in the genome of an attenuated viral stock are critical to
attenuation. An attenuated virus will grow poorly in the human host, and
will therefore produce immunity but not disease
Adapted from Janeway et al., Immunobiology (2001)
Attenuation can be achieved more
rapidly
and
reliably
with
recombinant DNA techniques. If a
gene in the virus that is required for
virulence but not for growth or
immunogenicity can be identified,
this gene can be either multiply
mutated (left lower panel) or deleted
from the genome (right lower panel)
by using recombinant DNA
techniques. This procedure creates
an avirulent (nonpathogenic) virus
that can be used as a vaccine. The
mutations in the virulence gene are
usually large, so that it is very
difficult for the virus to revert to the
wild type.
Adapted from Janeway et al., Immunobiology (2001)
DNA vaccination by injection of DNA encoding a protective antigen and
cytokines directly into muscle. Influenza hemagglutinin contains both Band T-cell epitopes. When a DNA plasmid containing the gene for
hemagglutinin is injected directly into muscle, an influenza-specific immune
response consisting of both antibody and cytotoxic CD8 T cells results. The
response can be enhanced by including a plasmid encoding GM-CSF in the
injection. The plasmid DNAs are presumably expressed by some of the cells
in the muscle tissue into which they are injected, provoking an immune
response that involves both antibody and cytotoxic T cells. The details of
this process are not yet understood.
Adapted from Janeway et al., Immunobiology (2001)
Type of vaccines
Immunogenicity
Live classical:
-viral
-bacterial
Live recombinant:
-viral
-bacterial
Subunit/Inactivated:
-whole pathogen
-protein
-peptide
-polysaccaride
cDNA based
Safety and
use of relevant epitopes
Rappuoli R. Curr Opin Microbiol 2000
Rappuoli R. Curr Opin Microbiol 2000
INNATE IMMUNITY
ACQUIRED IMMUNITY
BCG
Peptides
CpG
Hsp Phoshoantigens
Selected
HIV-peptides
+
& Glycolipids
Monocytes/Dendritic cells
CD4 T helper
CD8
CTL
gd T cells
B
cells
ab CD1-T cells
Innate antiviral response:
- Th1 cytokines
- Chemokines/CAF
- NK-like cytotoxicity
Co-stimulation
Acquired antiviral response:
- HIV-neutralising IgA
- HIV specific CTL
ISCOMs can be used to deliver peptides to the MHC class I processing
pathway. ISCOMs (immune stimulatory complexes) are lipid micelles that
will fuse with cell membranes. Peptides trapped in ISCOMs can be
delivered to the cytosol of an antigen-presenting cell (APC), allowing the
peptide to be transported into the endoplasmic reticulum, where it can be
bound by newly synthesized MHC class I molecules and hence transported
to the cell surface as peptide:MHC class I complexes. This is a possible
means for delivering vaccine peptides to activate CD8 cytotoxic T cells.
ISCOMs can also be used to deliver proteins to the cytosol of other types of
cell, where they can be processed and presented as though they were a
protein produced by the cell.
Adapted from Janeway et al., Immunobiology (2001)
TIPI DI VACCINO
PROGRAMMA VACCINAZIONI
VACCINI TERAPEUTICI
EFFETTI COLLATERALI
ESEMPI

![Lezione 15 Virus [modalità compatibilità]](http://s1.studylibit.com/store/data/000771737_1-84b1cca561c5813066d1b76125338a98-300x300.png)

![mutazioni genetiche [al DNA] effetti evolutivi [fetali] effetti tardivi](http://s1.studylibit.com/store/data/004205334_1-d8ada56ee9f5184276979f04a9a248a9-300x300.png)