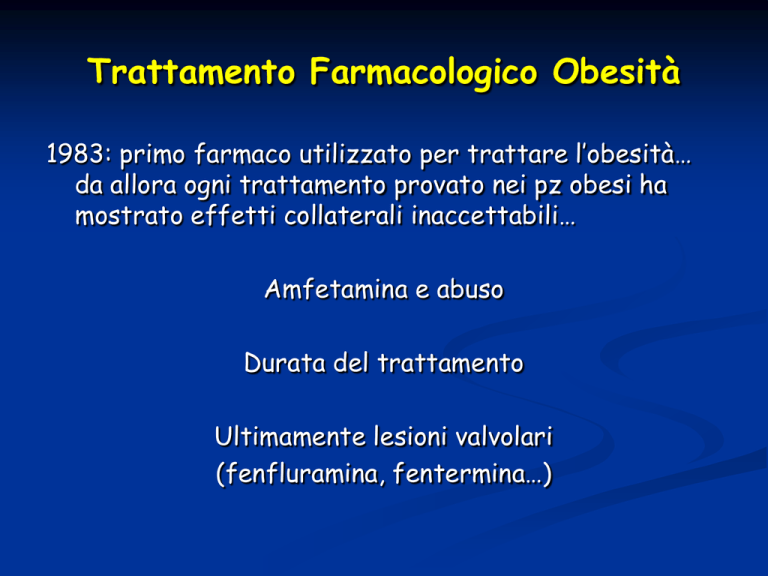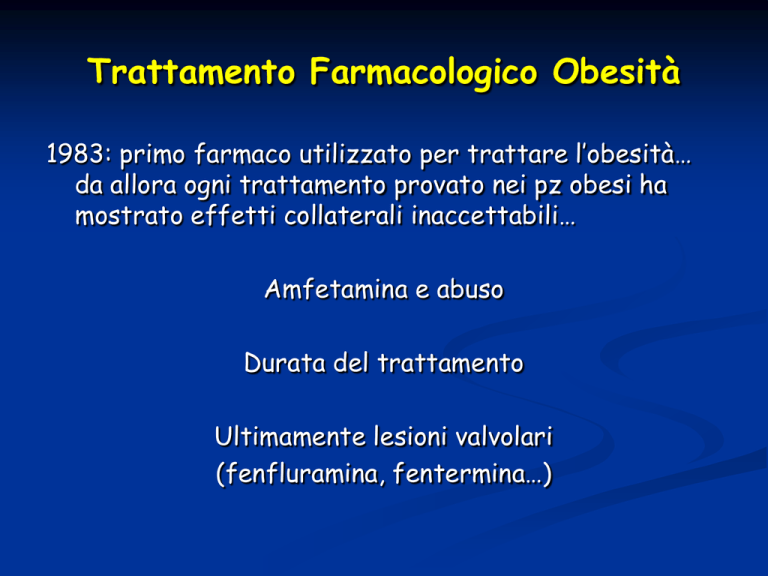
Trattamento Farmacologico Obesità
1983: primo farmaco utilizzato per trattare l’obesità…
da allora ogni trattamento provato nei pz obesi ha
mostrato effetti collaterali inaccettabili…
Amfetamina e abuso
Durata del trattamento
Ultimamente lesioni valvolari
(fenfluramina, fentermina…)
Meccanismi per il trattamento
dell’obesità
Riduzione del food intake
Alterazione assorbimento e/o
metabolismo
Farmaci che aumentano il metabolismo
Efedrina + caffeina
FDA approval, but not for obesity
Beta3 agonists in sviluppo
Farmaci che alterano assorbimento e/o
metabolismo
Orlistat è l’unico farmaco approvato da FDA per il
trattamento dell’obesità
Inibitore delle lipasi pancreatiche
Effetto dose dipendente: scarsi effetti in diete low-fat
Riduzione colesterolo, ma integrare vit liposolubili
Orlistat non è assorbito
Peptidi e food intake
Leptina
Assenza peptide = ob/ob
Assenza recettore = db/db
NPY
Y1 & Y5 antagonists
CCK
Peptide analogs
Metabolism inhibitors
Glucagone
GLP-1
Farmaci che riducono il food intake
Simpaticomimetici
Buon assorbimento orale
Emivita breve (unica eccezione sibutramina)
Effetti collaterali: secchezza fauci, costipazione,
astenia, insonnia.
Addictive properties?
Attenzione cardiovascolare
Associazione
fenfluramina /fentermina
1996: > 18M prescrizioni
Bupropion/Naltrexone (marketed as ContraveVR ). Bupropion/naltrexone was FDA approved
for weight loss in September 2014(26). Bupropion’s primary mechanism of action is via
dopaminergic and noradrenergic stimuli without inhibition of monoamine-oxidase (MAO) or
reuptake of serotonin. Inhibiting reuptake of dopamine and/or norepinephrine decreases the
“reward pathway” that various foods can induce. The second component of ContraveVR is
naltrexone, which is a pure opioid antagonist and blocks an opioid pathway that may slow weight
loss. Four 56-week multicenter, double-blind, placebo-controlled trials (CONTRAVEVR Obesity
Research, or CORI, COR-II, COR-BMOD, and COR-Diabetes) were conducted to evaluate the
effect of bupropion/naltrexone in conjunction with lifestyle modification in a placebo-controlled
cohort of 4536 patients. The COR-I, COR-II, and COR-BMOD trials enrolled patients with
BMI 30 kg/m2 or greater or overweight (BMI 27 kg/m2 or greater) and at least one comorbidity
(27-29). The COR-Diabetes trial enrolled patients with BMI greater than 27 kg/m2 with type 2
diabetes with or without hypertension and/or dyslipidemia. The primary endpoints were percent
change from baseline body weight and the proportion of patients achieving at least a 5%
reduction in body weight. In the 56-week COR-I trial, the mean change in body weight was
25.4% in patients assigned to bupropion/naltrexone 360/32 mg compared with 21.3% in the
placebo group. The clinically significant cut off of 5% reduction in body weight from baseline
occurred in 42% of treatment group patients vs. 17% of placebo patients (26).
In the COR-Diabetes trial, 44.5% of patients receiving bupropion/naltrexone lost 5% of their
body weight after 56 weeks vs. 18.9% of patients on placebo (P < .001) (30). Patients using
bupropion/naltrexone also showed a 0.6% reduction in HbA1c from baseline, compared to a
0.1% reduction in placebo. In all of the COR trials, secondary cardiovascular endpoints were
met, including statistically significant improvements in waist circumference (WC), visceral fat,
HDL cholesterol, and triglycerides (31).
Phentermine/Topiramate. Low-dose, controlled-release phentermine plus topiramate (as one
capsule) was approved by the FDA in 2012 as a long-term treatment for obesity for adults with a
body mass index of 30 kg/m2 or with a BMI 27 kg/m2 with at least 1 weight-related comorbidity.
Phentermine is an adrenergic agonist that promotes weight loss by activation of the sympathetic
nervous system and release of endorphins with a subsequent decrease in food intake and increased
resting energy expenditure. This occurs by modulating activity of anorectic or orexigenic peptides
in hypothalamic nuclei (14). Topiramate is an FDA approved medicine for epilepsy and migraine
prophylaxis that has been shown to reduce body weight by promoting taste aversion and decreasing
caloric intake. Phentermine/topiramate is available in 4 doses: 3.75/23 mg (starting dose), 7.5/46
mg (lowest treatment dose), 11.25/69 mg, or 15/92 mg (maximum treatment dose).
The 52-week CONQUER trial randomized 2487 patients who were obese with a mean BMI of
36.6 kg/m2 and comorbidities including hypertension, dyslipidemia, diabetes or pre-diabetes, or
abdominal obesity to either placebo, mid-treatment dose (7.5/46 mg), or maximum treatment dose
(15/92 mg) with results showing 6.6% and 8.6% placebo subtracted weight loss in the lower dose
and maximum dose arms respectively (19). A 2-year extension of the CONQUER trial was
published (SEQUEL) demonstrating a 2-year mean placebo subtracted weight loss of 8.7% in the
top group and 7.5% in the mid-dose group (20).
Improvement in systolic and diastolic blood pressure, triglycerides, and greater increases in HDL
were seen in subjects treated with phentermine/topiramate compared with placebo in the
CONQUER trials (19). Improvements in fasting glucose and insulin levels were seen in the
SEQUEL study and a 54% and 76% reduction in progression to type 2 diabetes in the 2 treatment
groups was noted in patients without diabetes at baseline (20).