Bronchiolite
Bronchiolite
L’incidenza annuale è di 11.4% nei bambini sotto 1
anno e 6% tra 1-2 anni. La malattia è responsabile di
4500 decessi e 90,000 ricoveri ogni anno negli USA.
Tra i bambini di 2 anni circa il 95% ha evidenza
sierologica di una pregressa infezione con il virus
respiratorio sinciziale. Rara nel neonato (< 28 gg) x
Ab. materni
Fattori di rischio:
Età < 6 mesi
Bambini con cardiopatia congenita
Bambini con displasia broncopolmonare
Bronchiolite
La B. è una infiammazione acuta delle piccole vie respiratorie che
esita in broncocostrizione per:
mediatori della flogosi (leucotrieni)
aumentata secrezione di muco
distruzione delle cellule epiteliali
edema delle vie aeree
È una malattia tipicamente del lattante (primi 12 mesi di vita) e
tipicamente di origine virale:
Virus respiratorio sinciziale
Virus parainfluenzale
Virus influenzale
Adenovirus
Metapneumovirus
C. trachomatis (< 4 mesi)
Bronchiolitis
Contagiosity
The disease is highly contagious. Viral
shedding in nasal secretions continues for 6
to as long as 21 days after the development of
symptoms. Incubation period is from 2-5 days.
Secondary infections occur in 46% of family
members, 98% of other children in day care,
42% of hospital staff and 45% of previously
uninfected hospitalized infants. Infection is
spread by fomites via environmental surfaces.
Hand washing and the use of disposable
gloves and gowns may reduce nosocomial
spread.
Decorso (5-7 giorni)
E’ una patologia tipica dei mesi invernali. Tipicamente
inizia come un banale raffreddore con o senza febbre di
solito di live entità e tosse. Gradualmente progredisce
verso una dispnea espiratoria con:
Tachipnea + tachicardia
Alitamento pinne nasali
Rientramenti soprasternali, intercostali e all’epigastrio
Difficoltà all’alimentazione
Complicanze:
Disidratazione
Apnee (bambini < 6 settimane)
Insufficienza respiratoria
Diagnosi
Dispnea
Wheezing (fischi e sibili su tutto l’ambito
polmonare + prolungamento della fase
espiratoria)
Rantoli fini crepitanti diffusi
Therapy
The mainstays of therapy for patients with bronchiolitis are:
oxygen supplementation and fluid replacement.
Hypoxemia
is the most common laboratory abnormality
detected, and supplemental oxygen administration is
common.
These infants are mildly dehydrated because of decreased
fluid intake and increased fluid losses from fever and
tachypnea. The goal of fluid therapy is to replace deficits and
provide maintenance requirements. Excessive fluid
requirements should be avoided as this may promote
interstitial edema formation.
Corticosteroids
Bronchodilators (?)
Indications for pediatric intensive care
referral
desaturation (Sat.O2 < 90-92%) in 40% O2 (3-
4 l/min O2)
PaCO2 > 60-65 mmHg
pH < 7.25
cyanosis
apnea
acidosis
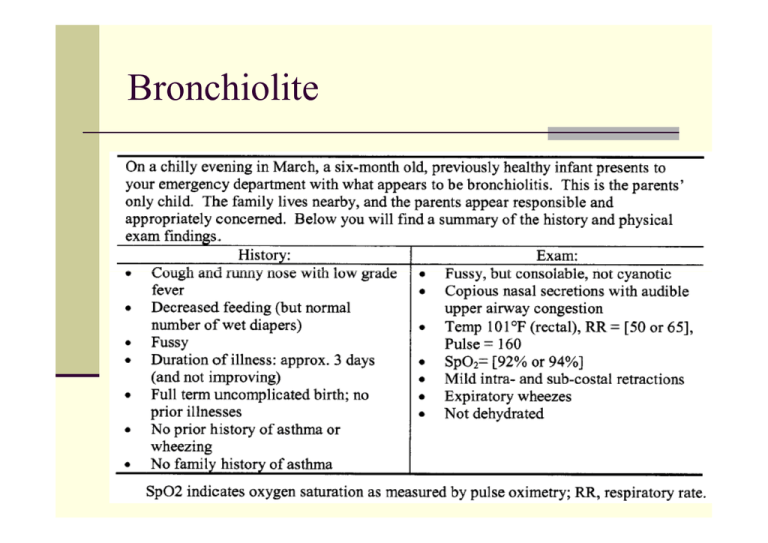
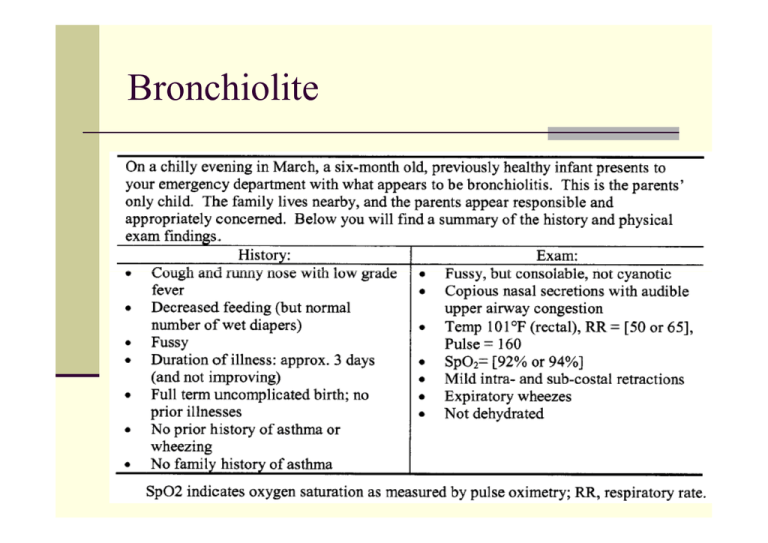
Caso clinico
A 16-month-old girl is evaluated in the ED for
increased work of breathing. She had been
seen 4 days ago for rhinorrhea, cough,
vomiting, diarrhea, and fever, all of which
appeared to have resolved. At that time, she
had a normal CBC and serum electrolyte
measurement and was treated with
intravenous fluids and discharged. Two days
later, she again developed cough with
posttussive vomiting and rhinorrhea, but no
fever or diarrhea.
Caso clinico
On physical examination, the girl is awake and alert
but in mild-to-moderate respiratory distress. Her
respiratory rate is 50 breaths/min, pulse oximetry
saturation is 94%, and heart rate is 161 beats/min.
She is afebrile. She has moderate pharyngeal
erythema, clear rhinorrhea, and a hyperemic right
tympanic membrane. Intercostal retractions, mild
wheezing, and occasional scattered crackles are
present. The rest of her physical findings are normal.
She is given three treatments of albuterol and
prednisolone and responds with a lower respiratory
rate of 40 breaths/min but a pulse oximetry saturation
of 92% in room air.
Caso clinico
She is given three treatments of albuterol and
prednisolone and responds with a lower
respiratory rate of 40 breaths/min but a pulse
oximetry saturation of 92% in room air.
Caso clinico
Initial laboratory studies include negative results for
respiratory syncytial virus (RSV) and influenza A and
B antigens. A chest radiograph shows no acute
disease and mild hyperinflation. She is admitted to
the hospital.
Over the next 3 days, she develops a temperature to
101°F (38.4°C) and has no improvement, despite
frequent albuterol treatments. On day 4, her WBC is
9x103/mcL (9x109/L), with 41% neutrophils, 2%
bands, 43% lymphocytes, and 7% monocytes, and
her platelet count is 775x103/mcL (775x109/L). A
urine culture is negative, but a blood culture is
reported positive for gram-negative diplococci.
Bronchiolite?
The patient's age of 16 months in conjunction with
cough, rhinorrhea, wheezing, and chest wall
retractions were consistent with a diagnosis of
bronchiolitis. Bronchiolitis is predominantly a viral
illness (RSV, parainfluenza 3 virus, adenovirus,
influenza virus) but also can be caused by
Mycoplasma. Notwithstanding negative antigen tests
for RSV and influenza A and B, she was treated for
presumptive viral lower respiratory tract disease.
The blood culture grew Moraxella catarrhalis, and
she was treated for 7 days with parenteral ceftriaxone
followed by 7 days of oral cefuroxime axetil. She was
discharged without complications.
Qualcosa di diverso?
Typically, bronchiolitis reaches its most critical
stage during the first 48 to 72 hours after the
onset of cough.
This patient's course was atypical because she
developed her initial fever after 3 days of cough
and wheezing, which proved to be indicative of a
bacterial infection. Although uncommon,
bronchiolitis may be complicated by bacterial
infection (about 2% to 10% of cases). Bacterial
otitis media and pulmonary bacterial coinfection,
as well as associated urinary tract infection, are
examples from recent literature.
Sepsi?
In general, a clinician should suspect sepsis
whenever a patient has fever associated with
behavioral changes such as irritability, fussiness,
lethargy, poor feeding, and altered mental status.
Tachycardia and tachypnea also may reflect sepsis.
Petechiae and purpura are well-known cutaneous
indicators of possible sepsis, especially
meningococcemia. A weak cry and jaundice may
indicate sepsis in neonates. The presentation of
sepsis depends on the competency of the patient's
immune system. Subtle presentations can occur in
young infants and immunocompromised children,
with the clinical picture influenced by the patient's
level of immunity.
Moraxella catarrhalis
M catarrhalis is an aerobic, gram-negative
diplococcus in the family Neisseriaceae that
commonly inhabits the upper respiratory tract
(nasopharynx), with increased seasonal colonization
in fall and winter. M catarrhalis can cause acute,
localized infection such as otitis media, sinusitis,
conjunctivitis, and pneumonia in children. Although it
causes a large proportion of cases of lower
respiratory tract infection in elderly patients who have
chronic obstructive pulmonary disease and chronic
bronchitis, this association has not been seen in
pediatric patients.
Moraxella catarrhalis
M catarrhalis generally is not thought of as causing
invasive, systemic disease (such as meningitis and
endocarditis) except in immunocompromised
conditions.
Risk factors for bacteremia include viral infection,
sickle cell disease, malignancy, acquired
immunodeficiency syndrome, and other
immunodeficient states.
This child did not have any other evidence of
immunodeficiency; thus, additional evaluation for that
state was not undertaken. It is possible that her
hyperemic tympanic membrane was caused by an M
catarrhalis infection, but the finding also could result
from underlying viral infection.
Moraxella catarrhalis
This child did not have any other evidence of
immunodeficiency; thus, additional evaluation
for that state was not undertaken. It is
possible that her hyperemic tympanic
membrane was caused by an M catarrhalis
infection, but the finding also could result from
underlying viral infection.
Moraxella catarrhalis
In the clinical laboratory, isolates of M catarrhalis
must be differentiated from Neisseria sp. The
management and infection control differences
between Neisseria sp and M catarrhalis are
important. As in this case, identification of gramnegative diplococci in a patient's blood culture
warrants droplet precautions for suspected
meningococcemia for 24 hours while the patient
receives appropriate antimicrobial therapy.
Confirmation of N meningitidis also warrants
antimicrobial prophylaxis for appropriate
contacts.
Moraxella catarrhalis
Also, major management and social implications are
associated with the differentiation between N
gonorrhoeae and M catarrhalis when gram-negative
diplococci are identified in the smear of an eye
discharge from a baby who has neonatal
conjunctivitis. Gonococcal neonatal conjunctivitis
requires systemic antimicrobial therapy for the baby
as well as evaluation and management of the mother
and her partner. A final diagnosis of M catarrhalis
does not raise any of these issues.
Terapia
More than 85% of M catarrhalis isolates are
ampicillin-resistant because of betalactamase production. First-line antibiotics for
focal infections (otitis media, sinusitis,
pneumonia) are oral amoxicillin-clavulanate or
oral second- and third-generation
cephalosporins. Other antibiotics active
against this organism include macrolides,
trimethoprim-sulfamethoxazole, and
fluoroquinolones.
Terapia
Sepsis generally is treated parenterally until the
patient becomes asymptomatic and has a negative
repeat blood culture, when treatment may be
changed to oral therapy to complete a 7- to 14-day
course, depending on the organism. When receiving
an initial report of "gram-negative diplococci" growing
in a blood culture, it is prudent to administer
parenteral third-generation cephalosporins (to cover
Neisseria sp and M catarrhalis) until the isolate is
identified. Then, therapy can be individualized,
depending on the clinical course and antimicrobial
susceptibility results
Messaggio da portare a casa
When the course of a patient's illness does not
follow the usual expectations, it is appropriate
to consider the possibility of multiple diseases
occurring simultaneously. Although rare, M
catarrhalis has the potential to cause a serious
bacterial infection.
The identification of gram-negative diplococcus
in the blood of a patient who has fever and
respiratory disease or otitis media should alert
the physician to the possibility of the uncommon
M catarrhalis as well as the more dangerous N
meningitidis.
Un caso “strano” per finire
Faith, 4 mesi di vita, prematura, viene
trasferita dal un Ospedale romano per febbre
(MAX: 39.6°C) da 1 settimana e diarrea.
E.O.:
modica dispnea
Tosse secca
FR 60 atti/min, Sat.O2: 90-93%
Milza e fegato palpabili a 2 cm dall’arco
costale.
Un caso “strano”
Laboratorio:
GB: 35.470 (73%)
Hb: 7.9 g/dL Trasfusa dopo 2 gg
PLT: 335.000
PCR: 18.8 mg/dL
D-dimeri: 3500 ng/mL (< 280)
EGA: modica alcalosi
Feci: Rotavirus ++
Rx torace: refertato nella norma
Inizia terapia con Amplital + Gentalyn
Un caso “strano”
Peggioramento progressivo delle condizioni generali in particolare della
dispnea.
Si sospetta bronchiolite ed inizia terapia specifica.
Dopo 4 gg di terapia:
GB: 21000 (N: 76%)
PLT: 139.000
PCR: 18 mg/dL
ECG e ecocardio: normali
Dopo 3 giorni si ripete RX torace che mostra micronoduli diffusi in tutto
il parenchima polmonare bilateralmente
TC polmonare:
Micronoduli diffusi
Focolai broncopneumonici lobo inf. Polmone dx e lingula polmone
sin.
Slargamento profilo mediastinico per incremento volumetrico timo e
linfonodi
Un caso “strano”
Peggioramento progressivo delle condizioni generali,
della dispnea, della Sat.O2, FR 85 atti/min, FC 152
atti/min.
Febbre persistente fino a 40°C, nonostante terapia
con Merrem e Targosid.
Sottopopolazioni linfocitarie:
CD4 totali (T Helper): 786.7 mmc
CD4/CD8: 2.95 (1.5-2.9)
Mantoux: neg.
Trasferimento In Unità Terapia Intensiva
HIV: Positivo
BAL: Micobatterio tubercolosi
Un caso “strano” per finire
Sepsis
Bacteremia: the recovery of bacteria in blood culture.
When bacteria are not effectively cleared by host
defense mechanisms, a systemic inflammatory
response is set into motion and can progress
independently of the original infection.
Sepsis: The systemic response to infection with
bacteria, viruses, fungi, protozoa or rickettsiae.
Sepsis is one of the causes of systemic inflammatory
response syndrome (SIRS). If not recognised or
treated early sepsis can progress to severe sepsis,
septic shock, multiple organ dysfunction syndrome
(MODS) and death.
Sepsis
Infection
Systemic Inflammatory Response Syndrome (SIRS)
•Hyper-hypothermia
•Tachycardia
•Tachypnea
•Increased or decreased white blood count
Sepsis
SIRS + hypotension
Severe Sepsis
Sepsis with organ dysfunction, hypoperfusion or hypotension,
Change in mental status, oliguria, hypoxemia, lactic acidosis
Septic shock
Severe sepsis + persistent hypotension despite adequate fluid resuscitation
Multiple Organ Dysfunction Syndrome (MODS)
Homeostasis cannot be maintained without intervention
Death