Epatiti virali
= malattie ad eziologia virale,
ubiquitarie, che colpiscono
PRIMITIVAMENTE il FEGATO
Epatiti acute
Epatiti croniche
Evoluzione storica
•
Fino al 1970: diagnosi generica di epatite virale:
– Epatite “epidemica”
– Epatite da siero
•
•
•
1970: Blumberg: Ag Australia nel siero di un paziente con epatite post- HBV
trasfusionale:
– Epatite AU+
– Epatite AU1973: identificazione di HAV
HAV
1976: diagnosi di Epatite A e B:
– Epatite AU+
– Epatite A
– Epatite Non A Non B (NANB)
• Forma oro-fecale
• Forma parenterale
1977: Rizzetto identifica VIRUS DELTA HDV
1983: identificazione virus E (test sierologico solo anni 90) HEV
•
•
•
1988: identificazione del virus HCV HCV
1989: test SIEROLOGICO per HCV
1994: identificazione del virus HFV
•
•
HFV
?
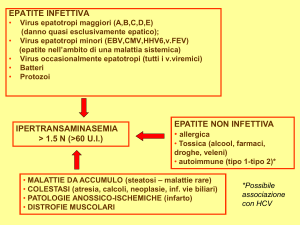
Virus epatitici maggiori
HAV
HDV
HBV
HEV
HCV
???
???
???
HGV
TTV
SEN-V
Virus epatitici maggiori
– Appartengono a differenti famiglie
– Acido nucleico
• DNA: HBV, TTV
• RNA: HAV, HCV, HDV, HEV, HGV
– Modalità di trasmissione
• oro-fecale: HAV, HEV
• parenterale: HBV, HCV, HDV, TTV
• verticale: HBV, HCV, HDV, HEV
– Differenti periodi di incubazione
– Diversa gravità dell’infezione acuta
– Evoluzione in forme croniche: HCV, HBV, HBV/HDV
– Disponibilità di un vaccino: HAV, HBV
Eziologia
Virus maggiori:
– HAV
– HEV
Trasmissione
oro-fecale
Non
chiara
– HGV
– GBV-A,B,C
Trasmissione
parenterale,
sessuale
HBV
HCV
HDC
HFV
Virus minori:
CMV
EBV
Quadro
epatico PURO
coxakie
herpes
virus parotite
virus rosolia
virus febbre gialla
virus Lassa
virus MarburgEbola
Raro
Viral Hepatitis - Overview
Type of Hepatitis
A
Source of
virus
Route of
transmission
Chronic
infection
Prevention
Incubation
time
B
C
D
E
feces
blood/
blood/
blood/
blood-derived blood-derived blood-derived
body fluids body fluids
body fluids
feces
fecal-oral
percutaneous percutaneous percutaneous
permucosal
permucosal
permucosal
fecal-oral
no
yes
yes
yes
Raro
pre/postpre/post- blood donor
pre/post- ensure safe
exposure
exposure
screening;
exposure
drinking
immunization immunization risk behavior immunization;
water
modification risk behavior
modification
15-45 days
40-160 days
15-180 d 30-160 d
15-50 days
Estimates of Acute and Chronic Disease
Burden for Viral Hepatitis, United States
Acute infections
(x 1000)/year*
Fulminant
deaths/year
Chronic
infections
Chronic liver disease
deaths/year
HAV
HBV
HCV
HDV
125-200
140-320
35-180
6-13
100
150
?
35
0
1-1.25
million
3.5
million
70,000
5,000
8-10,000
1,000
0
* Range based on estimated annual incidence, 1984-1994.
Source: CDC Sentinel Counties Study on Viral Hepatitis
Hepatitis B & C: similarities and differences
Hepatitis B
Hepatitis C
DNA
RNA
Genome
Symptomatic Acute dis.
Occult infection
+++
Yes
Chronicity
++
Goal of therapy
suppression
++
No
+++
eradication
Liver cancer
+++
++
Vaccine
Yes
No
Relative Efficiency of HBV, HCV, HIV
Transmission by Type of Exposure
Type of exposure
transmission
to infected source
Efficiency of
HBV
HCV
HIV
Transfusion
Injecting drug use
Unsafe injections
Needlestick
Sexual
Perinatal
Non-intact skin
Intact skin
++++
++++
+++
+++
++++
+++
++
-
++++
++++
+++
+
+
+
+/-
++++
++++
+
<+
+++
+++
+/-
Epatite acuta: aspetti clinici
•
•
1)Periodo PRE-ITTERICO:
–
durata: 3-8 giorni
–
astenia, malessere
–
turbe digestive
–
febbricola (23% casi)
–
artro-mialgie
–
reaz. Orticarioide
–
eruzioni maculopapulose (sind. Giannotti-crosti)
–
URINE IPERCROMICHE
AUM. transaminasi
valori: 500-2000 UI/ml
inversione rapporto
1° segno nel bambino
Forma classica
•
2) Periodo ITTERICO:
–
durata: 2 sett-2 mesi (fino a 6 mesi)
–
DA sub-ittero (ittero sclerale) A ittero franco
(a volte bifasico)
–
oliguria, ipercromia urinaria
–
FECI IPOCOLICHE
E.O.: epatomegalia “molle”
calo ponderale
splenomegalia
AUM. transaminasi
IPER-bilirubinemia tot: 4-30 mg/dl
aum PT
3) CONVALESCENZA:
–
miglioramento progressivo
della cenestesi
–
astenia persistente
Graduale normalizzazione
transaminasi
Epatite acuta: aspetti clinici
•
Forme particolari
Epatite asintomatica:
–
no sintomi
–
frequente
–
individuabile SOLO con markers epatitici
•
•
Epatite ANITTERICA:
–
come ep. Classica MA senza ittero
–
più frequente nei BAMBINI
E.O.: epatomegalia “molle”
calo ponderale
splenomegalia
AUM. transaminasi
Epatite colestatica
–
più frequente negli anziani
–
ittero intenso e persistente
–
ACOLIA FECALE
–
PRURITO
IPER-bilirubinemia ELEVATA
AUM. Transaminasi
EPATITE FULMINANTE:
espressione di necrosi MASSIVA ACUTA del
fegato
•
ANDAMENTO RAPIDO:
ATROFIA giallo-acuta
andamento (24 hrs)
piu lento
(1 settimana)
Segno di allarme:
SONNOLENZA
allungamento PT
ES. DI LABORATORIO:
SINTOMI:
•Encefalopatia:
stato confusionale
ebrezza,
sonnolenza,
COMA
•nausea,vomito, alitosi epatica (foetor epaticus)
•incremento ITTERO
•MANIFESTAZIONI EMORRAGICHE
•ascite (10%)
•ipotensione, tachicardia, IRA (fase terminale)
IPER-bilirubinemia ELEVATA
RIDUZIONE rapida delle
Transaminasi
Ipo-glicemia
ipo-albuminemia
RID. Fibrinogeno
ALLUNGAMENTO PT
EO:
RIDUZIONE AIA EPATICA
ecchimosi
segni neurologicici
Epatite acuta:
EPATITE A
EPATITE E
EPATITE B
EPATITE C
Distribuzione dei casi di epatite virale acuta
riportati all’ISTAT in Italia
Totale casi riportati:
Totale casi riportati:
5725
2,2%
14,7%
3602
1,7%
51,7%
13,2%
HAV
1998
HBV
HCV
2002
nAnBnC
31,4%
37,8%
47,3%
Distribuzione di casi notificati di epatite
virale (SEIEVA)
2,4%
19,9%
8,5%
63,5%
23,6%
1987 - 1990
56,5%
1997 - 2003
Epatite A
Epatite A
Epatite B
Epatite B
Epatite
nAnBnC
Epatite C
nAnBnC
25,6%
Distribuzione dei casi di epatite virale acuta
(SEIEVA 2000-2004)
Sconosciuta
8%
Epatite nAnBnC
21%
Epatite C
9,2%
Epatite B
29,4%
Epatite A
51,3%
Tassi annuali di incidenza (/100.000)
di epatite acuta A, B, e nAnB in Italia
Epatite
1985
1990
1997
2006
A
10
2
19
1,4
B
12
5
3
1,6
non A, non B
5
2
1
0,5
Acute Viral Hepatitis by Type, United States, 1982-1993
34%
47%
16%
Hepatitis A
Hepatitis B
3%
Source: CDC Sentinel Counties Study on Viral Hepatitis
Hepatitis C
Hepatitis
Non-ABC
EPATITE A
Picornavirus, RNA, lineare
SENZA envelope lipidico
1 unico sierotipo
min
Anticorpi
protettivi
duraturi
RESISTENTE all’etere
RESISTENTE al calore (60°, 10
È inattivato DA:
UVB
ebollizione
formalina, 37°, 72 hrs
Distribuzione dell’infezione da HAV
nel mondo
CDC Atlanta
GLOBAL PATTERNS OF
HEPATITIS A VIRUS TRANSMISSION
Endemicity
High
Moderate
Low
Very low
Disease
Rate
Low to high
Peak Age
of Infection
Transmission
Patterns
Early childhood
Person to person;
outbreaks uncommon
High
Late childhood/
young adults
Person to person;
food and waterborne
outbreaks
Low
Young adults
Person to person;
food and waterborne
outbreaks
Very low
Adults
Travelers; outbreaks
uncommon
Sieroprevalenza:
Frequenza di Ab-anti HAV IgG nella popolazione (frequente
INFEZIONE ASINTOMATICA)
• ITALIA:
– anni ‘50:
• 90% della popolazione
• sieroconversione in ETA’ pediatrica (infezione meno grave)
• adulti erano protetti
– attualmente:
• 70%
• siroconversione in età più adulta (infezioni più gravi)
•Svizzera: 5%
•Svezia <5%
•USA: 10%
•India:98%
REPORTED CASES OF SELECTED NOTIFIABLE DISEASES
PREVENTABLE BY VACCINATION, UNITED STATES, 2001
Hepatitis A
Hepatitis B
Pertussis
Meningococcal disease
H. influenzae, invasive
Mumps
Measles
Source: NNDSS, CDC
10,609
7,843
7,580
2,333
1,597
266
116
EPATITE A: VIA ORO-FECALE
EPATITE A: VIE DI TRASMISSIONE
Sorgente di infezione:
• Contatto personale diretto
(e.g., domestici, contatti sessuali,
asili)
• Cibi contaminati, acqua
(e.g., verdure, mitili, balneazione)
UOMO infetto sintomatico o asintomatico
Elimina il virus dalla II metà della fase di incubazione
fino al 14° giorno di malattia
Concentrazioni del virus nei liquidi biologici
Body Fluids
Feces
Serum
Saliva
Urine
100
102
104
106
Infectious Doses per mL
Source:
Viral Hepatitis and Liver Disease 1984;9-22
J Infect Dis 1989;160:887-890
108
1010
Epatite A: patogenesi
Effetto citopatico
diretto su
EPATOCITA
replicazione
del virus
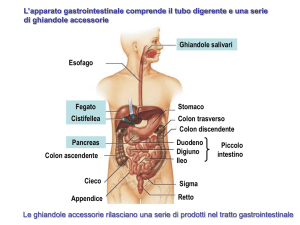
1 ingestione
fegato
Vena porta
Tubo digerente
4
3
2
bile
5
FECI
RISK FACTORS ASSOCIATED WITH
REPORTED HEPATITIS A,
1990-2000, UNITED STATES
Sexual or
Household
Contact 14%
Unknown
46%
International
travel 5%
Men who have
sex with men
10%
Injection drug use
6%
Child/employee in
day-care 2%
Other Contact
8%
Source: NNDSS/VHSP
Contact of daycare
child/employee
6%
Food- or
waterborne
outbreak 4%
Epatite A e trasmissione non convenzionale
•An outbreak of hepatitis A among homosexual men in Melbourne
(Stewart T, Med J Aust. 1993 Apr 19;158(8):519-21.
•An Outbreak of Hepatitis A among Homosexual Men in Amsterdam,
1991–1993 ANNE LEENTVAAR-KUIJPERS et al., Int. J.
Epidemiol..1995; 24: 218-222
•Outbreak of hepatitis A in Rotterdam associated with visits to
'darkrooms' in gay bars.
(Reintjes R et al. 1: Commun Dis Public Health. 1999 Jan;2(1):43-6)
•
La prevenzione NON passa per l’uso del CONDOM !!!!!!!
• Studio caso controllo (18 casi e 64 controlli)
durante una epidemia (1 giugno-4 Agosto) di
epatite A a Copenaghen (Danimarca, paese a
bassa endemia)
Bassa incidenza, alta % di soggetti
non protetti (IgG anti HAV neg)
Area a più alta incidenza,
Che diminuisce allontanandos
Dalla capitale
OMOSEX
OUTBREAK
protettivo
• Nessuna differenza per quanto riguarda i sexual
behaviors (rapp. oro-anali, digito-anali)
• Utilizzo di saune: a rischio aumentato indip.
(svariati partners in un tempo ridotto, Fattore calore?)
• Più partners
• Rapporti a casa più protetti
“Based on the results of the investigation we suggest
recommending hepatitis A vaccination to
all MSM who are not in a monogamous relationship,
especially if they visit gay saunas or other places with
frequent partner change.”.
EPATITE A
MALATTIA CLINICA
Infection
ALT
Response
IgM
IgG
Viremia
HAV nelle FECI
0
1
2
3
4
5
Fine
contagio
6
7
8
9
10
11
12
Week
13
EPATITE A - aspetti clinici
•Ittero
<6 anni
6-14 anni
>14 anni
<10%
40%-50%
70%-80%
•prevalenza dei sintomi GASTROENTERICI
•ESORDIO più BRUSCO
•complicazioni:
epatite fulminante (1%)
Epatite colestatica
Decorso protratto (bi- o poli-fasico)
•periodo di incubazione:
Average 30 days
Range 15-45 days
CRONICIZZAZIONE: MAI!!!!
EPATITE A - iter diagnostico
Anamnesi patologica prossima:
disturbi GI, astenia
urine ipercromiche
feci ipocoliche
Dati epidemiologici (ultime 2-6 sttimane) :
ingestione di mitili, verdura ecc nelle
lavoro a contatto con bambini
rapporti sessuali/omo
VIAGGI in zone ad alta p
EO: epatomegalia, ittero, sub-ittero
Esami di I°livello: transaminasi, bilirubinemia
Esami di II°livello: ricerca Ab anti-HAV IgM
NORME DI PROFILASSI
• Isolamento del paziente:
– SOLO se è un pz diarroico, incontinente o è un
bambino
• Ig specifiche (difficili da reperire):
– entro 10 g dal contagio/ durata di circa 5 mesi
– contatti stretti, viaggiatori per brevi periodi(?)
• VACCINO
– HAVRIX: virus inattivato con formalina, i.m.
PREVENTING HEPATITIS A (CDC)
• Hygiene (e.g., hand washing)
• Sanitation (e.g., clean water sources)
• Hepatitis A vaccine (pre-exposure)
• Immune globulin (pre- and postexposure)
HEPATITIS A VACCINE EFFICACY STUDIES
Site/
Age Group
Vaccine
HAVRIX
(GSK)
Thailand
Vaccine Efficacy
(95 % Cl)
N
38,157
1-16 yrs
94%
(79%-99%)
2 doses
360 EL.U.
VAQTA
(Merck)
New York
2-16 yrs
1 dose
25 units
JAMA 1994;271:1363-4; N Engl J Med 1992;327:453-7
1,037
100%
(85%-100%)
Indicazione alla vaccinazione:
• Viaggiatori abituali o per più di tre mesi in zone
ad alta endemia
• bambini piccoli che viaggiano in zone ad alta
endemia
• chi vive in case famiglie, case di riposo ecc...
• alimentaristi
• operatori sanitari
• omosessuali, TD
• emofilici
• epatopatici cronici (HBV, HCV)
Calendario vaccinale:
• Viaggiatori: 0, 2 settimane, dopo 9 mesi
(efficace dopo 1 mese)
• Adulti: 0, 6-12 mesi
• Bambini: 0, 1 mese, dopo 6-12 mesi
SAFETY OF HEPATITIS A VACCINE
Più comuni effetti collaterali
arrossamento e indurimento al sito di iniezione 50%
Cefalea - 15%
Malessere - 7%
assenza di reazioni avverse gravi
sicurezza in gravidanza: non determinata
Contro-indicazioni: reazioni avverse contro i componenti
del vaccino
NO speciali precauzioni negli IMMUNOCOMPROMESSI
Durata della protezione dopo il vaccino
• Persistence of antibody
• At least 5-8 years among adults and children
• Efficacy
– No cases in vaccinated children at 5-6 years of
follow-up
• Mathematical models of antibody decline
suggest protective antibody levels persist
for at least 20 years
• Other mechanisms, such as cellular
memory, may contribute
ACIP RECOMMENDATIONS FOR PREVENTION OF
HEPATITIS A USING HEPATITIS A VACCINE
1999
ACIP: Advisory Committee on immunization Practices
1999 ACIP RECOMMENDATIONS FOR ROUTINE
HEPATITIS A VACCINATION OF CHILDREN
Children Who Should be Routinely Vaccinated
- living in states, counties, and communities where the average
hepatitis A rate was 20 cases/100,000 during baseline period.
Children Who Should be Considered for Routine Vaccination:
- living in states, counties, and communities
where the
average hepatitis A rate was <20 but 10 cases/100,000
during
the baseline period.
COMBINED HEPATITIS A
HEPATITIS B VACCINE
Approved by the FDA in United States for persons >18
years old
Contains 720 EL.U. hepatitis A antigen and
20 μg. HBsAg
Vaccination schedule: 0,1,6 months
Immunogenicity similar to single-antigen vaccines
given separately
Can be used in persons > 18 years old who need
vaccination against both hepatitis A and B
Formulation for children available in many other
countries
1999 ACIP RECOMMENDATIONS FOR STATEWIDE
ROUTINE HEPATITIS A VACCINATION OF CHILDREN
Rate > 20/100,000*
Recommended
Rate 10-20/100,000*
Considered
Rate < 10/100,000*
Not statewide
* Based on average incidence rate during baseline period (1987- 97)
Hepatitis A Incidence, United States,
1980-2002*
1995 vaccine licensure
1996 ACIP recommendations
16
Cases/100,000
1999 ACIP recommendations
12
8
2002 rate* = 2.9
4
0
1980
*2002 rate provisional
'85
1990
Year
'95
2000
1987-97 average incidence
Hepatitis A
Incidence
NYC
DC
2002 incidence
rate per 100,000
0-4
>=20
5-9
10-19
NYC
DC
Rate per 100,000
> = 20
10 - 19
5-9
0-4
rate per 100,000
0-4
>=20
5-9
10-19
STD Treatment Guidelines
MMWR May 10, 2002 51(RR06)
“Vaccination against hepatitis is the
most effective means of preventing
sexual transmission
of hepatitis A and B.”
Hepatitis E Virus
•Virus a RNA, senza envelope
•famiglia degli hepevirus
•4 genotipi
•Zoonosi (Bacino animale:maiali)
•Originariamente descritto nei paesi a
basso livello sociosanitario (genotipo 1 e 2)
• Attualmente causa epidemie sporadiche
nei paesi industrializzati non endemici (genotipo 3,4)
Hepatitis E virus (HEV) infection is arguably
the most frequent acute viral hepatitis
infection around the world.
The real global burden of HEV infection is
not established, but it is estimated
that one-third of the world population has
been infected with HEV.1
Vet Microbiol. 2011 May 5;149(3-4):330-8. Epub 2010 Dec 16.
Viral and antibody HEV prevalence in swine at slaughterhouse in Italy.
Di Bartolo I, Ponterio E, Castellini L, Ostanello F, Ruggeri FM.
Department of Veterinary Public Health and Food Safety, Istituto Superiore di Sanità, Viale Regina
Elena 299, 00161 Rome, Italy. [email protected]
Abstract
Hepatitis E is an acute disease of humans caused by a small RNA virus, Hepatitis E virus (HEV). In
recent years, an increasing number of autochthonous human infections have been reported in
industrialized countries. Genotype 3 is the main HEV type circulating in swine, and is also reported in
sporadic cases of hepatitis E in humans worldwide. To date one serotype has been described. We
have conducted a survey to detect antibodies against HEV in 48 swine at a slaughterhouse in
Northern Italy, using ELISA test. Mean seroprevalence in the studied animal group was 87.0%. Bile,
liver and feces from the 48 animals were also collected, and HEV RNA was detected by nested
reverse transcription-polymerase chain reaction, amplifying a fragment of the ORF2. HEV genome
was most frequently detected in bile samples (51.1%), followed by feces (33.3%) and liver (20.8%).
Thirty-one out of 48 studied pigs (64.6%) were positive for HEV RNA in at least one sample. Overall,
HEV RNA was found at a statistically higher rate in the 3-4-month-old than in 9-10-month-old
animals (95.0% vs. 42.9%). Genetic characterization of swine strains identified was performed by
sequencing and database alignment. Phylogenetic analysis on the nucleotide sequences from 14
positive PCR products indicated that all strains belonged to genotype 3, clustering in two
branches subtypes g3c and g3f.
Geographic Distribution of Hepatitis E
Outbreaks or Confirmed Infection in >25% of Sporadic Non-ABC Hepatitis
•È diffusa nei PVS della fascia tropicale e sub-tropicale
•In ITA: sieroprevalenza: 0.74%
•soggetti più colpiti: DONNE 15-20 anni
Hepatitis E - Aspetti clinici
• Periodo di incubazione: Average 40 days
Range 15-60 days
• Forme fulminanti:
pop. generale 1%-3%
GRAVIDE (III trimestre): 15%-25%
• severità:
• Cronicizzazione:
aumenta con l’età
RARO (segnalazione in trapiantati*)
• in gravidanza: UNICO virus epatico che raggiunge il fegato
fetale
Hepatitis E Virus Infection
Typical Serologic Course
Symptoms
IMMUNITA’ MENO DURATURA
ALT
IgG anti-HEV
(2-4 anni)
Titer
IgM anti-HEV (breve durata)
Virus in stool
0
1
2
3
4
5
6
7
8
Weeks after Exposure
DAGNOSI: IgM anti-HEV
9
10
11
12
13
Prevention and Control Measures for
Travelers to HEV-Endemic Regions
• Avoid drinking water (and beverages with ice) of unknown purity,
uncooked shellfish, and uncooked fruit/vegetables not peeled or
prepared by traveler
• IG prepared from donors in Western countries does not prevent
infection
• Unknown efficacy of IG prepared from donors in endemic areas
• Vaccine
Lancet. 2010 Sep 11;376(9744):895-902. Epub 2010 Aug 20.
Efficacy and safety of a recombinant hepatitis E vaccine in healthy adults: a largescale, randomised, double-blind placebo-controlled, phase 3 trial.
Zhu FC, Zhang J, Zhang XF, Zhou C, Wang ZZ, Huang SJ, Wang H, Yang CL, Jiang HM, Cai JP, Wang YJ, Ai X, Hu YM, Tang Q,
Yao X, Yan Q, Xian YL, Wu T, Li YM, Miao J, Ng MH, Shih JW, Xia NS.
Abstract
METHODS:
Healthy adults aged 16-65 years in, Jiangsu Province, China were randomly assigned in a 1:1 ratio
to receive three doses of HEV 239 (30 microg of purified recombinant hepatitis E antigen adsorbed
to 0.8 mg aluminium hydroxide suspended in 0.5 mL buffered saline) or placebo (hepatitis B
vaccine) given intramuscularly at 0, 1, and 6 months. ...........This trial is registered with
ClinicalTrials.gov, number NCT01014845.
FINDINGS:
11,165 of the trial participants were tested for hepatitis E virus IgG, of which 5285 (47%) were
seropositive for hepatitis E virus. Participants were randomly assigned to vaccine (n=56,302) or
placebo (n=56,302). 48,693 (86%) participants in the vaccine group and 48,663 participants (86%)
in the placebo group received three vaccine doses and were included in the primary efficacy
analysis. During the 12 months after 30 days from receipt of the third dose 15 per-protocol
participants in the placebo group developed hepatitis E compared with none in the vaccine group.
Vaccine efficacy after three doses was 100.0% (95% CI 72.1-100.0). Adverse effects attributable to
the vaccine were few and mild. No vaccination-related serious adverse event was noted.
INTERPRETATION:
HEV 239 is well tolerated and effective in the prevention of hepatitis E in the general
population in China, including both men and women age 16-65 years.
Hepatitis B Virus
•Hepadnavirus
•virus a DNA, con envelope
•non coltivabile in vitro
citoplasma
SINTESI
nucleo
envelope
DNA ds
CORE
EPATOCITA
Ag Australia
forma solubile (non infettante)
DNA Pol
HBsAg
VIRUS INTERO
(p. di Dane)
envelope
DNA ds
CORE
DNA Pol
HBsAg
HBV:
•altamente resistente
al calore
•resiste fino a 72 hrs a
temperatura ambiente
Distribuzione geografica dell’infezione da HBV
circa 400 milioni di portatori nel mondo
Ogni anno circa 500.000 morti per cirrosi ed epatocarcinoma da infezioni croniche da HBV
e circa 40.000 decessi per epatite acuta da HBV.
Nelle aree ad elevata prevalenza di infezione da HBV, il rischio di carcinoma epatocellulare
è circa 100 volte maggiore nei soggetti infetti rispetto ai soggetti non infetti.
La prevalenza di HBsAg in Europa è generalmente basso ma
è più alto nelle aree del Sud e dell’Est
>8%
2-8%
1-2%
<1%
2,2
2,1
2,0
Prevalenza di HBsAg (%)
1,8
1,5
1,6
1,7
1,4
1,2
1,0
0,8
0,65
0,4-0,8
0,6
0,4
0,2
WHO Collaborative Centre, University of
Antwerp , WHO/EURO and Publications
0,0
Francia Germania Italia
Spagna
Grecia
Zarski JP et al. J Hepatol. 2006; 45:355-360; Robert-Koch Institute. Epidem Bull. 2005; 46:421436; D’Amelio R et al. Am J Epidemiol. 1992; 135:1012-1018; Sola R et al. Med Clin (Barc). 2002;
119:90-95; Gogos CA et al. Eur J Epidemiol. 2003; 18:551-557
Distribuzione geografica dei
genotipi di HBV
F
D
A
D
A, B, C, D
C
C
D
D
D
E
Bj
Ba
F
F
A
A, B, C, D
Annual Hepatitis B
Infections in the United States
HBV Acute Infections
300,000
5% to 10% chronicity
Chronic Hepatitis B
15,000 - 30,000
1.0-1.25 million people in the United States
are chronic carriers of HBV
MMWR.
1991;40:1-17.
Alter MJ, et al.
Gastroenterol Clin North Am.
1994;23:437-455.
Sorgente di infezione:
UOMO infetto sintomatico o asintomatico
Elimina il virus per tutta la fase ACUTA (2stt-3 mesi)
e in TUTTA la FASE CRONICA (anni)
Attraverso la VIA
• SESSUALE
• PARENTERALE
• PARENTERALE INAPPARENTE
• PERINATALE
Concentration of Hepatitis B Virus
in Various Body Fluids
Low/Not
High
Moderate
Detectable
blood
semen
urine
serum
vaginal fluid
feces
wound exudates
saliva
sweat
tears
breastmilk
Inb. intestinale
VIE DI TRASMISSIONE EPATITE HBV
• PARENTERALE:
•
trasfusioni sangue ed emoderivati (attualmente NO)
•
SCAMBIO di SIRINGHE
•
punture accidentali
• PARENTERALE INAPPARENTE:
•
microlesioni cute e mucOSE
•
tatuaggi, piersing
•
cure dentali, pedicure
•
contagio domestico (rasoi, spazzolini, forbici)
• SESSUALE:
•
rapporti NON protetti da preservativo
•
25% di rischio
• PERINATALE (durante il parto):
• 90-100% casi: da madre HBsAg+/HBeAg+
• 25% : da madre HBsAg+/HBeAg-/ antiHbeAg• 5%: da madre HBsAg+/antiHbeAg+
Epatite B: distribuzione dei fattori di rischio
(SEIEVA 1998-2005)
Nessuno dei
precedenti fattori
di rischio
29,1%
Droghe
14,9%
Convivente HBsAg+
6,9%
Trasfusioni
2,5%
Terapia
odontoiatrica
8,8%
> 1 partner
8,1%
Interventi chirurgici
6,9%
Altre esp. parenterali
20%
Risk Factors for Acute Hepatitis B
United States, 1992-1993
Heterosexual* (41%)
Injecting
Drug Use
(15%)
Homosexual Activity (9%)
Household Contact (2%)
Health Care Employment (1%)
Unknown (31%)
Other (1%)
* Includes sexual contact with acute cases, carriers, and multiple partners.
Source: CDC Sentinel Counties Study of Viral Hepatitis
HBV e comportamenti sessuali
HBV: patogenesiI
Penetrazione sessuale o parenterale
EPATOCITA
citoplasma
Passaggio ematico
FEGATO
Replicazione
virale
HBcAg
nucleo
HBeAg
bile
MHC I + Ag virali
EFFETTO
CITOLITICO
immuno-mediato
su
epatociti
Tcitotox
•Urine
•saliva
•secrezioni
Tubo digerente
Inattivazione intestinale
TCR
NK
Altri organi
FECI
Replicazione
virale
HBsAg
HBV: patogenesi II
Ab anti-HBsAg
B
HBsAg
Neutralizzazione
del virus
HBV: patogenesi III
BUONA RISPOSTA immune
EVOLUZIONE
SCARSA RISPOSTA immune
E/o
Alta virulenza VIRUS
EPATITE ACUTA
Fase 1
Ab anti-HBsAg
B
Fase 2
HBsAg
Comparsa anti HBs
Fase 3
GUARIGIONE-IMMUNITA’
HBV persiste
no danno epatico
massivo
DANNO istologico
HBV persiste
danno epatico
COSTANTE
Lesione infiammatoria-necrotica
EPATITE CRONICA-CIRROSI
EPATOCARCINOMA
“Portatore” SANO
STOP alla replicazione virale
CIRROSI INATTIVA
HBV: storia naturale
•Infezione asintomatica
•epatite ACUTA
Epatite FULMINANATE
5-10%
GUARIGIONE
(anti-HBsAg+
HBsAg -)
CRONICIZZAZIONE
(anti-HBsAg-, HBsAg +)
Persiste
REPLICAZIONE
Persistenza
virale
di
HBV in
Clearance
Completa
di
forma
HBV
MAL. EVOLUTIVAocculta
(HBsAg+, HBV-DNA+
HBeAg +)
1%
Chemioterapici
“Portatore” asintomatico
(anti-HBsAg-, HBsAg +)
F.
immunoComparsa mutante
soppressori
(HBsAg+, HBV-DNA+
HBeAg -, anti-HBe+)
Assenza di
REPLICAZIONE
Rituximab
virale
MAL. NON
EVOLUTIVA
(HBsAg+, HBV-DNAHBeAg -, anti-HBe+)
EPATOCARCINOMA
Resta tale
guarigione
(HBsAg, anti-HBs+)
HBV
reactivation
Storia naturale dell’infezione
cronica da HBV
Risoluzione
Infezione
acuta
Stabilizzazione
Epatite
cronica
Portatore cronico
Cirrosi
Progressione
Anni
Cirrosi compensata
HCC
Cirrosi scompensata
(Morte)
10-20
Morte
Fattori che influenzano la storia naturale
della malattia da HBV
Genere
Carica virale
di HBV
Età all’epoca
dell’infezione
Stato immunologico
dell’ospite
Progressione della malattia da HBV
Coinfezioni con
HCV o HIV
Mutazioni virali
HBeAg
Uso di alcolici
Fattovich. Semin Liver Dis 2003; 23:47-58; Chen et al. JAMA 2006; 295:65-73
Immunopatologia dell’infezione
da HBV
Risposta
immunitaria
Replicazione
virale
CD8+
HBV
Immunotolleranza
CD8+
HBV
Fase di clearance
Epatite cronica
HBV
Sieroconversione
Remissione
CD8+
Guidotti et al. 1999; Guo et al. 2000; Kakimi et al. 2000; Zhu et al. 2001
EPATITE DA HBV con guarigione
Tipico quadro SIEROLOGICO
Symptoms
anti-HBe
HBeAg
HBV-DNA
Total anti-HBc
Titer
GUARIGIONE
0
4
anti-HBs
IgM anti-HBc
HBsAg
8
12
16
20
24
28
32
36
Weeks after Exposure
52
100
EPATITE DA HBV con cronicizzazione
Tipico quadro SIEROLOGICO
Acute
(6 months)
Chronic
(Years)
HBeAg
anti-HBe
HBsAg
Total anti-HBc
Titer
HBV-DNA
IgM anti-HBc
0
4
8
12 16 20 24 28 32 36
Weeks after Exposure
52
Years
EPATITE DA HBV “mutante” con cronicizzazione
Tipico quadro SIEROLOGICO
Acute
(6 months)
Chronic
(Years)
HBeAg -
anti-HBe HBsAg
Total anti-HBc
Titer
HBV-DNA
PEGGIORE PROGNOSI
IgM anti-HBc
0
4
8
12 16 20 24 28 32 36
Weeks after Exposure
52
Years
Mutanti pre-core (“minus”) di HBV
• Non sono capaci di produrre più HBeAg (mutazione da triptofano
a codone di STOP)
• molto comuni nell’area del mediterraneo
• in aumento dal 1975 (HBeAg pos: 58%) ad oggi (89%)
• 3 possibilità:
– infezione mista iniziale da virus selvaggio e virus minus con
s
successiva comparsa di Anti-HBeAg e negativizzazione HbeAg per
selezione (il virus si nasconde negli epatociti e cronicizza con scarsa
risposta all’IFNa)
s e – infezione da virus selvaggio con HBsAg + e HBeAg , nel tempo si
formano gli Ab anti-Hbe con riduzione della replicazione virale.
Successivamente si seleziona il ceppo minus con ripresa della
s
replicazione virale
– infezione primaria da variante minus (più alta incidenza di epatite
s
fulminante)
s e
Hepatitis B - Aspetti clinici
• Periodo di INCUBAZIONE
media 60-90 days
range
45-180 days
• ittero:
<5 yrs, <10%
>5 yrs, 30%-50%
• epatite fulminante:
0.5%-1%
• Chronic infection:
<5 yrs, 30%-90%
>5 yrs, 2%-10%
• Premature mortality from
chronic liver disease:
15%-25%
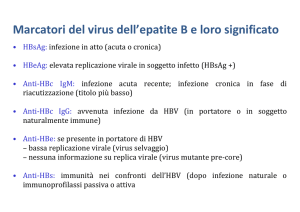
EPATITE B - iter diagnostico
Anamnesi patologica prossima:
disturbi GI, astenia
urine ipercromiche
feci ipocoliche
Dati epidemiologici (ultimi 60-90 giorni) :
rapporti sessuali/omo
manovre invasive, dentista
EO: epatomegalia, ittero, sub-ittero
Esami di I°livello: transaminasi, bilirubinemia
Esami di II°livello:
Ab anti-HBcAg IgM……..+: EPATITE ACUTA
HBsAg…………+: EPATITE ACUTA o CRONICA
Ab anti-HBsAg………+: guarigione
HBeAg…..+: EPATITE acuta o cronica (segno di replicazione)
Ab-anti HBeAg…….+: insorgenza mutante o guarigione
HBV-DNA……..+: alta replicazione
Eradicazione dell’infezione da HBV
Obiettivi
•
•
•
•
Prevent chronic HBV Infection
Prevent chronic liver disease
Prevent primary hepatocellular carcinoma
Prevent acute symptomatic HBV infection
Eradicazione dell’infezione da HBV
Strategie
• Prevent perinatal HBV transmission
• Routine vaccination of all infants
Entro 24hrs: IgG specifiche
entro 1 sett: vaccino
Dal 1991: obbligatorietà
0-1-6 mesi
richiamo: 5 anni
• Vaccination of adolescents
– all unvaccinated children at 11-12 years of age
– “high-risk” adolescents at all ages
• Vaccination of adults in high-risk groups
Personale sanitario
studenti medicina
conviventi HbsAg+
militari
Estimated Incidence of Acute Hepatitis B
United States, 1978-1995
HBsAg screening
of pregnant women
recommended
80
Vaccine
licensed
Cases per 100,000 Population
70
Infant
immunization
recommended
60
OSHA Rule
enacted
50
Adolescent
immunization
recommended
40
30
20
Decline among
homosexual
men & HCWs
10
*
Decline among
injecting
drug users
0
78
79
* Provisional date
80
81
82
83
84
85
86
87
Year
88
89
90
91
92
93
94
95
• PEG-interferon
• Entecavir (Baraclude)
• Tenofovir (Viread)
• lamivudina (3TC) (Zeffix)
• Emtricitabina (3FTC)
• Adefovir
•
Come, chi, quando trattare e con quale strategia
terapeutica ?
Il “paradigma” di STRESA (Raccomandazioni AISF-SIMIT, 2008)
Stadio di malattia
Ishak
Lieve
Moderata
Severa
Cirrosi
S0-S1
S2
S3 S4
S5 S6
PEG-IFN
ALT elevate
NA
qualunque ALT
HBeAg pos:
HBV-DNA >20.000 IU/mL
>200 IU/mL
HBeAg neg:
HBV-DNA >2.000 IU/mL
>200 IU/mL
Considerare la terapia
TRATTARE
Fig. 1. The “Stresa Paradigm” summarizing the indications for treatment of patients
with HBeAg positive hepatitis B with or without cirrhosis. NA: nucleoside/tide analogues.
“In all patients with chronic arthritis requiring immunomodulating
treatments both HBV and HCV infection along with liver
conditions should be evaluated before any therapeutic decisions,
including differential diagnosis among virus-related autoimmune
disease and simple comorbidity.
Patients
with
HBV
infection
should
be
referred
to
the
hepatologist (?) and correctly classified into active, inactive,
and occult carriers. Similarly, rheumatic patients with active
chronic hepatitis C must be treated with sequential or combined
treatment with antiviral and biological agents.
Rituximab: Mechanism of action
• Rituximab initiates
complement-mediated
B-cell lysis
• Rituximab initiates cellmediated cytotoxicity
via macrophages and
NK cells
• Rituximab induces
apoptosis caspase-3,-9
CD20
Macrophage
B cell
Complement
cascade
B cell
B-cell lysis
Apoptosis
Rituximab
Clynes RA et al. Nat Med. 2000;6:373-374; Reff ME et al. Blood. 1994;83:435-
HBV reactivation following
rituximab
• The control of HBV infection is mediated mainly
by HBV-specific cytotoxic T lymphocytes
• B lymphocytes are still essential for antigen
presentation
• The failure in antigen presentation related to the
prolonged depletion of B cells by rituximab may
allow the HBV to escape the cytotoxic T
lymphocyte
control,
hence
leading
to
development of viral hepatitis reactivation
HBV reactivation
• Identification of “overt” and “occult” carrier
• HBV-DNA and ALT monitoring
• Antiviral prophylaxis
• Antiviral treatment
HBV assessment in patients
receiving biologic therapy
(i.e. anti-CD20, anti-CD52,
anti-TNF-a)
HBsAg, HBcAb, HBsAb,, AST, ALT, HIVAb,
HCVAb
HBs Ag HBcAb HBsAb -
HBV vaccination
if possible
HBs Ag HBcAb +
HBsAb+/-
quantitative
HBV-DNA
HBV-DNA
undetectabl
e
“HBV
reactivation”
Antiviral therapy :
ENTECAVIR/
TENOFOVIR
For high-risk
patients consider
combination
therapy
If HBVDNA
detectabl
e +
ALT/AST
increase
HBsAg +
HBcAb +
“potential occult
infection “ or
“resolved
hepatitis”
Closely monitoring
AST, ALT, HBV-DNA
HBV-DNA
detectable
“occult infection”
Antiviral therapy
(1-2 wks before
biologicals and 6 mos
after interruption):
ENTECAVIR/TENOFOVIR*
For low-risk patients
consider LAMIVUDINE
quantitative
HBV-DNA
HBV-DNA
undetectabl
e
“inactive
carriers”
Antiviral therapy (1-2
weeks before
biologicals and 6
months after
interruption):
ENTECAVIR/TENOFOVI
R
HBV-DNA
detectable
“active overt carriers”
Antiviral therapy (1-2 weeks
before biologicals and 12
months after interruption):
ENTECAVIR/TENOFOVIR
For high-risk patients
consider combination
therapy
HBsAg neg
antiHBs neg
antiHBc pos
HBV neg
Antivir Ther. 2010;15(6):929-32.
Caso clinico
- Donna di 60 anni, senza precedenti anamnestici di
rilievo.
- Nel 1997 diagnosi di linfoma non Hodgkin B
- A febbraio 2008 recidiva di Linfoma non Hodgkin a
piccole cellule B.
Screening virologico
- Prima di iniziare il trattamento
chemioterapico :
-
Ab anti HCV: negativo
HBsAg: negativo
Anti- HBc: positivo
Anti-HBs: positivo
- HBV-DNA: non rilevabile (<12 IU/ml).
Conclusioni
• Riattivazione di HBV in pazienti HBsAg neg
• Rebound virologico in corso di terapia antivirale con
entecavir
• Rebound non legato a resistenze farmacologiche ma
correlato a leucopenia prolungata
• Espressione di escape immunitario
Hepatitis D (Delta) Virus
antigen
HBsAg
•Scoperta italiana (Rizzetto)
•Virua a RNA
•virua DEFETTIVO:
• infetta SOLO se ricoperto da HBsAg
•infetta epatociti HBsAg+
RNA
Geographic Distribution of HDV Infection
Taiwan
Pacific Islands
HDV Prevalence
High
Intermediate
Low
Very Low
No Data
In ITALIA: attualmente 8% degli HBsAg (in diminuzione)
a rischio:
tossicodipendenti
conviventi
Hepatitis Delta in Europe: vanishing or refreshing ?
Prevalence of anti-HDV
in Germany
Prevalence of anti-HDV
in Italy
% anti-HDV positive
12
10
8
1997
2006
6
4
2
0
18-29
30-49
> 50
age (years)
Wedemeyer et al., Hepatology 2007
Gaeta et al., Hepatology 2007
HDV
Vie di trasmissione
• Esposizione percutanea
– tossicodipendenti
• Esposizione mucosa
– rapporti sessuali
• Infezione SIMULTANEA
– HBV+HDV (incub:2 mesi)
• SOVRA-INFEZIONE
– HDV in portatore HBsAg+
(incub:1 mese)
Epatite D - Aspetti clinici
• Infezione simultanea
– severità in fase acuta (doppio picco di
transaminasi)
– basso rischio di infezione acuta
• Sovra-infezione
– alta % di cronicizzazione (90%)
– rapida evoluzione in cirrosi
HBV - HDV Infezione simultanea
Typical Serologic Course
Symptoms
ALT Elevated
Titer
anti-HBs
IgM anti-HDV
HDV RNA
HBsAg
Total anti-HDV
Time after Exposure
Markers: HBsAg+/IgM anti HDV/IgMantiHBcAg+
HBV - HDV Superinfection
Typical Serologic Course
Jaundice
Symptoms
Total anti-HDV
Titer
ALT
HDV RNA
HBsAg
IgM anti-HDV
Time after Exposure
Markers: HBsAg+/IgM anti HDV/IgM antiHBcAg-/IgGantiHBcAg+
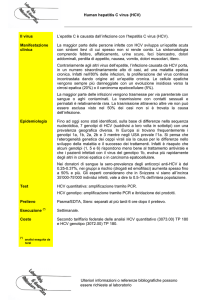
HCV:
•recentemente identificato al
microscopio elettronico (1996)
•simil flavivirus
•a RNA singola elica, con envelope
•alta capacità di MUTAZIONI
(envelope)
6 genotipi(1-6)
ogni genotipo:vari sottotipi(a,b,c..)
ogni sottotipo: Quasispecie
Resistente
all’ambiente esterno:
Disattivato da:
formalina
solventi organici
calore secco a 60°
Difficile
vaccino
Diversa
risposta
alla terapia
Diversa
distribuzione
geografica
HCV Lifecycle
Receptor binding
and endocytosis
Transport
and release
Fusion and
uncoating
ER lumen
(+) RNA
LD
LD
Translation and
polyprotein
processing
Virion
assembly
LD
Membranous
web
ER lumen
Adapted from Manns MP, et al. Nat Rev Drug Discov. 2007;6:991-1000.
RNA replication
Infezione da HCV nel mondo
• Infezione ubiquitaria
• Si calcola che 170 milioni di persone nel mondo
sono affette da epatite cronica HCVcorrelata (3% della popolazione mondiale)
• 3-4 milioni di nuove infezioni/anno
• Tassi di prevalenza variabili: 0.15% in
Scandinavia, 44% in alcune zone dell’Egitto e
del Camerun
Infezione da HCV nel mondo
(WHO, 1999)
Regione
Prevalenza
HCV (% )
Africa
5.3
Popolazione
infetta (milioni
di persone)
31.9
Americhe
1.7
13.1
M editerraneo
orientale
Europa
4.6
21.3
1.03
8.9
Sud-est asiatico
2.15
32.3
Pacifico
occidentale
TOTALE
3.9
62.2
3.1
%
169.7
MILIONI
Infezione da HCV:
modalità di infezione
Infezione da HCV: prospettive future
• Nei prossimi 20 anni i pz. HCV+ infettati negli
anni ‘80 raggiungeranno l’età in cui
generalmente si manifestano le complicazioni
della malattia, con un picco di prevalenza nel
2015
• Stime per il 2018:
– pz. con cirrosi HCV-correlata: 28.9% vs 15.6% nel
1988
– pz. con HCC: aumento del 63%
– pz. con insufficienza epatica: aumento dell’84%
– decessi HCV-correlati: aumento del 300%
HCV: vie di trasmissione
• Trasmissione parenterale (in passato la più frequente): (emofilici,
TD)
• Parenterale inapparente (attualmente la più frequente):
– VIA SESSUALE (rischio più basso rispetto a HBV e HIV)
– procedure invasive
– uso di cocaina endonasale
– trasmissione intra-familiare (rara, aumenta con il tempo di
esposizione)
– Trasmissione perinatale:
• Tasso medio di trasmissione: 6% (17% se la madre è anche
HIV+)
• Più probabile con alti livelli di HCV-RNA
• Indipendente da TC e allattamento
Prevalenza dell’infezione da HCV negli USA in
diversi gruppi di soggetti
Storia naturale dell’infezione
da HCV
Esposizione
Incubazione:15-180 giorni
Fase acuta (raramente sintomatica)
(85%)
Cronicizzazione
(15%)
Risoluzione
(80%)
(20%)
Cirrosi
Infezione stabile
75%
Progressione
lenta
25%
HCC
Insufficienza
epatica
HCV
Infezione da HCV:
risposta immune
via parenterale o
parenterale inapparente
Antigeni
virali
PMN
LISI DIRETTA
IFNa
DC
MO
NK
MHC-II
+
TCR
APOPTOSI
lisi cellulare
CD4+
MHC-I
TNFa
IFNg
TCR
TH2
Epatociti
TH1
CTL
++
+++
Kupffer
-TGFb
Infezione da HCV: risposta immune
Antigen presenting cells
Anticorpi
neutralizzanti
B
DC
B
MO
B
MHC-II
APOPTOSI
TCR
TH0
CD4+
Epatocita
IL-12
TCR
TCR
+
TH2
IL-10
IL-4
lisi cellulare
TH1
IL-2
IFNg
+
+
CTL
CTL
IFNg
TNFa
Infezione da HCV: risposta
immune
• Risposta umorale
– anticorpi neutralizzanti tipo-specifici: livelli
più elevati nei soggetti con infezione
cronica
• Risposta cellulare
– Linfociti T citotossici (CTL): necessari per il
controllo dell’infezione acuta; promuovono
il danno epatico nell’infezione cronica
– Linfociti CD4+ specifici: sostengono la
risposta CTL
Infezione da HCV:
risposta immune
via parenterale o
parenterale inapparente
Antigeni
virali
PMN
LISI DIRETTA
IFNa
DC
MO
NK
MHC-II
+
TCR
APOPTOSI
lisi cellulare
FIBROSI
CD4+
MHC-I
TNFa
IFNg
TCR
TH2
Epatociti
TH1
CTL
++
+++
Kupffer
-TGFb
FIBROSI
FIBROSI
Fibrogenesi in corso di
infezione da HCV
APOPTOSI + FIBROGENESI = EVOLUZIONE IN CIRROSI
Fas-L
Fas-R
Epatociti
ECM
CTL
ROS
L
I
S
I
++
TGFb
TNFa
IFNg
++
Kupffer
CD4+
TIMP
Patogenesi della fibrosi epatica
• Apoptosi delle cellule epatiche
• Stress ossidativo
• Iperproduzione di TGFb
• Attività delle cellule stellate
HCV sierologia
Andamento più frequente: CRONICIZZAZIONE
Fase acuta (asintom)
Titer
Ab anti-HCV
HCV-RNA
ALT
1-2 settimane
6-10 settimane
Time after Exposure
Markers: HCV-RNA +/Ab-antiHCV prima NEG, poi +
HCV sierologia
Andamento meno frequente: GUARIGIONE
Fase acuta (asintom)
Titer
Ab anti-HCV
HCV-RNA
ALT
1-2 settimane
10-15 settimane
Time after Exposure
Epatite C - Aspetti clinici
• Periodo di INCUBAZIONE
• ittero:
range:15-180 days
più sfumato in fase acuta
• età più colpita:
>60 anni
• epatite fulminante:
0.5% (eccezione:casi nosocomiali)
• Chronic infection:
85%
• Portatore asintomatico:
25%
• Latenza clinica:
10-20 anni
Standard of care
HCV Lifecycle
Receptor binding
and endocytosis
Transport
and release
Fusion and
uncoating
ER lumen
(+) RNA
LD
LD
Translation and
polyprotein
processing
Virion
assembly
LD
Membranous
web
ER lumen
Adapted from Manns MP, et al. Nat Rev Drug Discov. 2007;6:991-1000.
RNA replication
Porfira cutanea tarda in una
nostra paziente HIV/HCV
Treatment
She started erythro-apheresis
with a progressive decrease of
urine and plasma porphyrins
(from 5,13 mg/24h to 1,98 and
from 0,104 mg/L to 0,059
respectively)
6
5
HFE mutations :H63D
4
3
2
Plasma porphyrins mg/L
1
Urine porphyrins mg/L
0
1
2
3
4
5
6
7
Porphyria cutanea tarda
• Porphyria cutanea tarda ( PCT) is a iron-related
disorder that results from decreased activity of
hepatic uroporphyrinogen decarboxylase (UROD)
Porphyria cutanea tarda
• Porphyrins accumulate in the liver and are
then transported to the skin where they are
photoactivated by long-wave ultraviolet light,
forming activated oxygen species that cause
characteristic skin fragility and blistering.
• Cutaneous lesions are found on sun exposed
(the dorsa of the hands, face, neck and feet).
• HIV virions have been isolated from blister fluid of PTC/HIV-1
patients
Independent Predictors
of Liver-Related Death
Latest CD4 Cell Count (cells/µL)
16.06
<50
11.54
50-99
7.14
100-199
3.95
200-349
1.67
350-499
>500
2.01
HIV Acquisition via IDU
Hepatitis C Status
Multivariate analysis.
Not shown: Age per 5 years (1.32).
Negative
6.66
Positive
Hepatitis B Status
Negative
3.73
Positive
Weber R, et al. Arch Intern Med. 2006;166:1632-1641.
0.2
1.0
10
Relative Rate of Death
100
The probe induces an elastic
wave through the liver
FibroScan
The velocity of the wave is evaluated in a region located from 2.5
to 6.5 cm below the skin surface
2.5 cm
Explored volume
1 cm
LB: 1/50,000 of the liver
FibroScan: 1/500 of the liver
4 cm
“Standard of care” per il
trattamento dei pazienti HIV• Interferon alfa-2b/a + ribavirina per 12
mesi (genotipo 1 o cirrosi) o 6 mesi
• Pegylated interferon alfa-2b per 12 mesi
• Pegylated interferon alfa-2b/a + ribavirin
New HCV Agents –
Boceprevir and Telaprevir
• Boceprevir and Telaprevir, the 2 new oral
HCV protease inhibitors has phase 3 data
• Telaprevir (plus peg/rbv) 75% of patients
achieved SVR. Telaprevir is taken only for 12
weeks, peg/RBV is taken during the entire 48
weeks
• In mono infection with HCV 68% of patients in
studies had undetectable HCV viral load at 4
weeks and 58% at weeks 4 and 12 (212/363).
New HCV Agent- Telaprevir
• Relapse rates were low, 9%. Ontreatment virologic failure rates were only
3%. Patients with no, mild or portal
fibrosis had a 78% SVR. Patients with
cirrhosis with a 62% SVR, and for African
Am. the SVR was 62%
• Rash 56% with 6% a severe rash, on
average hemoglobin went down from
12.3 g/dL approx to 11 by week 8.
• It is expected that FDA will approve this
Pharmacokinetic Interactions
Between ARVs and Telaprevir
TVR Dose
TVR 750 mg tid
TVR 1250 mg tid
ARV
TVR AUC
TVR Cmin
ARV AUC
ARVCmin
ATV/r
0.80
(0.76-0.98)
0.85
(0.75-0.98)
1.17
(0.97-1.43)
1.85
(1.40-2.44)
DRV/r
0.65
(0.61-0.69)
0.68
(0.63-0.74)
0.60
(0.57-0.63)
0.58
(0.52-0.63)
FPV/r
0.68
(0.63-0.72)
0.70
(0.64-0.77)
0.53
(0.49-0.58)
0.44
(0.40-0.50)
LPV/r
0.46
(0.41-0.52)
0.48
(0.40-0.56)
1.06
(0.96-1.17)
1.14
(0.96-1.36)
0.82
(0.74-0.90)
0.90
(0.81-1.01)
1.10
(1.03-1.18)
1.17
(1.06-1.28)
0.85
(0.79-0.91)
0.89
(0.82-0.96)
1.10
(1.03-1.17)
1.06
(0.98-1.15)
EFV
TDF
TVR 1500 mg bid
0.82
(0.73-0.92)
0.75
(0.66-0.86)
EFV
TDF
0.80
(0.73-0.88)
Van Heeswijk R, et al. 18th CROI; Boston, MA; February 27-March 2, 2011. Abst. 119.
0.52
(0.42-0.64)
New HCV Agents - Boceprevir
• Patients received a 4-week lead in with peg/rbv
before starting boceprevir, hence, this will likely
be used this way.
• Patients with a 1 log or more decline in viral load
after the 4-week lead-in, 82% achieved SVR.
Patients with undetectable viral load at week 8,
90% achieved SVR.
• 49% had anemia, 1% discontinued, 13% dose
reduced due to anemia, 24% used EPO for
treatment of anemia.
New HCV Agents - Boceprevir
• RESPOND 2 study - The SVR were significantly higher
in patients randomized to receive boceprevir (56-75%)
compared to those who got peginterferon alfa-2b plus
ribavirin alone (40 %).
• Week 4 lead-in response predicted SVR: if a patient had
1 log or more decline in viral load at week 4, 73-79%
achieved SVR.
• The boceprevir treatment arm was associated with an
incremental risk of significant anemia compared to
peginterferon/ribavirin and epoetin alfa was more
frequently used.
New Information
• Lambda Interferon less side effects
• Genotype 1a vs 1b appears to matter: 1a appears to
respond less well to protease inhibitors than genotype 1b
because drug resistance appears more likely to emerge
with 1a
• Therapeutic approaches that will likely be more effective
for 1a include more potency, nucleosides like R7128 and
nucleotides like PSI7977 and PSI938 as they don't
develop resistance easily.
Indicazioni al trattamento con
IFN+RBV
Segni di epatite cronica a rischio di
progressione in cirrosi:
•
•
•
•
ALT elevate per più di sei mesi
HCV-RNA presente (analisi qualitativa/ quantitativa)
Fibrosi di grado 2 o 3 (periportale o bridging)
Grado moderato di infiammazione e necrosi epatica
Controindicazioni al trattamento
con IFN+RBV
Anemia (Hb<12-13 g/dl)
Emoglobinopatie
GB<1500
PLT<100.000
Gravidanza
Cirrosi scompensata
Patologie cardiovascolari
Epilessia
Malattie autoimmunitarie
Alcolismo
Diabete mellito scompensato Tossicodipendenza
Patologie psichiatriche gravi
Obiettivi della terapia anti-HCV
nei pazienti HIV• Obiettivi primari
– ERADICAZIONE di HCV
• Obiettivi secondari
– Ridurre la replicazione virale
– Ridurre l’infiammazione/necrosi epatica
– Rallentare la progressione della malattia
– Ridurre il rischio di epatocarcinoma
HCV Lifecycle and
STAT-C Targets
Receptor binding
and endocytosis
Transport
and release
Fusion and
uncoating
(+) RNA
ER lumen
LD
LD
Translation and
LD
NS3/4 protease
polyprotein
inhibitors
processing
Virion
assembly
Membranous
web
ER lumen
NS5B polymerase
RNA
replication
inhibitors
NS5A* inhibitors
*Role in HCV lifecycle not well defined
Adapted from Manns MP, et al. Nat Rev Drug Discov. 2007;6:991-1000.
New HCV Agents –
Boceprevir and Telaprevir
• Boceprevir and Telaprevir, the 2 new oral HCV
protease inhibitors has phase 3 data
• Telaprevir (plus peg/rbv) 75% of patients achieved
SVR. Telaprevir is taken only for 12 weeks,
peg/RBV is taken during the entire 48 weeks
• In mono infection with HCV 68% of patients in
studies had undetectable HCV viral load at 4 weeks
and 58% at weeks 4 and 12 (212/363).
New HCV Agent- Telaprevir
• Relapse rates were low, 9%. On-treatment
virologic failure rates were only 3%. Patients
with no, mild or portal fibrosis had a 78% SVR.
Patients with cirrhosis with a 62% SVR, and for
African Am. the SVR was 62%
• Rash 56% with 6% a severe rash, on average
hemoglobin went down from 12.3 g/dL approx
to 11 by week 8.
Remaining questions
• Why doesn’t IFN work in some patients?
• Is IFN necessary if you have two potent
antivirals?
• How many antiviral targets are needed
and how long is therapy needed?
• Target lipid metabolism?
Remaining questions
• Why doesn’t IFN work in some patients?
• Is IFN necessary if you have two potent
antivirals?
• How many antiviral targets are needed
and how long is therapy needed?
• Target lipid metabolism?
What is Pegylation?
• Covalent attachment of
polyethelene glycol to peptide
• Increases hydrodynamic size
• Prolonged circulation, delayed
renal clearance
• PegIntron (12kd, Schering),
Pegasys (40kd, Roche)
• Enzon pharmaceutical
– Adenosine deaminase
– Others: Neulasta (GCSF),
doxorubicin
Side Effects of PegIFN/Ribavirin
• Depression ranging
“Interferon Man”
from mild to
suicidality
• Irritability,
aggressive behavior
• Worsening of mania
• Fatigue
• Insomnia
• Myalgias, fever, flulike symptoms
• Hair loss
• Cytopenias
Slide courtesy Chia Wang
The importance of viral kinetics
8
Therapy
7
Log (10) HCV RNA
6
Non-response (NR)
5
Slow response with relapse
4
Early virologic response
(EVR)
3
Rapid virologic response
(RVR)
2
1
0
0
1
2
3
4
12
24
Time (wks)
Scott J and Gretch DR. JAMA 2007.
48
72
Kinetics and SVR
GT 1 (Pegasys + RVN)
Time
HCV RNA status
Wk 4
Neg
<2 log
<2 log
Any
Wk 12
Neg
Neg
>2 log
Any
Wk 24
Neg
Neg
Neg
Pos
SVR
91%
60%
43%
2%
Ferenci P. J Hepatol 2005; 43:425-33
Mechanism of Action: Interferon
HCV
HCV virions
Interferon alfa
Assembly
IFN receptors
JAK
Viral RNA
HCV replicative
complex
PKR
STAT
IRF9
ADA
ISG mRNA
ISGF3
ISRE
Hoofnagle J. NEJM
2006
PKR: inactivates
viral ptn translation
ADA: edits viral
RNA
STAT1
Adapted from
OAS
OAS: activates
antiviral RNAses
Effect of IFN-a/Ribavirin
Average HCV RNA level reduction (log IU/ml)
+0.5
0.0
-0.5
-1.0
-1.5
-2.0
-2.5
-3.0
-3.5
Group A: untreated
Group C: IFN-a3 MU tiw
Group D: IFN-a3 MU tiw + ribavirin 1.0-1.2 g qd
-4.0
-4.5
-5.0
0
2
4
6
8
10
12
14
16
18
20
Days
(Pawlotsky et al., Gastroenterology 2004;126:703-14) slide courtesy of JM Pawlotsky
22
24
26
28
Ribavirin Prevention of Relapse
% relapse (HCV RNA +)
Treatment
Follow-up
*
Continue ribavirin > wk
24
Stop ribavirin at wk 24
*
* p<0.05
*
24
30
*
*
36
48
52
Weeks of treatment
60
(Bronowicki et al., Gastroenterology 2006;131:1040-8) slide courtesy of JM Pawlotsky
72
Ribavirin’s Antiviral Mechanisms
• Direct inhibition of HCV RNA-dependent RNA
polymerase ?
• Depletion of intracellular GTP pools via IMPDH
inhibition ?
• RNA mutagenesis leading to "error catastrophe" ?
Ribavirin Antiviral Mechanisms
O
?
N
H N
2
HO
O
HO
N
N
?
?
OH
2’5’OAS
PKR
Mx
ADAR1
ISG20
ISG54
ISG56
…
Slide courtesy JM Pawlotsky
Future Therapies
•
•
•
•
Coming soon! (2011?)
Potent
Rapid antiviral resistance if used by itself
More side effects
HCV Life Cycle: Key Features
• Multiple proteins mediate HCV entry:
– CD81, Scavenger Receptor B1, Claudin 1, Occludin, Very Low
Density Lipoprotein Receptor
• Input HCV RNA is translated, a polyprotein is formed,
and individual viral proteins are released from
polyprotein by cellular and viral proteases
• HCV proteins associate with endoplasmic reticulum
membranes, the site of HCV replication
• Virion assembly occurs at lipid droplets
• HCV leaves the cell by hitching a ride on the
apolipoprotein B secretion pathway
• HCV life cycle is intimately tied with lipid metabolism
Slide courtesy S Polyak
HCV Variability
• RNA virus, RDRP lacks proof-reading
function
• Mutations arise during replication are
not corrected
– Genotypes
• genetically divergent HCV isolates that can be
grouped phylogenetically
– Quasispecies
• Highly related yet genetically distinct viruses
Slide courtesy S Polyak
HCV Drug Development
Phase of Development
Viral entry inhibitors
Hepatitis C immunoglobulin HCIg)
HCV-Ab 68 and Ab 65 (monoclonal Ab)
Preclinical
I
II
HCV RNA translation inhibitors
*
*
ISIS 14803 (antisense)
AVI – 4065 (antisense)
Heptazyme (ribozyme)
VGX-410C (small molecule IRES inhibitor)
TT 033 (siRNA)
Posttranslational processing inhibitors
NS3-4A serine proteinase inhibitors
BILN 2061
ITMN 191
VX-950
SCH 503034
ACH-806/GS-9132
HCV replication inhibitors
NS5B polymerase inhibitors
*
*
MK-0608
HCV-796
R1626
JTK-003
NM-283
XTL 2125
Cyclophilin B inhibitors
DEBIO-025
NIM 811
NS5A inhibitors
A-831, A-689
Helicase inhibitors
QU663
Recombinant Ab fragments
Virus assembly and release inhibitors
UT-231B (iminosugar-glucosidase inhibitor)
Celgosivir (glucosidase inhibitor)
(Pawlotsky JM, Chevaliez S, McHutchison JG, Gastroenterology 2007;132:1979-98)
*
*
*
III
IV
HCV Lifecycle
HCV Lifecycle
NS3 Protease Targets
Serine proteinase
catalytic site
(Pawlotsky JM, Chevaliez S, McHutchison JG, Gastroenterology 2007;132:1979-98)
NS3 Protease Inhibitors Having
Reached Clinical Development
• Peptidomimetic inhibitors
•
•
•
•
•
•
•
BILN 2061 (Boehringer-Ingelheim)
Telaprevir (VX950, Vertex & Tibotec)
Boceprevir (SCH503034, Schering-Plough)
TMC 435350 (Tibotec)
ITMN-191 (InterMune)
MK-7009 (Merck)
BI 201335 (Boehringer-Ingelheim
VX-950 Alone or in Combination
with Pegasys: Mean Viral Response
HCV RNA Change from
Baseline (Log10 IU/mL)
1
Baseline
0
-1
Pegasys + placebo
-2
-3
-4
VX-950
-5
VX-950 + Peg-IFN
-6
B
1
2
3
4
5 6 7 8 9 10 11 12 13 14
Study Time (In Days)
Reesink H et al. EASL. April 26-30, 2006.
Vienna, Austria. Abstract 737.
Slide courtesy Roche Medical Affairs
IFN sparing regimens?
• Roche: protease + polymerase inhibitor
(phase I)
• Merck/Schering: protease + polymerase
inhibitors
Remaining questions
• Why doesn’t IFN work in some patients?
• Is IFN necessary if you have two potent
antivirals?
• How many antiviral targets are needed
and how long is therapy needed?
• Target lipid metabolism?
Percentuale di coinfezione
per categorie a rischio
HIV+
8-40%
HIV+ omosessuali
4-8%
HIV+ emofilici
60-85%
HIV+ tossicodipendenti
52-90%
Genotipo 1b
Genotipo 1a e 3a
Storia naturale dell’infezione
da HCV
Esposizione
(fase acuta)
(85%)
Cronicizzazione
(15%)
(80%)
(20%)
Risoluzione
Infezione stabile
Cirrosi
75%
25%
Progressione
lenta
HCC
Insufficienza
epatica
Storia naturale dell’infezione
da HIV
Esposizione
(fase acuta)
Cronicizzazione
??
Risoluzione
99%
1-10%
Infezione
stabile?
80%
Progressione
lenta
AIDS
10%
Progressione
rapida
HIV
HIV
..
HCV
HCV
HIV/HCV
HIV
HIV/HCV
HAART
HAART
HIV
HCV
HIV/HCV+
doppia terapia
HAART
HIV
IFN+RBV
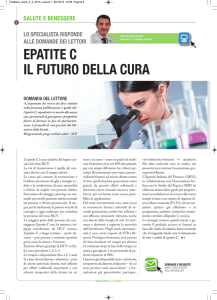
Ipertransaminasemia:percorso diagnostico
VN=30-50 UI/ml
AUMENTO TRANSAMINASI
> 10 volte VN (600-2500)
< 10 volte VN (70-500)
Sospetta EPATITE ACUTA
sospetta EPATITE CRONICA
I livello:
•IgM anti-HAV
+
•HBsAg/anti-HBc IgM
-
•anti-HEV IgM
-
I livello:
Ep acuta B
•HBsAg/HBeAg Ep cronica B
•Anti-HCV
++
Anti-HDV IgM
II livello:
•HCV-RNA
++
+
+
+
Ep acuta A
Altre ipotesi:
Ep acuta E
alcoolica
tossica
Ep acuta C
Altre ipotesi: TOSSICA, AUTOIMMUNE
altri virus
Ab antiVCA-IgM, Ab anti CMV IgM
-
autoimmune
Wilson
+
emocromatosi
Ep acuta EBV, CMV
Ep cronica C