Primary Lymphoma of the Central Nervous System in
Two Children with Acquired Immune Deficiency Syndrome
ANNAROSA DEL MISTRO, M.D., ANNAMARIA LAVERDA, M.D., FIORELLA CALABRESE, M.D.,
MAURIZIO DE MARTINO, M.D., GIUSEPPE CALABRI, M.D., PAOLA COGO, M.D., PIERO COCCHI, M.D.,
EMMA D'ANDREA, M.D., ANITA DE ROSSI, PH.D., CARLO GIAQUINTO, M.D., RENZO GIORDANO, M.D.,
ROSSELLA M. NIERI, M.D., GIUSEPPE SALVI, M.D., NATALE PENNELLI, M.D., AND LUIGI CHIECO-BIANCHI, M.D.
Istituto di Oncologia, Centro Interuniversitario per la Ricerca
sul Cancro (CIRC), Dipartimento di Pediatria, Istituto di
Anatomia Patologica, Universita di Padova, and Dipartimento
di Pediatria, Universita di Firenze, Italy
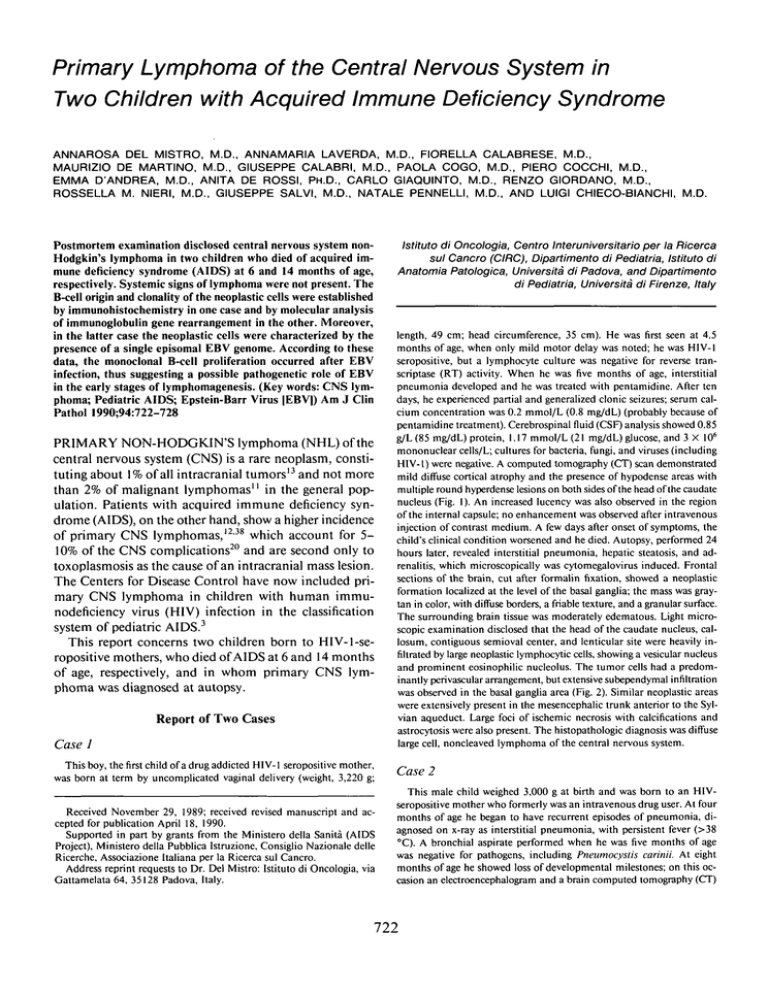
Postmortem examination disclosed central nervous system nonHodgkin's lymphoma in two children who died of acquired immune deficiency syndrome (AIDS) at 6 and 14 months of age,
respectively. Systemic signs of lymphoma were not present. The
B-cell origin and clonality of the neoplastic cells were established
by immunohistochemistry in one case and by molecular analysis
of immunoglobulin gene rearrangement in the other. Moreover,
in the latter case the neoplastic cells were characterized by the
presence of a single episomal EBV genome. According to these
data, the monoclonal B-cell proliferation occurred after EBV
infection, thus suggesting a possible pathogenetic role of EBV
in the early stages of lymphomagenesis. (Key words: CNS lymphoma; Pediatric AIDS; Epstein-Barr Virus [EBV]) Am J Clin
Pathol 1990;94:722-728
PRIMARY NON-HODGKIN'S lymphoma (NHL) of the
central nervous system (CNS) is a rare neoplasm, constituting about 1% of all intracranial tumors' 3 and not more
than 2% of malignant lymphomas'' in the general population. Patients with acquired immune deficiency syndrome (AIDS), on the other hand, show a higher incidence
of primary CNS lymphomas, 12 ' 38 which account for 5 10% of the CNS complications 20 and are second only to
toxoplasmosis as the cause of an intracranial mass lesion.
The Centers for Disease Control have now included primary CNS lymphoma in children with human immunodeficiency virus (HIV) infection in the classification
system of pediatric AIDS. 3
This report concerns two children born to HIV-1-seropositive mothers, who died of AIDS at 6 and 14 months
of age, respectively, and in whom primary CNS lymphoma was diagnosed at autopsy.
Report of Two Cases
Case J
This boy, thefirstchild of a drug addicted HIV-1 seropositive mother,
was born at term by uncomplicated vaginal delivery (weight, 3,220 g;
Received November 29, 1989; received revised manuscript and accepted for publication April 18, 1990.
Supported in part by grants from the Ministero della Sanita (AIDS
Project), Ministero della Pubblica Istruzione, Consiglio Nazionale delle
Ricerche, Associazione Italiana per la Ricerca sul Cancro.
Address reprint requests to Dr. Del Mistro: Istituto di Oncologia, via
Gattamelata 64, 35128 Padova, Italy.
length, 49 cm; head circumference, 35 cm). He was first seen at 4.5
months of age, when only mild motor delay was noted; he was HIV-1
seropositive, but a lymphocyte culture was negative for reverse transcriptase (RT) activity. When he was five months of age, interstitial
pneumonia developed and he was treated with pentamidine. After ten
days, he experienced partial and generalized clonic seizures; serum calcium concentration was 0.2 mmol/L (0.8 mg/dL) (probably because of
pentamidine treatment). Cerebrospinalfluid(CSF) analysis showed 0.85
g/L (85 mg/dL) protein, 1.17 mmol/L (21 mg/dL) glucose, and 3 X 106
mononuclear cells/L; cultures for bacteria, fungi, and viruses (including
HIV-1) were negative. A computed tomography (CT) scan demonstrated
mild diffuse cortical atrophy and the presence of hypodense areas with
multiple round hyperdense lesions on both sides of the head of the caudate
nucleus (Fig. 1). An increased lucency was also observed in the region
of the internal capsule; no enhancement was observed after intravenous
injection of contrast medium. A few days after onset of symptoms, the
child's clinical condition worsened and he died. Autopsy, performed 24
hours later, revealed interstitial pneumonia, hepatic steatosis, and adrenalitis, which microscopically was cytomegalovirus induced. Frontal
sections of the brain, cut after formalin fixation, showed a neoplastic
formation localized at the level of the basal ganglia; the mass was graytan in color, with diffuse borders, a friable texture, and a granular surface.
The surrounding brain tissue was moderately edematous. Light microscopic examination disclosed that the head of the caudate nucleus, callosum, contiguous semioval center, and lenticular site were heavily infiltrated by large neoplastic lymphocytic cells, showing a vesicular nucleus
and prominent eosinophilic nucleolus. The tumor cells had a predominantly perivascular arrangement, but extensive subependymal infiltration
was observed in the basal ganglia area (Fig. 2). Similar neoplastic areas
were extensively present in the mesencephalic trunk anterior to the Sylvian aqueduct. Large foci of ischemic necrosis with calcifications and
astrocytosis were also present. The histopathologic diagnosis was diffuse
large cell, noncleaved lymphoma of the central nervous system.
Case 2
This male child weighed 3,000 g at birth and was born to an HIVseropositive mother who formerly was an intravenous drug user. At four
months of age he began to have recurrent episodes of pneumonia, diagnosed on x-ray as interstitial pneumonia, with persistent fever (>38
°C). A bronchial aspirate performed when he was five months of age
was negative for pathogens, including Pneumocystis carinii. At eight
months of age he showed loss of developmental milestones; on this occasion an electroencephalogram and a brain computed tomography (CT)
722
Vol. 94 • No. 6
BRAIN LYMPHOMA IN TWO CHILDREN WITH AIDS
723
20. The search for viral antigens in serum and CSF was
performed by using the HIV p24 enzyme-linked immunosorbent assay (ELISA) system (DuPont), according to
the manufacturer's instructions. In case 1, anti-EBV IgG
presence was determined with the use of a radioimmunoassay (RIA). In case 2, a search for IgM anti-EBV capsid
antigen was performed with an immunofluorescence
assay.
As reported in Table 1, anti-HIV-1 Abs were present
in both serum samples but not in CSF, whereas p24 Ag
was detected only in case 2. Abs against EBV capsid proteins were present in serum but not CSF of case 1, whereas
serum of case 2 was negative for anti-EBV IgM. Finally,
an inverted CD4+/CD8+ lymphocyte ratio was observed
in both children.
DNA Extraction and Molecular Analysis
FIG. 1. Case 1. Computerized tomography. Presence of hypodense
areas with bilateral multiple round hyperdense lesions at the head of the
caudate nucleus.
scan were negative. After four more months, he had right palpebral ptosis
and left hemiparesis. A second brain CT scan showed a mass abutting
the frontal horn of the right lateral ventricle and the right side of the
capsule (Fig. 3). Funduscopic examination revealed no abnormalities;
the child's condition precluded brain biopsy and CSF examination. One
month later, a third CT scan showed that the intracranial mass had
grown and now involved the surrounding structures; the child died suddenly at 14 months of age.
Autopsy revealed a large tumor mass involving the right hemisphere,
basal nuclei, and semioval center. On histologic examination, this tumor
consisted of medium-sized round cells with a big, bulky nucleus, and
multiple nucleoli in some cells: the large cytoplasm contained abundant
periodic acid-Schiff(PAS) -positive material. Giant multinucleated cells
and foamy macrophages were also present, as well as many typical and
atypical mitoticfigures.The histopathologic diagnosis was central nervous
system lymphoma. No signs of systemic lymphoma were found.
Serologic Studies
Serum samples were screened by an immunoenzymatic
assay for the presence of antibodies (Abs) against human
retroviruses HIV-1 (DuPont, Wilmington, DE; Abbott
Laboratories, North Chicago, IL), HIV-2 (Midy Pasteur,
Diagnostics Pasteur, Marnes la Coquette, France), and
HTLV-I (DuPont); positive results were confirmed by
Western blot (WB) analysis (DuPont). CSF from patient
1 was available and was analyzed for Abs against HIV-1
by commercial WB, with the use of a final dilution of 1:
DNA was extracted from both CNS lymphoma specimens. Only formalin-fixed, paraffin-embedded material
was available in case 1, and extraction was performed
according to published procedures6'9 with slight modifications. Briefly, 5-^m sections were cut, deparaffinized,
rehydrated, and digested with 1 mg/mL Proteinase K.®
(Boehringer Mannheim, Mannheim, West Germany) and
1% (weight/volume [w/v]) sodium dodecyl sulfate (SDS)
for 72 hours at 37 °C; DNA was extracted with phenolchloroform, precipitated with sodium acetate/cold
ethanol, and recovered by centrifugation. Only low molecular weight DNA was obtained; this was analyzed by
dot blot for the presence of the following viral sequences:
EBV, with the use of the pSL9 probe26; HTLV-I, with the
use of the pMT2/64 probe (kindly provided by Dr. R. C.
Gallo, National Institutes of Health, Bethesda, MD); HIV1, with the use of the pBH10-R3 probe32; and HHV-6,
with the use of the pZVH 14 probe.14 A probe representing
only plasmid sequences (pSP64 and pBR322) was used
as a negative control. Positive samples were included in
all analyses. No viral sequences were detected, and a negative result was also obtained with the use of the plasmid
probe (Fig. 4).
In case 2, freshly cut frozen material was homogenized
and digested with 0.1 mg/mL Proteinase K and 0.5%
(w/v) SDS for 20 hours at room temperature; DNA was
extracted and precipitated as above and spooled out with
a glass rod. The high molecular weight DNA obtained
was then digested with restriction enzymes BamHI and
EcoRI, electrophoresed through an 0.8% (w/v) agarose
gel, and transferred to a NYTRAN® membrane
(Schleicher and Schuell, Keene, NH) according to the
method of Southern.34 The filter was hybridized with the
c-myc pMC41 3RC probe (1.4-kb Clal-EcoRI fragment)4
for gene rearrangements, and the Xho 1.9-kb EBV
fragment5 for analysis of EBV genome dominance, as well
724
DEL MISTRO ET AL.
A.J.C.P. • December 1990
FIG. 2. Case 1. Histologic sections of the tumor mass. {A, B). Perivascular collection of neoplastic cells. Hematoxylin and eosin (A) (X195), (B)
(X380). (C, D). Subependymal infiltration. Hematoxylin and eosin (C) (X195), (£>) (X380).
Vol. 94 • No. 6
725
BRAIN LYMPHOMA IN TWO CHILDREN WITH AIDS
FIG. 3. Case 2. CT scan: right extensive
mass involving the basal nuclei, characterized by uneven density, causing important
dislocation and compression of the lateral
and the third ventricles.
as with the immunoglobulin JH (3.3-kb EcoRI-Hindlll
fragment)29 and the T-cell receptor (TCR) beta cDNA
(0.77-kb PstI fragment)37 probes for genotypic analysis.
As shown in Figure 5A, hybridization with the Xho 1.9kb EBV fragment disclosed only one EBV-specific band,
due to the persistence of a single episomal EBV genome
in both the lymphoma DNA and the well-characterized
Raji cell line DNA, 28 after BamHI digestion. The EBVspecific 3.1 -kb band was detected with the use of the pSL9
homologous probe on the same filter. The equal intensity
of both IgH-rearranged bands also suggested that a single
B-cell clone carrying rearrangements of both alleles was
present in the tumor and coexisted in almost equal proportions with nonrearranged cells (Fig. 5B). Finally, the
germline configuration observed with the use of the TCR
beta probe (Fig. 5C) confirmed the B-cell lineage fidelity
of the tumor. No rearrangement of c-mycgene was present
(data not shown). The lymphoma DNA was negative for
all other viruses tested (HI V-1, HTLV-I, HHV-6), as well
as for plasmid sequences (Fig. 4). Thus, the molecular
diagnosis was EBV-positive B-cell lymphoma of the CNS.
Immunohistochemistry
Formalin-fixed, paraffin-embedded serial sections of the
CNS lymphoma specimens were stained with monoclonal
antibodies (MoAbs) MTl, MT2, MB1, MB2 (Clonab
Biotest, Dreieich, West Germany), UCHL1, and 4KB5,
as well as Abs for intracytoplasmic kappa and lambda
light chain immunoglobulins (DAKOPATTS, Glostrup,
Denmark), with the use of the peroxidase-antiperoxidase
(PAP) technique. 35
In case 1 the tumor cells were strongly positive with
MoAb MT2 and for intracytoplasmic lambda light chain
immunoglobulins; slightly positive with the MoAbs MB1,
MB2, and 4KB5; and negative with MoAbs MTl and
UCHL1 and for intracytoplasmic kappa light chain immunoglobulins. These results indicate a monoclonal Bcell lineage of the tumor cells.
In case 2, immunoperoxidase analysis performed on
formalin-fixed paraffin-embedded sections with MTl,
MT2, MB1, and MB2 MoAbs proved technically unsatisfactory.
Table 1. Laboratory Findings
Blood
CSF
HIV-1
Case
no.
Ab
1
2
Pos
Pos
HIV-1
Ag
HTLV-I
Ab
HIV-2
Ab
EBV
Ab
CD4/CD8
ratio
Ab
Ag
EBV
Ab
Neg
Pos
Neg
Neg
Neg
Neg
Pos
Neg
0.5
0.2
Neg
ND
Neg
ND
Neg
ND
CSF = cerebrospinal fluid; Ab = antibody; Ag = p24 antigen; ND = not done.
DEL MISTRO ET AL.
726
A.J.C.P. • December 1990
B
C +
C -
&
•
*
<
&
IWJ.
Case
1
Case
2
*
•<!.:
FIG. 4. Dot blot analysis for presence of viral sequences in the lymphoma specimens. Tumor DNA from case 1 (2 ng) and case 2 (8 ^g) was loaded
on nitrocellulosefiltersthrough a Minifold II apparatus (Schleicher & Schuell, Keene, NH). Two micrograms of DNA derived from Raji (A), H9 III
(B), MT2 (C) cells, and 2 ng of pZVH14 (D) and pSP64 (E) plasmid DNA were used as positive controls (C+) for EBV, HIV-1, HTLV-I, HHV-6,
and pSP64 specific sequences, respectively. Four micrograms of H9 cell DNA were used as negative control (C—) in all cases.
Discussion
Primary intracranial lymphoma is uncommon in any
age group, but it is especially rare during childhood,30
where it occurs almost exclusively in children with inherited or acquired immune deficiency syndromes.22 Primary CNS lymphoma in adults with AIDS has been repeatedly observed,18'3338 but very few cases of AIDS-related lymphoma have been reported in children. 81516 - 23
In the two cases described above, primary CNS lymphoma
without involvement of other sites was diagnosed at autopsy in two male infants (6 and 14 months old, respectively), both born to HIV-1 seropositive mothers. Clinical
and tomographic signs of a CNS lesion were present in
both cases; lymphoma and opportunistic infections were
considered, but only histologic examination enabled a
conclusive diagnosis.
As commonly observed in most of the lymphomas occurring in patients with AIDS,7 the tumor cells in these
two CNS lymphomas were of B-cell origin. A survey of
lymphomas occurring in patients with primary immune
deficiencies (notably Wiskott-Aldrich syndrome) as well
as in transplant recipients showed that many were of Bcell origin, and in 33-52% of the cases there was a predilection for the CNS. 25 To explain this propensity for
CNS localization, it was advanced that the brain is an
immunologically "privileged" site, where neoplastic cells
can thrive in an environment of impaired immunosurveillance.31
The presence of monotypic light-chain immunoglobulin in case 1 and the pattern of IgH gene rearrangement
and EBV genome dominance in case 2 indicate clonality
of the neoplastic B-cell population. This finding, together
with the short latency and the rapid disease progression,
suggests that the early steps leading to tumor development
might have occurred during the prenatal period. Although
tumor monoclonality is not the rule in adult patients with
AIDS, because many B-cell non-Hodgkin's lymphomas
contained multiple B-cell clones,18 a recent report produced evidence of monoclonality in three lymphoma cases
associated with both EBV infection and c-myc germline
configuration.19
The pathogenesis of AIDS-NHL is not yet understood,
and different mechanisms, such as oncogene activation24,36
and viral oncogenicity,21 were proposed. Although
monoclonal gene rearrangements of the c-myc locus were
frequently demonstrated in AIDS-related NHL, 36 c-myc
activation apparently was not involved in the pathogenesis
of the tumor we tested or in those associated with EBV
infection reported by Knowles and associates.19 Whether
EBV has a primary role in lymphomagenesis or secondarily infects malignant cells in patients with inherited or
acquired immune deficiencies has not yet been established.27 The clonality observed in case 2, demonstrated
also by EBV genome dominance, would favor the former
hypothesis: an EBV-driven polyclonal B-cell expansion
could give rise, through as yet unknown mechanisms apparently not involving c-myc rearrangements, to a cell
clone against which the immune-deficient patient is unable to respond.10 Indeed, an impaired response to EBV
infection was demonstrated in HIV-infected patients2;
moreover, in an infant with AIDS,16 Abs against viral
capsid antigen were first demonstrated only four months
after detection of EBV DNA in a lymph node explanted
when the child was eight months old.
DNA sequences of other viruses possibly involved in
the pathogenesis of NHL, such as HIV-1, HTLV-I, and
HHV-6, were not detected in the tumor of both cases
Vol. 94 • No. 6
727
BRAIN LYMPHOMA IN TWO CHILDREN WITH AIDS
a
E
o
I
5
Kb
OC
%
>I
J
eg
»
«
-<
£
a
E
IO
t
S 2
Kb
Kb
9.4 >
9.4>
—
W
23.1 >
23.11>^^
23.1 >\
I
\
tl
9.4 > |
67>
6.7t>
6.7>
4.4>
•
•
2.3>
2.0>
digestion
prob*
I
Bam HI
Xhol9
p8L9
Eco R1
BimHI
JH
Ec« «1
TCI
.
• • « N1
A
B
FIG. 5. Southern blot analysis of high molecular weight DNA extracted from lymphomatous tissue of case 2. (A). Bam-Hl-digested DNA was
hybridized with two 32P-labeled EBV-specific probes, representing the EBV BamHl K fragment (pSL9) and the EcoRI-D unique sequences of EBV
left terminus (Xho 1.9). Ten micrograms of DNA were loaded in each lane. The lymphoblastoid cell line Raji contains about 80 genome equivalents
per cell. (B). EcoRI- and BamHI-digested DNA was hybridized with a 32P-labeled JH probe. A germline pattern for the K.562 cell line DNA, and a
rearranged pattern for the lymphoma tissue can be observed. (C). DNA as in (B) was hybridized with a 32P-labeled TCR beta probe. A germline
pattern can be observed in both K562 cell and lymphoma DNA.
(Fig. 4). A direct role of HIV-1 in AIDS-NHL is not very
likely because proviral DNA has never been found in the
neoplastic cells; however, the virus could act indirectly,
either by chronically stimulating the B-cell compartment
or by causing immunosuppression, or both. In fact, the
high frequency of spontaneously activated specific B-cells
observed during HIV infection' closely resembles the
situation present in patients shortly after any immunization17; this phenomenon, however, is not transitory
in HIV-infected patients, but long lasting, possibly leading
to lymphoma development.
Acknowledgments. The authors thank Dr. Flossie Wong-Staal (National
Institutes of Health, Bethesda, MD) for providing probes pBH10-R3,
pMT2/64, and pZVH14; and Patricia Segato for helpful discussion in
preparing the manuscript.
References
1. Amadori A, Zamarchi R, Ciminale V, et al. HIV-l-specific B-cell
activation. A major constituent of spontaneous B-cell activation
during HIV-1 infection. J Immunol 1989;143:2146-2152.
Birx DL, Redfield RR, Tosato G. Defective regulation of EpsteinBarr virus infection in patients with AIDS or ARC. N Engl J Med
1986;314:874-879.
Centers for Disease Control. Classification system for human immunodeficiency virus (HIV) infection in children under 13 years
of age. MMWR 1987;36:226-235.
Dalla-Favera R, Martinotti S, Gallo RC. Erikson J, Croce CM.
Translocation and rearrangements of the c-myc oncogene locus
in human undifferentiated B-cell lymphomas. Science 1983:219:
963-967.
Dambaugh T, Beisel C, Hummel M, et al. Epstein-Barr virus (B958) DNA VII: molecular cloning and detailed mapping. Proc Natl
Acad Sci USA 1980;77:2999-3003.
Dubeau L, Chandler LA, Gralow JR, Nichols PW, Jones PA. Southern blot analysis of DNA extracted from formalin-fixed pathology
specimens. Cancer Res 1986;46:2964-2969.
Egerter DA, Beckstead JH. Malignant lymphomas in the acquired
immunodeficiency syndrome. Additional evidence for a B-cell
origin. Arch Pathol Lab Med 1988; 112:602-606.
Epstein LG, DiCarlo FJ, Joshi VV, et al. Primary lymphoma of the
central nervous system in children with acquired immunodeficiency syndrome. Pediatrics 1988;82:355-363.
Goelz SE, Hamilton SR, Vogelstein B. Purification of DNA from
formaldehyde fixed and paraffin embedded human tissue.
Biochem Biophys Res Commun 1985; 130:118-126.
10. Henle W, Henle G. Epstein-Barr virus-specific serology in immunologically compromised individuals. Cancer Res 1981:41:4222—
4225.
728
DEL MISTRO ET AL.
11. Henry JM, Heffner RR, Dillard SH, Earle KM, Davis RL. Primary
malignant lymphomas of the central nervous system. Cancer
1974;34:1293-1302.
12. Ioachim HL, Cooper MC, Hellman GC. Lymphoma in men at high
risk for acquired immune deficiency syndrome (AIDS). A study
of 21 cases. Cancer 1985;56:2831-2842.
13. Jellinger K, Radaskiewicz TH, Slowik F. Primary malignant lymphomas of the central nervous system in man. Acta Neuropathol
(Berl) 1975;(suppl6):95-102.
14. Josephs SF, Salahuddin SZ, Ablashi DV, Schachter F, Wong-Staal
F, Gallo RC. Genomic analysis of the human B-lymphotropic
virus (HBLV). Science 1986;234:601-603.
15. Kato T, Hirano A, Llena JF, Dembitzer HM. Neuropathology of
acquired immune deficiency syndrome (AIDS) in 53 autopsy cases
with particular emphasis on microglial nodules and multinucleated giant cells. Acta Neuropathol (Berl) 1987;73:287-294.
16. Katz BZ, Andiman WA, Eastman R, Martin K, Miller G. Infection
with two genotypes of Epstein-Barr virus in an infant with AIDS
and lymphoma of the central nervous system. J Infect Dis
1986;153:601-604.
17. Kehrl JH, Fauci AS. Identification, purification and characterization
of antigen-activated and antigen-specific human B lymphocytes.
J Exp Med 1983;157:1692-1697.
18. Knowles DM, Chamulak GA, Subar M, et al. Lymphoid neoplasia
associated with the acquired immunodeficiency syndrome (AIDS).
The New York University Medical Center Experience with 105
patients (1981-1986). Ann Intern Med 1988;108:744-753.
19. Knowles DM, Inghirami G, Ubriaco A, Dalla Favera R. Molecular
genetic analysis of three AIDS-associated neoplasms of uncertain
lineage demonstrates their B-cell derivation and the possible
pathogenetic role of the Epstein-Barr virus. Blood 1989;73:792799.
20. Koppel BS, Wormser GP, Tuchman AJ, Maayan S, Hewlett D,
Daras M. Central nervous system involvement in patients with
acquired immune deficiency syndrome (AIDS). Acta Neurol
Scand 1985;71:337-353.
21. Levine AM. Reactive and neoplastic lymphoproliferative disorders
and other miscellaneous cancers associated with HIV infection.
In: DeVita VT, Hellman S, Rosenberg SA, eds. AIDS: etiology,
diagnosis, treatment, and prevention. 2nd ed. New York: JB Lippincott, 1988:263-275.
22. Link MP. Non-Hodgkin's lymphomas in children. PediatrClin North
Am 1985;32:699-720.
23. Pahwa S, Kaplan M, Fikrig S, et al. Spectrum of human T-cell lymphotropic virus type III infection in children. Recognition of
symptomatic, asymptomatic, and seronegative patients. JAMA
1986;255:2299-2305.
A.J.C.P. • December 1990
24. Pelicci PG, Knowles DM, Magrath I, Dalla-Favera R. Chromosomal
breakpoints and structural alterations of the c-myc locus differ in
endemic and sporadic forms of Burkitt lymphoma. Proc Natl
Acad Sci USA 1986,83:2984-2988.
25. Penn I. The occurrence of malignant tumors in immunosuppressed
states. Prog Allergy 1986;37:259-300.
26. Polack A, Hartl G, Zimber U, et al. A complete set of overlapping
cosmid clones of M-ABA virus derived from nasopharyngeal carcinoma and its similarity to other Epstein-Barr virus isolates. Gene
1984;27:279-288.
27. Purtilo DT. Immune deficiency predisposing to Epstein-Barr virusinduced lymphoproliferative syndrome as a model. Adv Cancer
Res 1981;34:279-312.
28. Raab-Traub N, Flynn K. The structure of the termini of the EpsteinBarr virus as a marker of clonal cellular proliferation. Cell 1986:47:
883-889.
29. Ravetch JV, Siebenlist U, Korsmeyer S, Waldmann T, Leder P.
Structure of the human immunoglobulin n locus: characterization
of embryonic and rearranged J and D genes. Cell 1981;27:583589.
30. Schiffer D, Chio' A, Giordana MT, et al. Primary lymphomas of
the brain: a clinico-pathologic review of 37 cases. Tumori 1987;73:
585-592.
31. Schneck SA, Penn I. De novo cerebral neoplasms in renal transplant
recipients. Lancet 1971;1:983-984.
32. Shaw GM, Hahn BH, Arya SK, Groopman JE, Gallo RC, WongStaal F. Molecular characterization of human T-cell leukemia
(lymphotropic) virus type III in the acquired immune deficiency
syndrome. Science 1984;226:1165-1171.
33. Snider WD, Simpson DM, Aronyk KE, Nielsen SL. Primary lymphoma of the nervous system associated with acquired immunedeficiency syndrome. N Engl J Med 1983,308:45.
34. Southern EM. Detection of specific sequences among fragments
separated by gel electrophoresis. J Mol Biol 1975,98:503-517.
35. Sternberger LA. The unlabelled antibody peroxidase-anti-peroxidase
method. In: Sternberger LA, ed. Immunocytochemistry. 2nd ed.
New York: John Wiley and Sons, 1979:104-120.
36. Subar M, Neri A, Inghirami G, Knowles DM, Dalla-Favera R. Frequent c-myc oncogene activation and infrequent presence of Epstein-Barr virus genome in AIDS-associated lymphoma. Blood
1988;72:667-671.
37. Yoshikai Y, Anatoniou D, Clark SP, et al. Sequence and expression
of transcripts of the human T-cell receptor B-chain genes. Nature
1984;312:521-524.
38. Ziegler JL, Beckstead JA, Volberding PA, et al. Non-Hodgkin's
lymphoma in 90 homosexual men. Relation to generalized
lymphadenopathy and the acquired immunodeficiency syndrome.
N Engl J Med 1984;311:565-570.